Health care financing
advertisement
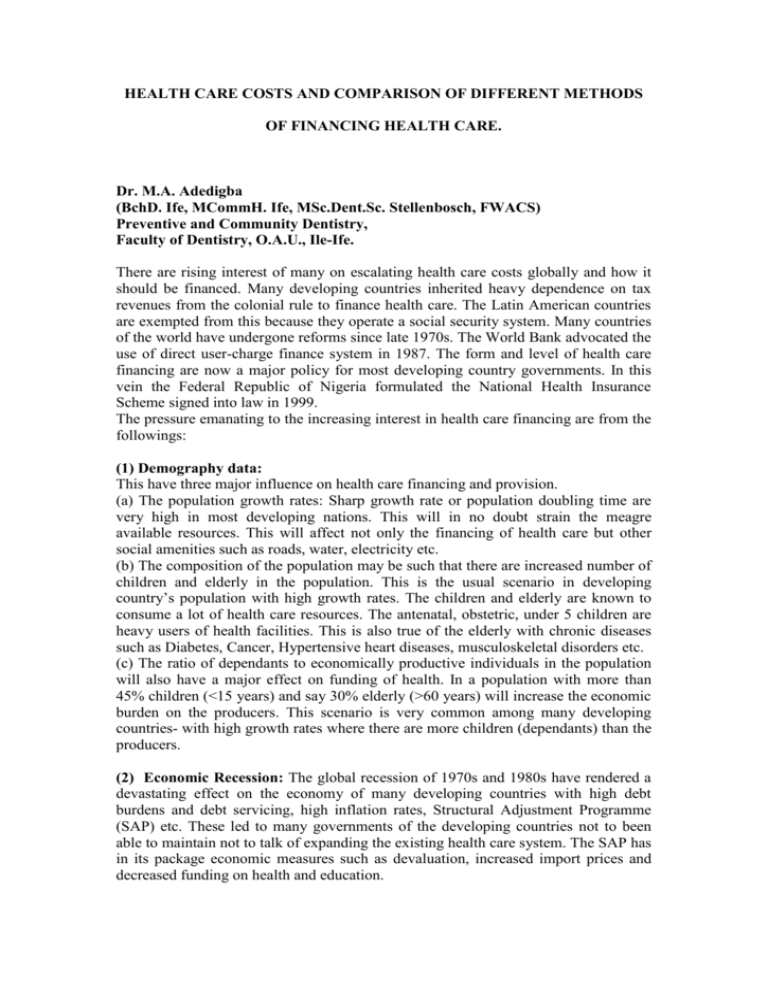
HEALTH CARE COSTS AND COMPARISON OF DIFFERENT METHODS OF FINANCING HEALTH CARE. Dr. M.A. Adedigba (BchD. Ife, MCommH. Ife, MSc.Dent.Sc. Stellenbosch, FWACS) Preventive and Community Dentistry, Faculty of Dentistry, O.A.U., Ile-Ife. There are rising interest of many on escalating health care costs globally and how it should be financed. Many developing countries inherited heavy dependence on tax revenues from the colonial rule to finance health care. The Latin American countries are exempted from this because they operate a social security system. Many countries of the world have undergone reforms since late 1970s. The World Bank advocated the use of direct user-charge finance system in 1987. The form and level of health care financing are now a major policy for most developing country governments. In this vein the Federal Republic of Nigeria formulated the National Health Insurance Scheme signed into law in 1999. The pressure emanating to the increasing interest in health care financing are from the followings: (1) Demography data: This have three major influence on health care financing and provision. (a) The population growth rates: Sharp growth rate or population doubling time are very high in most developing nations. This will in no doubt strain the meagre available resources. This will affect not only the financing of health care but other social amenities such as roads, water, electricity etc. (b) The composition of the population may be such that there are increased number of children and elderly in the population. This is the usual scenario in developing country’s population with high growth rates. The children and elderly are known to consume a lot of health care resources. The antenatal, obstetric, under 5 children are heavy users of health facilities. This is also true of the elderly with chronic diseases such as Diabetes, Cancer, Hypertensive heart diseases, musculoskeletal disorders etc. (c) The ratio of dependants to economically productive individuals in the population will also have a major effect on funding of health. In a population with more than 45% children (<15 years) and say 30% elderly (>60 years) will increase the economic burden on the producers. This scenario is very common among many developing countries- with high growth rates where there are more children (dependants) than the producers. (2) Economic Recession: The global recession of 1970s and 1980s have rendered a devastating effect on the economy of many developing countries with high debt burdens and debt servicing, high inflation rates, Structural Adjustment Programme (SAP) etc. These led to many governments of the developing countries not to been able to maintain not to talk of expanding the existing health care system. The SAP has in its package economic measures such as devaluation, increased import prices and decreased funding on health and education. (3) Expectations from health care: There are increasing pressures from the population on the expectations on health care. Majority will like to enjoy the health care facilities similarly available in the first world countries. This is usually associated with the use of high Tech equipment which most of the time are imported. (4) Drive for Equity: Many segments/regions of most developing countries are underserved with health care facilities. Also, majority have access only to basic but limited health care. One of the principles of primary health care is to improve coverage; this is contrary to the sophisticated health care facilities needed by the middle class in the urban areas. (5) Changing disease pattern: As the income of an individual rises there is a change in the pattern of the disease to be observed. The diseases associated with poverty are rapidly disappearing leaving the room for those of the affluence. Major health problems in developing countries are preventable and are relatively cheap to deal with when compared with that of the advanced countries (Heart diseases, Cancer, Diabetes etc). The change in disease pattern associated with change in social status will invariably lead to an increasing cost for health care of those diseases. Also, when new diseases are being discovered (e.g. HIV/AIDS, SAS, Bird flu) or that previous diseases that are not medically diagnosable based on the available knowledge then, are now possible through the use of high sophisticated and expensive medical equipments. HOW DO WE INCREASE EFFECTIVE RESOURCE LEVEL IN HEALTH CARE FINANCING? As a result of the afore-mentioned factors affecting health care funding, there is a need to look into what areas and measures that