Massive Left Ventricular Thrombus Amsterdam MD
advertisement
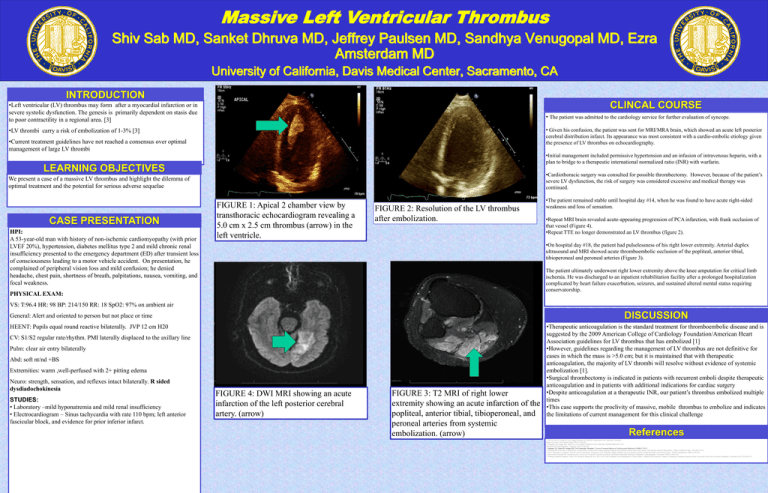
Massive Left Ventricular Thrombus Shiv Sab MD, Sanket Dhruva MD, Jeffrey Paulsen MD, Sandhya Venugopal MD, Ezra Amsterdam MD University of California, Davis Medical Center, Sacramento, CA INTRODUCTION CLINCAL COURSE •Left ventricular (LV) thrombus may form after a myocardial infarction or in severe systolic dysfunction. The genesis is primarily dependent on stasis due to poor contractility in a regional area. [3] • The patient was admitted to the cardiology service for further evaluation of syncope. • Given his confusion, the patient was sent for MRI/MRA brain, which showed an acute left posterior cerebral distribution infarct. Its appearance was most consistent with a cardio-embolic etiology given the presence of LV thrombus on echocardiography. •LV thrombi carry a risk of embolization of 1-3% [3] •Current treatment guidelines have not reached a consensus over optimal management of large LV thrombi •Initial management included permissive hypertension and an infusion of intravenous heparin, with a plan to bridge to a therapeutic international normalized ratio (INR) with warfarin. LEARNING OBJECTIVES •Cardiothoracic surgery was consulted for possible thrombectomy. However, because of the patient’s severe LV dysfunction, the risk of surgery was considered excessive and medical therapy was continued. We present a case of a massive LV thrombus and highlight the dilemma of optimal treatment and the potential for serious adverse sequelae CASE PRESENTATION HPI: A 53-year-old man with history of non-ischemic cardiomyopathy (with prior LVEF 20%), hypertension, diabetes mellitus type 2 and mild chronic renal insufficiency presented to the emergency department (ED) after transient loss of consciousness leading to a motor vehicle accident. On presentation, he complained of peripheral vision loss and mild confusion; he denied headache, chest pain, shortness of breath, palpitations, nausea, vomiting, and focal weakness. FIGURE 1: Apical 2 chamber view by transthoracic echocardiogram revealing a 5.0 cm x 2.5 cm thrombus (arrow) in the left ventricle. FIGURE 2: Resolution of the LV thrombus after embolization. •The patient remained stable until hospital day #14, when he was found to have acute right-sided weakness and loss of sensation. DISCUSSION •Repeat MRI brain revealed acute-appearing progression of PCA infarction, with frank occlusion of that vessel (Figure 4). •Repeat TTE no longer demonstrated an LV thrombus (figure 2). •On hospital day #18, the patient had pulselessness of his right lower extremity. Arterial duplex ultrasound and MRI showed acute thromboembolic occlusion of the popliteal, anterior tibial, tibioperoneal and peroneal arteries (Figure 3). The patient ultimately underwent right lower extremity above the knee amputation for critical limb ischemia. He was discharged to an inpatient rehabilitation facility after a prolonged hospitalization complicated by heart failure exacerbation, seizures, and sustained altered mental status requiring conservatorship. PHYSICAL EXAM: VS: T:96.4 HR: 98 BP: 214/150 RR: 18 SpO2: 97% on ambient air DISCUSSION General: Alert and oriented to person but not place or time HEENT: Pupils equal round reactive bilaterally. JVP 12 cm H20 CV: S1/S2 regular rate/rhythm. PMI laterally displaced to the axillary line Pulm: clear air entry bilaterally Abd: soft nt/nd +BS Extremities: warm ,well-perfused with 2+ pitting edema Neuro: strength, sensation, and reflexes intact bilaterally. R sided dysdiadochokinesia STUDIES: • Laboratory –mild hyponatremia and mild renal insufficiency • Electrocardiogram – Sinus tachycardia with rate 110 bpm; left anterior fascicular block, and evidence for prior inferior infarct. FIGURE 4: DWI MRI showing an acute infarction of the left posterior cerebral artery. (arrow) FIGURE 3: T2 MRI of right lower extremity showing an acute infarction of the popliteal, anterior tibial, tibioperoneal, and peroneal arteries from systemic embolization. (arrow) •Therapeutic anticoagulation is the standard treatment for thromboembolic disease and is suggested by the 2009 American College of Cardiology Foundation/American Heart Association guidelines for LV thrombus that has embolized [1] •However, guidelines regarding the management of LV thrombus are not definitive for cases in which the mass is >5.0 cm; but it is maintained that with therapeutic anticoagulation, the majority of LV thrombi will resolve without evidence of systemic embolization [1]. •Surgical thrombectomy is indicated in patients with recurrent emboli despite therapeutic anticoagulation and in patients with additional indications for cardiac surgery •Despite anticoagulation at a therapeutic INR, our patient’s thrombus embolized multiple times •This case supports the proclivity of massive, mobile thrombus to embolize and indicates the limitations of current management for this clinical challenge References 1. Nili M, Deviri E, Jortner R, et al. Surgical Removal of a Mobile, Pedunculated Left Ventricular Thrombus: Report of 4 Cases. Ann Thoracic Surg 1988; 46: 396-400. 2. Haugland JM, Asinger RW, Mikell FL, et al. Embolic Potential of Left Ventricular Thrombi Detected by Two Dimensional Echocardiography. Circulation 1984;70:588-598. 3. Stokman, PJ., Charn SN, Asinger RW."Left Ventricular Thrombus." Current Treatment Options in Cardiovascular Medicine 3.6 (2001): 515-21 4. Hochberg MS, Parsonnet V, Gielchinsky I, Hussain SM. Coronary artery bypass grafting in patients with ejection fractions below forty percent: early and late results in 466 patients. J Thorac Cardiovasc Surg.. 1983;86:519-527. 5. Sari I, Davutoglu V, Soydinc S, Sucu M, Ozer O. Fibrinolytic Treatment in Left Ventricular Mobile Thrombi with Low Ejection Fraction: Results and Follow-up of Seven Cases. J Thromb Thrombolysis 2008;25:293-296. 6. Stratton JR, Nemanich JW, Johannessen KA. Fate of Left Ventricular Thrombi in Patients with Remote Myocardial Infarction or Idiopathic Cardiomyopathy. Circulation 1988;78:1388-1393. 7. Writing Committee Members, Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;128:e240-319.