Thyroid Fine Needle Aspiration Biopsy (FNAB): Inside the Eye of a
advertisement
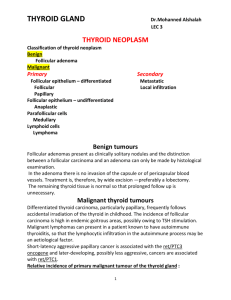
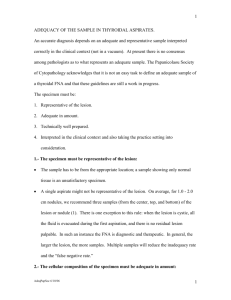
Thyroid Fine Needle Aspiration Biopsy (FNAB): Inside the Eye of a Cytopathologist Ian Jaffee, MD FCAP Director of Cytopathology California Pacific Medical Center Outline of Discussion • • • • Utility of FNAB Applications to thyroid nodules Cytology… Understanding the cytopathology report FNA of the Thyroid Gland • Safe, widely accepted, and cost-effective • Accurate “triage” of the thyroid nodule • Current estimates of ~30,000,000 people in U.S. with thyroid nodules > 1 cm • ~30,000 with malignant thyroid nodules • Goal: Identify patients who require surgical intervention Good practice in cytopathology • Direct communication • Collaboration with endocrinologist, surgeon (general vs ENT), radiologist, and PCP • Follow-up correlation with final surgical pathology Good practice in cytopathology • • • • • Benign Malignant The in betweens… Suboptimal samples (quality/quantity) Diagnostic guidelines – Papanicolaou Society of Cytopathology Task Force – American Thyroid Association – None have been necessarily universally accepted Diagnostic approach • Non-diagnostic • Benign • Atypical follicular lesion of undetermined significance (AFL-US) • Suspicious for follicular neoplasm/follicular lesion • Suspicious for malignancy • Malignant Non-diagnostic • Findings – – – – Blood only Absence of colloid Insufficient cellularity (“6/10 rule”) Colloid only (cyst contents) • Management: Follow-up U/S and repeat FNA • Repeated non-diagnostics and risk of malignancy – “quite low” (<5%) » McHenry CR, Walfish PG, Rosen IB. Non-diagnostic fine-needle aspiration biopsy: a dilemma in management of nodular thyroid disease. Am Surg. 1993;59:415-419. » Renshaw A, Significance of repeatedly non-diagnostic thyroid FNAs. Am J Clin Pathol 2011;135:750-752 Benign • “Most things in the thyroid are benign” • Risk of malignancy (~3%) Benign Thyroid Nodules (BTN) • Management: Clinical follow-up Atypical follicular lesion of undetermined significance (AFL-US) • • • • I don’t use it Poorly defined category Theoretical risk of malignancy is 5-15% Management: Repeat FNA or molecular triage (more later) Follicular lesions • • • • • Suspicious for follicular neoplasm Follicular neoplasm Follicular lesion Hürthle cell lesion Risk of malignancy: ~15-20% Cytology of follicular lesions Follicular adenoma • Capsule; no vascular invasion Follicular carcinoma • Capsular invasion • Vascular invasion Follicular lesions • Management Options: – Lobectomy – Lobectomy with frozen section – Total thyroidectomy – Molecular testing (more later…) Malignant • Suspicious for malignancy (risk of malignancy 60-75%) – Management: Lobectomy vs total thyroidectomy • Malignant (risk of malignancy 99%) – Management: Thyroidectomy Malignant • • • • • • • Papillary thyroid carcinoma Follicular carcinoma Medullary carcinoma Anaplastic carcinoma Poorly differentiated carcinoma Lymphoma Metastatic carcinoma Papillary thyroid carcinoma PTC: Surgical pathology Molecular triage of FNA samples • 60-70% of thyroid malignancies harbor at least one genetic mutation – BRAF – RAS – RET/PTC – PAX8-PPARγ Molecular triage of FNA samples • Indeterminate by cytology – AFL-US – Follicular category Available tests • VeraCyte (Afirma) – mRNA gene expression classifier – High NPV (>90%) but modest specificity (50+%) • Asuragen – Reportedly specific (rule-in/confirmatory) – RNA-based assay (RAS, BRAF, RET/PTC, and PAX8-PPARγ) • Quest Bonus Final comments • FNAB is highly accurate with high sensitivity and specificity • Accuracy in diagnosing thyroid abnormalities – dependant on the expertise of the cytopathologist interpreting the biopsy specimen – physician performing the biopsy • Categorization of samples – – – – – – Non-diagnostic Benign AFL-US Follicular (Suspicious for) lesion/neoplasm Suspicious for malignancy Malignant • FNA cannot reliably distinguish benign from malignant follicular neoplasm • New molecular triage testing (lukewarm) Tzanck you