can be introduced to improve health care financing. The followings are areas to look into with the hope of improving resources to finance health care: (1) Efficiency: The existing services should be look into with the hope of improving them. This can best be done by: (a) Appraisal: cost-effectiveness analysis may suggest alternative approaches to specific health problems that are better or more effective. (b) Contracting out: Some of the services can be contracted out to individuals and companies to improve effectiveness e.g. catering, cleaning, security services etc. (c) An internal market: This is selling of services to one another within the same organisation e.g. X-rays. There is an assumption that this will improve efficiency. (d) Information dissemination: Comparative information about various segments of the establishment can be disseminated to enhance peer group pressure to change practice that will bring about better efficiency. (e) Management team composition: The clinicians are to be involved in decision making body because they have more influence on the way resources are used. Their involvement in management team will invariably improve their level of awareness to cost and better efficiency. (2) Reallocation of resources (within the health sector): This is allocation of resources to priority areas. This is better observed in changing pattern of disease e.g. eradication of smallpox. Allocation should be based on planning- say based on the proportion of various groups in a population (% of children, elderly etc). Currently, most countries are allocating huge amount resources on the prevention, control and management of HIV/AIDS as compared to some other diseases. (3) Reallocation of resources to health sector (from other sectors): This done by the government by allocating more resources to health by reducing allocation to other sectors such as defence. It should be noted here that what reallocation of such funds would achieve in health sector might equally be achieved through education and Agriculture. Similar result can also be observed through provision of social infrastructure. CRITERIA FOR CHOOSING A FINANCING SYSTEM The choice of funding system involves a major policy decision. The followings are clear criteria for selection of the best method. The first 3 deals with any financing system while the last 3 hold true for primary health care system: (1) Viability and simplicity of use: Any financing system must possess the ability to be made to work. Careful consideration of technical feasibility is very important. Complex, bureaucratic and costly mechanism must be avoided. Say paying stations remote from places of consumption of services (use of banks etc). Cultural acceptability of the financing system must be considered in a community. (2) Revenue-generating ability: A system is said to be generating revenue when the cost of production is much less than the revenue earnings OR when the sale of goods and services are greater than that of the resources inputted i.e. output/income greater than input/expenditure. (3) Effects on service provision: The mode of financing health care can be dis/incentive to the users. You can create dis-incentive to urban dwellers to use a secondary level of care (Hospital) as a primary care centre by introducing heavy out of pocket charges in to the out patient department. The contrary will be done to those patients referred from the primary health care centre to the secondary centres. Also, in third party health care financing, some services such as preventive services (S& P) may carry more remuneration for the practitioner than extraction of wisdom tooth. Some other treatment may be discouraged such aesthetic care (orthodontic)-payment of such may not cover the entire practitioner’s bill. (4) Effects on equity: Equity here means “equal access to care for those in equal need”. There are two types of equity: Horizontal and Vertical equity. Horizontal means equal treatment of equals: those with similar health needs be given equal opportunity to access and treatment. Vertical equity means unequal treatment for unequals-those with greater needs would obtain concessional access e.g. more resources for TB prevention and control in endemic areas or lower income groups may have treatment and transport fare subsidized. This must be considered before a choice of financing system is chosen. User charges may discourage lower income earners from using/consuming a particular service(s). Social insurance may favour services utilisation by urban high income earners. Fund raising can be regressive or progressive depending on the relative income of the users. It is regressive if its