Complications of Dermatologic Laser Surgery
advertisement

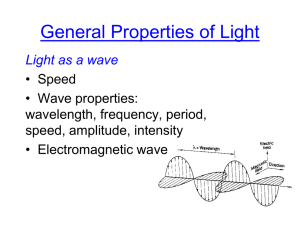
Complications of Dermatologic Laser Surgery Author: Clarence William Brown Jr, MD, Assistant Professor of Dermatology, Director of Dermatologic and Mohs Micrographic Surgery, Rush University Medical Center Contributor Information and Disclosures Updated: Oct 7, 2009 Introduction Over the course of the past 2 decades, the indications for their use and the number of different lasers available to treating physicians have increased dramatically. Combined with widespread media attention fueling a strong public focus on youth and beauty, the volume of laser procedures performed has increased steadily and, with this, so has the number of resulting complications observed from their use. Understanding the science and principles behind laser surgery can help to minimize the potential for complications; however, as with all surgical modalities, excellent surgical results are tempered by undesirable adverse outcomes. For the purposes of this article, any undesired effect of a laser intervention is considered a complication, regardless of its frequency. For example, purpura following short-pulsed, pulsed dye laser therapy of telangiectasia or erythema following carbon dioxide laser resurfacing is expected in 100% of patients treated; nevertheless, these problems are still noted as complications. Laser Surgery Principles and Potential Complications Laser light (energy) has unique properties that allow it to be used therapeutically. Laser light is monochromatic (single wavelength), coherent (in phase, both in time and space), and collimated (light waves are parallel). These properties make possible the generation and delivery of high fluence (energy per area), which can interact with the skin to effect clinical outcomes that are both desired and undesired. Additionally, the monochromaticity of laser light is essential for selective targeting of structures in the skin (chromophores), which preferentially absorb light of that wavelength. Commonly targeted chromophores in the skin, which each have their own unique absorption spectrum for laser light, include water, hemoglobin, melanin, and tattoo ink. When laser light hits the skin, it may be reflected, transmitted, or absorbed. Absorbed energy is most responsible for the clinical effect because it is converted to thermal energy (heat) by the intended targets (chromophores). In many cases, complications result from collateral damage created when energy intended for the target chromophore is nonselectively diffused to and absorbed by surrounding tissues and structures. For example, hyperpigmentation and hypopigmentation noted after carbon dioxide laser resurfacing are related to damage to melanocytes vaporized along with targeted keratinocytes and fibroblasts in the epidermis and dermis. Similarly, in laser-assisted hair removal, unwanted damage to the epidermis (including melanocytes) may occur despite the fact that follicular melanin is the intended target. The first cutaneous lasers used continuous beams of laser light. Even when wavelengths relatively specific for a particular chromophore were used, their continuous output dictated that the tissue dwell time (ie, how long the laser was held to the skin) depended on the speed of the surgeon's hand—typically long enough to cause a buildup of thermal energy that diffused to nontargeted adjacent tissue. This led to undesirable rates of adverse effects and complications (notably, scarring) that limited the use of cutaneous lasers. For example, until the advent of pulsed dye lasers in the mid 1980s, continuous-beam argon lasers were used to treat port-wine stains. Despite high absorption by the target chromophore hemoglobin, nonspecific damage to surrounding tissue and scarring was relatively common. Most of the currently used lasers take advantage of Anderson and Parrish's theory of selective photothermolysis, thus minimizing the undesired collateral damage discussed above. This theory states that selective heating of a target chromophore is achieved when the laser wavelength is preferentially absorbed by the chromophore, the energy of the laser is high enough to damage the chromophore, and the pulse duration of laser energy is shorter than the thermal relaxation of the target (time it takes for the target to cool by 50% of its peak temperature after irradiation).1 The majority of cutaneous lasers in use today operate according to these principles and attempt to limit the duration of the laser light's impingement on tissue. In recent years, the majority of cutaneous lasers have been used with systems to cool the epidermis to prevent collateral damage to epidermal structures from laser light intended to target deeper structures. Some of the most recent advances in laser and light equipment technology uses within treatment fields small areas of therapeutic energy exposure interspersed with well-organized skip areas of normal, untreated skin. Often, these fields of treatment are administered via a specially designed handpiece, and the areas of normal untreated skin speed the healing process, while the small size of the treated surface results in an evident clinical effect but also serves to minimize the risk for adverse events and outcomes. All of the cutaneous laser systems in current use target structures in the epidermis or dermis. Most adverse effects and complications of laser treatment can be predicted by understanding that they are mainly due to collateral damage of normal adjacent skin structures. Introduction to Classification of Dermatologic Laser Complications Each laser system has its own adverse effect and complication profile specific to the cutaneous lesion being treated. Possible complications related to any aspect of a specific laser treatment (including anesthesia) should be discussed in full with the patient as part of the procedure of obtaining informed consent. The following sections outline the spectrum of cutaneous laser complications. Not all potential complications for each individual laser system are listed. Newer devices in the past few years include nonablative laser systems and fractional lasers (fractional photothermolysis).2 These lasers, unlike classic ablative resurfacing lasers (eg, carbon dioxide, erbium), typically have the same low-risk profile for complications as other nonablative pulsed