Example 6 - Pediatric Trauma Society
advertisement
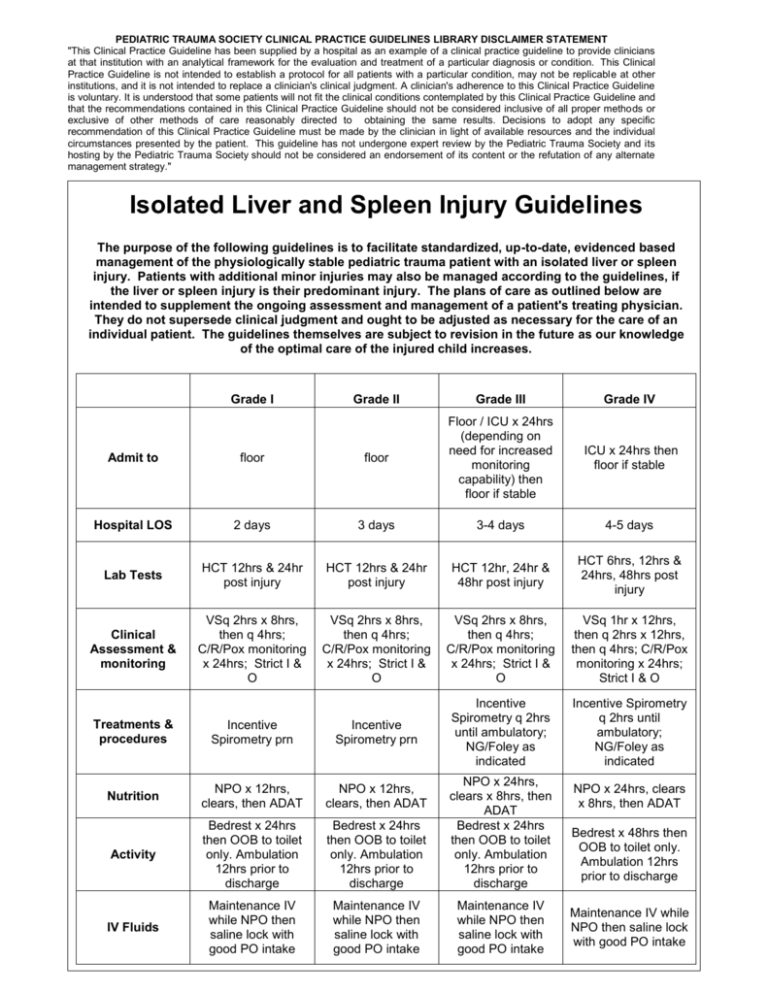
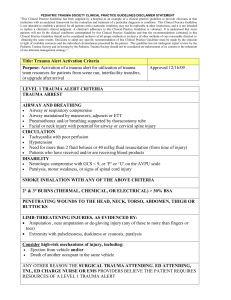
PEDIATRIC TRAUMA SOCIETY CLINICAL PRACTICE GUIDELINES LIBRARY DISCLAIMER STATEMENT "This Clinical Practice Guideline has been supplied by a hospital as an example of a clinical practice guideline to provide clinicians at that institution with an analytical framework for the evaluation and treatment of a particular diagnosis or condition. This Clinical Practice Guideline is not intended to establish a protocol for all patients with a particular condition, may not be replicable at other institutions, and it is not intended to replace a clinician's clinical judgment. A clinician's adherence to this Clinical Practice Guideline is voluntary. It is understood that some patients will not fit the clinical conditions contemplated by this Clinical Practice Guideline and that the recommendations contained in this Clinical Practice Guideline should not be considered inclusive of all proper methods or exclusive of other methods of care reasonably directed to obtaining the same results. Decisions to adopt any specific recommendation of this Clinical Practice Guideline must be made by the clinician in light of available resources and the individual circumstances presented by the patient. This guideline has not undergone expert review by the Pediatric Trauma Society and its hosting by the Pediatric Trauma Society should not be considered an endorsement of its content or the refutation of any alternate management strategy." Isolated Liver and Spleen Injury Guidelines The purpose of the following guidelines is to facilitate standardized, up-to-date, evidenced based management of the physiologically stable pediatric trauma patient with an isolated liver or spleen injury. Patients with additional minor injuries may also be managed according to the guidelines, if the liver or spleen injury is their predominant injury. The plans of care as outlined below are intended to supplement the ongoing assessment and management of a patient's treating physician. They do not supersede clinical judgment and ought to be adjusted as necessary for the care of an individual patient. The guidelines themselves are subject to revision in the future as our knowledge of the optimal care of the injured child increases. Grade I Grade II Grade III Grade IV ICU x 24hrs then floor if stable Admit to floor floor Floor / ICU x 24hrs (depending on need for increased monitoring capability) then floor if stable Hospital LOS 2 days 3 days 3-4 days 4-5 days Lab Tests HCT 12hrs & 24hr post injury HCT 12hrs & 24hr post injury HCT 12hr, 24hr & 48hr post injury HCT 6hrs, 12hrs & 24hrs, 48hrs post injury Clinical Assessment & monitoring VSq 2hrs x 8hrs, then q 4hrs; C/R/Pox monitoring x 24hrs; Strict I & O VSq 2hrs x 8hrs, then q 4hrs; C/R/Pox monitoring x 24hrs; Strict I & O VSq 2hrs x 8hrs, then q 4hrs; C/R/Pox monitoring x 24hrs; Strict I & O VSq 1hr x 12hrs, then q 2hrs x 12hrs, then q 4hrs; C/R/Pox monitoring x 24hrs; Strict I & O Incentive Spirometry q 2hrs until ambulatory; NG/Foley as indicated Incentive Spirometry q 2hrs until ambulatory; NG/Foley as