takes a greater percentage of income from the lower income earners; it could be progressive if it takes a greater percentage of income from the higher income earners. The tax system of a country can be regressive if tax is placed on essential goods or progressive if placed on luxury goods. “Under tax based system, collective financing of health care is carried out in such a way that there is a transfer of resources from the richer elements of society to the poor and sick group”. In user charges, the sick will pay for the services s/he consumes without any cross-subsidy from others in the community (rich, healthy individuals). (5) Community participation: User charges allow the individual consumer to get involved in decision making. This is done by direct strengthening of direct relationship between the consumer and the provider. (6) Multi-sectorialism: This describes the involvement of other sectors of life to play key role in health care system (Engineers, Sociologists etc). A financing system may allow or disallow the involvement of other sectors of the society. User charges may not encourage fees collected for clinical services to be used for the provision of water for a particular community. This is contrary with the use of tax-based system. ALTERNATIVE SOURCES TO FINANCING HEALTH CARE. The major sources of financing health care are as follows: (A) Fees for service and insurance (B) Tax revenue and national insurance (C) Community financing (D) Loans and grants. (A) Fees for service and insurance: The most essential mode of health care financing is the fees for service. Fees are charged to cover the cost of the provided services. This is commonly found in many government health care facilities in developing countries. It is done so as to raise funds and to possibly discourage “unnecessary demand”. The World Bank suggested this type of health care financing but in differential manner .i.e. community preventive services should be rendered free, curative primary care by user charges and potential personalised preventive care at a reduced cost. It’s disadvantages are: (a) Collection may be difficult/complex (b) may not encourage equity (c) it discourages the real users (because price is a determining factor) (d) It is regressive because the poor are greatly affected (e) Waged labourer who are not paid during the course of sickness will be affected and (f) peasant farmers with highly seasonal income will face difficulties in paying for the health bills especially during pre-harvest period (which is also time they become more sick). Exemption schemes have been advocated to get around equity problems in health care financing but it has its own problems as well. The question of “who should be exempted” is a major obstacle. “Is it based on income level?” “If on income level at what level should be?” “What is the process of selecting exempts and who determine the exemption?” (‘the beauty is in the eyes of the beholder’). Exemption process can also discourage utilisation of services due stigmatizing of holders of such. Insurance coverage is another means of health care financing. Here the risk of illness is pooled among the insured group. There are various alternative combinations of coverage are available within the insurance schemes. Various combinations can be: in-patient or out-patient cover, with/out obstetric cover, exclusion of chronic diseases cover etc. Premium (monthly payment to the insurance company) depends on some factors. These factors are: (1) Type of care required: this is to know what type of medical conditions will be paid for; will it include preventive services? (2) Health status of the insuree: this can be determined by health indicators such as Age, Occupation (high risk?), life habits (smoking, alcoholism) and by conducting a medical test. This is done to possibly select high risk insurees that would consume more and afterwards make exorbitant claims from the insurance. Potentially high risk insuree may require paying high premiums or not covered for some services consumed. (3) Co-payment agreement: this will determine the amount of premium to be paid. Insuree agreeing to part-payment of some procedures may be required to pay lower premium. A reimbursement method may also be put in place-where the insuree pay for the consumed services and afterwards make claims from the insurance. Disadvantages: (1) It encourages stratification of health care system. Within the same community different people holds different insurance cover for their health as a result of their ability to pay varied amount of premiums. (2) Spreading of risk rarely occurs because the higher the risk the higher the premium to be