A Case Discussion of Infectious Lymphadenitis Mimicking Lymphoma
advertisement

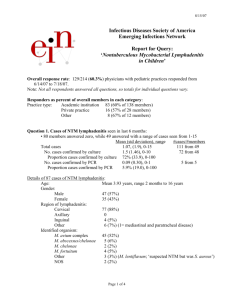
California Tumor Tissue Registry Case of the Month June, 2003 “A 29 y/o Man with Malaise and a Mass in the Neck” A 29-year-old male presented to his family physician with a two week history of malaise, fever, sore throat, and a neck mass. A monospot test was negative. On physical exam, a four cm mass in the left neck was palpated, eventually excised, and submitted for pathologic examination. Fig. 1. Lymph node follicles were enlarged and irregular and were separated by interfollicular zones filled with pale-staining cells. Insert: High magnification showed these “monocytoid B cells” to have small, round, mature nuclei and moderate amounts of pale or clear cytoplasm. Fig. 2. Some interfollicular regions showed early necrosis (insert). Fig. 3. Some cells contained large, eosinophilic intranuclear inclusions. Note that many of the surrounding lymphocytes had increased amounts of pale cytoplasm. Fig. 4. More viral inclusions. Note the engulfed granulocyte (insert). Fig. 5. An immunohistochemical stain for CMV showed only rare positive cells. DIAGNOSIS: Cytomegalovirus (CMV) lymphadenitis Christopher Poulos, M.D., Resident in Pathology, and Dennis P. O’Malley, M.D., Assistant Professor Department of Pathology and Laboratory Medicine Indiana University School of Medicine Reactive lymphadenopathies are usually categorized by the structural and immunologic areas of the lymph node that are affected (4). Generally: those that involve follicles are associated with B-cells and humoral immunity, those that involve the interfollicular spaces are associated with T-cell abnormalities and cell-mediated immunity, and those that involve the sinuses are part of a monocyte/macrophage response. CTTR’s Case of the Month June, 2003 1 Follicular responses are seen in a wide variety of disorders including HIV lymphadenopathy, syphilis, and others. Diffuse lymph node involvement (usually paracortical) (5) is seen with Epstein-Barr virus (EBV) infection, Varicella-Zoster virus (VZV) infection, Herpes simplex virus (HSV) infection, and postvaccinial lymphadenopathy (4). Involvement of the lymph node sinuses is seen in Rosai-Dorfman disease, other histiocytic proliferations, and in certain non-infectious disorders. A mixed pattern of nodal involvement may be encountered in a variety of entities including Toxoplasmosis, and in granulomatous infections such as cat-scratch disease and Yersinia. Classic acute EBV infection or infectious mononucleosis (IM) usually has distinctive clinical findings and usually do not require lymph node biopsy. Occasional cases, however, may require biopsy to rule out other causes of lymphadenopathy including malignancy (4). IM lymphadenitis is the prototype of a group of reactive lymphadenopathies which display diffuse paracortical involvement (5). The typical appearance of IM is of an expanded and mottled paracortex, immunoblastic proliferation, germinal centers that are usually small (but can be hyperplastic with follicular lysis), and a prominent vascular proliferation. The mottled appearance of the paracortex is primarily due to large transformed immunoblasts that are admixed with small paracortical T-cells, plasma cells and plasmacytoid lymphocytes. Although the presence of atypical immunoblasts, mitoses, and focal necrosis may cause confusion with large cell lymphoma, the polymorphous nature of the accompanying cells helps identify the proliferation as being reactive. Additionally, an unusual vascular prominence of venules with plump endothelial cells (perhaps incited as part of a generalized immune response) further supports a benign interpretation (5). In reactive lymphadenopathies (such as IM) the nodal sinuses are typically patent and filled with the reactive immunoblasts (2). The sinuses are usually unapparent in lymphomas. In reactive conditions the nodal architecture tends to be intact (but distorted), but is effaced in lymphoma. Besides large cell lymphomas, the differential diagnosis of IM lymphadenitis may include anaplastic large cell lymphomas and classical Hodgkin lymphoma (cHL). In addition to morphology, immunohistochemistry may be helpful in these situations. An immunostain for EBV may highlight large lymphocytes in IM, however it should be noted that some lymphomas are also EBV positive. Reactive lymphadenopathies due to CMV infection, HSV infection, VZV infection, or the post-vaccination state can all produce nearly