indicated Treatments & procedures Incentive Spirometry prn Incentive Spirometry prn Nutrition NPO x 12hrs, clears, then ADAT NPO x 12hrs, clears, then ADAT Activity Bedrest x 24hrs then OOB to toilet only. Ambulation 12hrs prior to discharge Bedrest x 24hrs then OOB to toilet only. Ambulation 12hrs prior to discharge NPO x 24hrs, clears x 8hrs, then ADAT Bedrest x 24hrs then OOB to toilet only. Ambulation 12hrs prior to discharge IV Fluids Maintenance IV while NPO then saline lock with good PO intake Maintenance IV while NPO then saline lock with good PO intake Maintenance IV while NPO then saline lock with good PO intake NPO x 24hrs, clears x 8hrs, then ADAT Bedrest x 48hrs then OOB to toilet only. Ambulation 12hrs prior to discharge Maintenance IV while NPO then saline lock with good PO intake PEDIATRIC TRAUMA SOCIETY CLINICAL PRACTICE GUIDELINES LIBRARY DISCLAIMER STATEMENT "This Clinical Practice Guideline has been supplied by a hospital as an example of a clinical practice guideline to provide clinicians at that institution with an analytical framework for the evaluation and treatment of a particular diagnosis or condition. This Clinical Practice Guideline is not intended to establish a protocol for all patients with a particular condition, may not be replicable at other institutions, and it is not intended to replace a clinician's clinical judgment. A clinician's adherence to this Clinical Practice Guideline is voluntary. It is understood that some patients will not fit the clinical conditions contemplated by this Clinical Practice Guideline and that the recommendations contained in this Clinical Practice Guideline should not be considered inclusive of all proper methods or exclusive of other methods of care reasonably directed to obtaining the same results. Decisions to adopt any specific recommendation of this Clinical Practice Guideline must be made by the clinician in light of available resources and the individual circumstances presented by the patient. This guideline has not undergone expert review by the Pediatric Trauma Society and its hosting by the Pediatric Trauma Society should not be considered an endorsement of its content or the refutation of any alternate management strategy." Grade I Grade III Grade IV Mild pain Tylenol 15mg/kg po/pr q 4hrs prn Grade II Mild pain Tylenol 15mg/kg po/pr q 4hrs prn Moderate Pain Tylenol with Codeine 1mg/kg po q 4hrs prn Severe Pain Morphine 0.1mg/kg IV q 24hrs prn Mild pain - Tylenol 15mg/kg po/pr q 4hrs prn Moderate Pain Tylenol with Codeine 1mg/kg po q 4hrs prn Severe Pain Morphine 0.1mg/kg IV q 2-4hrs prn Mild pain - Tylenol 15mg/kg po/pr q 4hrs prn Moderate Pain - Tylenol with Codeine 1mg/kg po q 4hrs prn Severe Pain Morphine 0.1mg/kg IV q 2-4hrs prn none none none none 3 weeks 4 weeks 5 weeks 6 weeks *6 weeks *8 weeks *12 weeks *16 weeks 1 week 1 week 1-2 weeks 1-2 weeks 2 weeks 2 weeks 2 weeks 1-2 weeks Medications Pre and Post discharge imaging Restricted activity for normal age appropriate activities Restricted activity for full contact/competitive sports or play Return to school Follow-up clinic visit *Return to full-contact / competitive sports or play (Gymnastics, dance, Biking, Skiing, Snow