paid. (3) administrative costs may make it inefficient as a revenue generator (paperwork for claims, advertisement, medical tests etc), (4) they tend to emphasize curative over the preventive care (5) difficulty in controlling overall medical costs- there can be abuse by demanding more than needed (6) tendency towards poor remuneration for the doctors (paying less for some difficult procedures etc) (7) It encourages changing of jobs- in that insurance policies are tied to employment. Health Maintenance Organisation (HMO): This is a variant of general insurance scheme. The members pay an annual amount of money to a health care provider to keep them healthy. The provider in turn provides services required directly or through a third party (i.e. pay other person/ other health care provider services not available in their centre). The practice here acts as the insurance company. It has the tendency to reduce its own costs through preventive care and hence minimizing unnecessary sophisticated medical procedures. It has been proposed to be a regime to the escalating health care costs in USA. Disadvantage: They may discriminate against members of the HMO schemes (those with lower educational background and can not push for their rights) e.g. referring them to higher hospitals where a higher costs may be paid by the referring HMO. (B) Tax revenue and national insurance: National Insurance Scheme (NIS): This widens the base of private schemes with payments tied to wage levels. It differs from private insurance scheme in that the cover is identical and premiums are based on the level of income (not on health status). Health care is often part of social security schemes. Contributions to the scheme are from the employees, employers and in some instances the State (government). Collection of premiums is better done among salaried individuals rather than the artisan, peasant farmers etc (no regular employment). Equity may be a big question here because stratification of care may be obvious (due to level of premium). Where services are not available carriers of social insurance scheme may only have ‘paper rights’. In some countries where social security schemes have being the method of caring for the health of the people. The government care for the populace from her own sources of revenue. The services are provided at minimal or no direct cost to all the citizens in cases of most comprehensive schemes. Equity, here depend on means of raising finance and the means of rationing and distributing the health care resultant from the ‘free service’. Raising finance can be from PAYE tax (Pay as you earn) which is progressive and regressive if from indirect tax (also depending on goods and services taxed). It is believed that Tax revenue and national insurance encourages equity and coverage (relative). Also, have potential to reduce unit costs through economics of scale and co-ordination of services. Disadvantages: Systems financed by tax revenue or national insurance are generally regarded as inefficient because there are no incentives to cut costs and addition of administrative costs. (C) Community financing UNICEF under the Bamako initiative suggested community fund raising to finance health care. One of these is service-use (e.g. Drug Revolving Funds (DRF)) and others which are community based (e.g. pre-paid community taxes). This has the advantage of community participation. The amount of money arising from such community in the overall that will be available for health will limit its uses not to think of if it has to be re-distributed to other communities (D) Loans and grants Loans and grants may be used to provide resources for health care financing. This can be through technical assistance or provision of free drugs. Loans are mostly used for capital financing while grants have the subsidizing effect on the cost of provision of services. Loans are to be re-paid back at a later time. Loans are to be properly look into so as to avoid noosing your neck in to difficult, concealed, stringent economic conditions. The World Bank usually give soft loans with little interest and longer period of payment but it should be noted that such loans can actually compound the economic recovery of a developing nation. Loans and grants are sometimes tied to a particular project or the way and where the money is to be spent e.g. donor may require that equipment and personnel must be purchased from their market. This may lead to purchase of spare parts and technical staff from abroad for maintenance purposes. Sources of loans and grants come from World Bank, Non-governmental organisations, foreign countries and organisations (EEC, EU, ECOWAS) etc.