identical morphologic changes to those seen in the previously-described prototypic EBV infection. CMV lymphadenitis may show localized lymphadenopathy with follicular hyperplasia and paracortical proliferations of monocytoid B-cells (4). Some cases will reveal the characteristic brick-red CMV intranuclear inclusions as are seen in our discussion case. These inclusions are usually found in T-cells or more often, within stromal or endothelial cells (5). Some infected large lymphocytes will be positive for CD15 and this may cause confusion with the RS cells of cHL. As in CTTR’s Case of the Month June, 2003 2 the current case, IHC for CMV, or FISH may provide confirmation of the diagnosis. HSV lymphadenitis can produce a very similar histologic picture as IM or CMV lymphadenitis, however the skin lesions are so characteristic that lymph node biopsy is rarely performed (4). But occasionally, HSV may present only with lymphadenitis and be otherwise asymptomatic, leading to biopsy. HSV lymphadenopathy tends to involve regional lymph nodes (i.e. inguinal) and the presence of isolated HSV lymphadenitis is often associated with hematopoietic malignancies (1,5). HSV lymphadenitis usually shows a paracortical immunoblastic proliferation, a polymorphous interfollicular infiltrate, and prominent necrosis. Multinucleated giant cells and typical Cowdry type A viral inclusions are only occasionally seen. The inclusion-bearing cells are often within the areas of necrosis (3). The primary differential diagnosis of HSV lymphadenitis is between other causes of necrotizing lymphadenitis, such as Kikuchi’s disease, other infectious lymphadenopathies, and high-grade lymphomas. As with other forms of viral lymphadenitis, diagnosis of HSV lymphadenitis can be confirmed using either viral immunostains or hybridization. Yet another form of lymphadenitis that can cause confusion with lymphoma is postvaccinial lymphadenitis. It has been reported that 50% of reported cases of postvaccinial lymphadenitis have previously been misdiagnosed as lymphoma of either the Hodgkin or Non-Hodgkin type (4). This emphasizes the need for adequate clinical history in evaluation of lymph nodes. Most cases present with enlarged, painful, lymph nodes presenting 7-15 days after vaccination in the area draining the injection site. The prototype of postvaccinial (“post immunization”) lymphadenitis occurs after administration of the smallpox vaccine. In the classic case, post-vaccinial lymphadenitis is histologically seen as a diffuse (before 15 days), or follicular (after 15 days) hyperplasia of immunoblasts with a mottled paracortex (4). The immunoblastic proliferation can resemble other forms of viral lymphadenitis and is accompanied by the typical changes seen in other reactive lymphadenitis. As with other viral lymphadenitis, the architecture of the node is distorted but not effaced as in lymphomas. Despite the fact that a postvaccinial lymph node may have Reed-Sternberg-like cells, the changes appear reactive and are unlike those seen in cHL (4). Nodes that are post-measles vaccination can appear very similar, but have increased numbers of plasma cells and usually contain Warthin-Finkeldy giant cells (4). The array of histologic lymph node changes associated with HIV infection are collectively known as “Persistent Generalized Lymphadenopathy” (PGL). Baroni and Uccini have stated that patients with PGL have an increased rate of progression to AIDS (1). As with the previously discussed forms of lymphadenopathy, the findings of HIV lymphadenopathy are nonspecific and may be confused with other viral lymphadenopathies requiring clinical and laboratory correlation to exclude other causes. PGL most often affects cervical or axillary lymph nodes, and histologically shows follicular abnormalities, either hyperplastic or regressive. Histologically, the first stage is CTTR’s Case of the Month June, 2003 3 follicular hyperplasia, consisting of increased numbers of follicles, many of which are enlarged and poorly formed. In the hyperplastic stage, there is also a proliferation of small blood vessels in the germinal centers, and the presence of interfollicular aggregates of monocytoid B-lymphocytes. The germinal centers are mainly composed of B-cells and rare T-cells. These hyperplastic changes may be with or without follicular fragmentation, which is marked by hemorrhage in germinal centers, foci of necrosis, and small lymphocyte infiltration of the necrotic foci. During follicular fragmentation there is a reduction in the