boarding, Sled riding, Swimming, Jungle Gyms, Skateboarding, Rollerblading, Running and Jogging, Basketball, Soccer, Football, Boxing, Diving, Ice/Field Hockey, Lacrosse, Martial Arts, Rodeo, Rugby, Wrestling, Handball, Mountain Climbing, etc) is at the discretion of the individual's pediatric trauma surgeon. PEDIATRIC TRAUMA SOCIETY CLINICAL PRACTICE GUIDELINES LIBRARY DISCLAIMER STATEMENT "This Clinical Practice Guideline has been supplied by a hospital as an example of a clinical practice guideline to provide clinicians at that institution with an analytical framework for the evaluation and treatment of a particular diagnosis or condition. This Clinical Practice Guideline is not intended to establish a protocol for all patients with a particular condition, may not be replicable at other institutions, and it is not intended to replace a clinician's clinical judgment. A clinician's adherence to this Clinical Practice Guideline is voluntary. It is understood that some patients will not fit the clinical conditions contemplated by this Clinical Practice Guideline and that the recommendations contained in this Clinical Practice Guideline should not be considered inclusive of all proper methods or exclusive of other methods of care reasonably directed to obtaining the same results. Decisions to adopt any specific recommendation of this Clinical Practice Guideline must be made by the clinician in light of available resources and the individual circumstances presented by the patient. This guideline has not undergone expert review by the Pediatric Trauma Society and its hosting by the Pediatric Trauma Society should not be considered an endorsement of its content or the refutation of any alternate management strategy." PEDIATRIC TRAUMA SOCIETY CLINICAL PRACTICE GUIDELINES LIBRARY DISCLAIMER STATEMENT "This Clinical Practice Guideline has been supplied by a hospital as an example of a clinical practice guideline to provide clinicians at that institution with an analytical framework for the evaluation and treatment of a particular diagnosis or condition. This Clinical Practice Guideline is not intended to establish a protocol for all patients with a particular condition, may not be replicable at other institutions, and it is not intended to replace a clinician's clinical judgment. A clinician's adherence to this Clinical Practice Guideline is voluntary. It is understood that some patients will not fit the clinical conditions contemplated by this Clinical Practice Guideline and that the recommendations contained in this Clinical Practice Guideline should not be considered inclusive of all proper methods or exclusive of other methods of care reasonably directed to obtaining the same results. Decisions to adopt any specific recommendation of this Clinical Practice Guideline must be made by the clinician in light of available resources and the individual circumstances presented by the patient. This guideline has not undergone expert review by the Pediatric Trauma Society and its hosting by the Pediatric Trauma Society should not be considered an endorsement of its content or the refutation of any alternate management strategy."