number of CD4+ T cells with an increase in the number of CD8+ T cells, accompanied by follicular lysis and dissolution of the follicular dendritic cell network (1). This follicular fragmentation may represent early regressive changes of the lymph node and is associated thinning of the mantle zones. The regressive changes, subclassified into follicular involution and follicular depletion, are associated with an advanced stage of HIV disease (5). Follicular involution is characterized by small germinal centers with hyaline vascular-type centers, a surrounding layer of nucleolated follicular dendritic cells, and prominent paracortical HEVs, similar to the findings seen in Castleman’s Disease. Follicular depletion, is characterized by dominant nodal fibrosis, paracortical lymphocyte depletion, and effacement of the nodal architecture. Toxoplasmosis, a protozoan disease, can produce lymphadenitis with a mixed histologic pattern of nodal involvement similar to viral lymphadenopathies (4). It is estimated that up to 50% of US adults have been infected by the organism. Toxoplasmosis typically presents as a flu-like or IM-like syndrome. Lymphadenopathy may involve many nodes, but most often involves only the posterior cervical lymph nodes. Although serology (not histology) is the primary means of diagnosis, there are distinctive lymph node changes that can aid in a diagnosis. Toxoplasma lymphadenitis is characterized by follicular hyperplasia, marginal zone or monocytoid B cell hyperplasia, and microgranulomas that often encroach on germinal centers. The germinal centers have ragged, indistinct borders, many tingible body macrophages, and numerous mitotic figures. Microgranulomas are composed of small clusters of epithelioid histiocytes without giant cells (5). Microgranulomas may also be seen in various forms of lymphoma and sarcoidosis, which can lead to diagnostic confusion. Other common findings in Toxoplasmosis include the presence of subcapsular sinuses filled with the monocytoid Bcells and the presence of plasma cells and immunoblasts in the medullary cords. Toxoplasma cysts are rarely seen in the nodes and the genomes of the organism are only rarely detected, suggesting that the nodal findings are reactions to products of the organism, not to the organism itself (4). CTTR’s Case of the Month June, 2003 4 Summary Chart of Findings in Reactive Lymphadenopathies Type of Lymphadenopathy Nodal Compartment Involved Key Histologic Findings EBV (IM) Diffuse, Paracortical HSV Diffuse, Paracortical CMV Diffuse, Paracortical Postvaccinial Diffuse, Paracortical HIV Follicular Toxoplasmosis Mixed 1. Atypical immunoblastic proliferation with “mottled appearance” 2. Polymorphous background 3. Proliferation of HEVs 4. Variable necrosis 1. Findings similar to IM 2. Rare intranuclear inclusions 3. Discrete foci of necrosis; often extensive 1. Follicular Hyperplasia 2. Marginal zone hyperplasia 3. Characteristic inclusions 1. Follicular (after 15 days) or diffuse (before 15 days) immunoblastic proliferation 2. Polymorphic background 1. Follicular hyperplasia with or without fragmentation 2. Follicular regression with eventual lymphoid depletion 1. Follicular hyperplasia 2. Marginal zone hyperplasia 2. Microgranulomas Differential Diagnosis 1. Large Cell NHL 2. HD Key Factors in Establishing Final Diagnosis 1. Distorted but intact nodal architecture 2. Open sinuses 3. Polymorphic background 4. Staining for EBVLMP 1. Kikuchi’s Disease 2. Necrotic viral, bacterial, and fungal lymphadenitis 1. Immunostaining 2. In-situ hybridization 1. Other viral adenopathies 2. CHL 1. CD 15 staining 2. In-situ hybridization 3. Immunostaining 1. cHL 2. NHL 1. History critical 1. Other viral adenopathies 1. History 2. Viral serology 1. Sarcoid 2. NHL 1. Serology 2. Isolated posterior cervical lymph node involvement REFERENCES 1. Baroni CD, Uccini S. The Lymphadenopathy of HIV Infection, Am J Clin Pathol, 1993, 99: 397-401. 2. Childs CC, Parham DM, Berard C. Infectious Mononucleosis, The Spectrum of Morphologic Changes Simulating Lymphoma in Lymph Nodes and Tonsils. Am J Surg Pathol, 1987, 11(2): 122-132. 3. Gaffey MJ, Ben-Ezra JB, Weiss LM. Herpes Simplex Lymphadenitis. Am J Clin Pathol, 1991, 95: 709-714. 4. Knowles DM, Ed. Neoplastic Hematopathology, 2nd Ed. Lippincott Williams and Wilkins, Philadelphia, 2001, pp. 537-561. 5. Krishnan J, Danon AD, Frizzera G. Reactive Lymphadenopathies and Atypical Lymphoproliferative Disorders. Am J Clin Pathol, 1993, 99: 385-396. CTTR’s Case of the Month June, 2003 5