laser systems, which do not target the epidermis. Intense pulsed light has increasingly been used in clinical practice for photorejuvenation, treatment of vascular and pigmented lesions, and hair removal. Because the intense pulsed light is not a true laser, but an energy composed of a combination of numerous wavelengths of light, specific complications are beyond the scope of this article. As with all lightbased therapies, however, risks include hyperpigmentation, hypopigmentation, erythema, blistering, and scarring. Laser Safety Complications Ocular complications These may occur via direct or indirect ocular exposure to laser irradiation. Potential damage is wavelength-specific. For example, carbon dioxide or erbium lasers (chromophore: water) damage the cornea on impact. On the other hand, 585- or 595-nm pulsed dye lasers (chromophore: hemoglobin) and several red and infrared pigment-specific lasers (eg, ruby, alexandrite, Nd:YAG) pass through the cornea and lens and damage choroidal and retinal vasculature or retinal pigment, respectively. Thus, wavelength-specific eyewear must be worn by both operators and patients. Fire and electric shock With high enough energy and absorption, laser beams can ignite clothing, hair, or paper products. The risk increases in the presence of oxygen, methane, and alcohol. Precautions (eg, removing or protecting hair and clothing within the treatment areas) must be taken to prevent this. Electric shock due to the high voltage required by lasers can also occur. Proper wiring during installation is critical. Infection of personnel Depending on the laser and its indication, laser-tissue interaction may produce a smoke plume and/or tissue splatter. While it is difficult to quantify the actual risk of transmission of infection, concerns exist. Human papillomavirus has been cultured from the plume generated with carbon dioxide laser treatment of warts.3 A smoke evacuator and special laser mask (filtered to 0.3 µm) should be used if laser plumes are anticipated. Additionally, the tissue splatter produced by some Q-switched lasers necessitates wearing of gloves, eye protection, and masks. Primarily Epidermal Complications Hyperpigmentation Postoperative hyperpigmentation can be observed after virtually any cutaneous laser or intense pulsed light procedure. This problem is more common in patients with darker skin types. Patients with fresh tans are also more at risk. Hyperpigmentation is almost always a temporary effect that responds to topical bleaching therapy and resolves over time. Hyperpigmentation is relatively common after ablative (especially carbon dioxide laser) resurfacing, lasting an average of 3-4 months. The risk of hyperpigmentation with laser-assisted hair removal is related to seasonal variations, the presence of a tan, and the intrinsic pigment defining the patient's skin type. Idiosyncratic hyperpigmentation may occur, and patients should always be warned of this risk. Interestingly, although cryogen spray cooling systems limit hyperpigmentation due to epidermal heating, excessive application of cooling in itself can cause epidermal damage and hyperpigmentation. 4 Hypopigmentation Postoperative hypopigmentation is also possible, particularly after the use of lasers that target melanin as a chromophore, or pigment-specific laser irradiation. Thus, it is quite common in tattoos, pigmented lesions, or hair removal treated with Qswitched ruby, alexandrite, and Nd:YAG lasers. In these situations, hypopigmentation is more commonly observed after multiple treatments and is more common in patients with darker skin types. In 1998, Nanni and Alster reported that hypopigmentation occurs in about 10% of patients treated for hair removal with the long-pulsed ruby and alexandrite lasers.5 As with hyperpigmentation, this complication is often temporary, although permanent hypopigmentation has been noted. Delayed permanent hypopigmentation has been recognized as a complication particular to ablative laser resurfacing especially carbon dioxide laser skin resurfacing. Postoperative blistering Blister formation (or vesiculation) is due to epidermal thermal damage and, while uncommon, can be produced by virtually all laser systems. It is most often observed with Q-switched laser irradiation for tattoo removal. Explanations for its development include use of excessive laser fluence or inadvertent absorption of laser energy attributable to the increased presence of an epidermal chromophore (eg, melanin in a tan). The concomitant use of tissue cooling (through a contact chill tip or cryogen spray) serves to protect the epidermis from excessive thermal damage during laser irradiation, and improperly applied or improperly functioning cooling may also account for epidermal damage.6 Postoperative crusting This undesirable effect is also caused by laser-induced epidermal damage (see postoperative blistering above). Crusting is common with Q-switched lasers used for tattoo removal but can be observed after treatment with other lasers as well. Without appropriate postoperative care, crusting is inevitable after cutaneous laser resurfacing procedures. Milia Milia often occur as a normal event in the postoperative course of patients who have undergone carbon dioxide or erbium laser skin resurfacing. Their development may be reduced by application of topical tretinoin or glycolic acid. When just a few lesions are present, milia are easily treated by manual extraction. Primarily Dermal Complications Purpura Purpura (or bruising) is often noted in patients after pulsed-dye laser treatment. It was virtually inevitable with the firstgeneration 585-nm pulsed dye lasers and was typically used as a clinical measure of effective fluence selection. Purpura is a transient phenomenon that usually lasts 7-14 days. Its incidence has been reduced with the development of pulsed dye lasers with longer pulse durations, which permit slower heating of cutaneous vessels. Users of these systems can choose settings that minimize or eliminate purpura Scarring This permanent complication is perhaps the most feared of laser complications and was relatively common with continuouswave lasers. The risk of scarring with more recently developed pulsed and Q-switched lasers that use the principles of selective photothermolysis is far less, but scarring is still possible with almost any device. Whether atrophic or hypertrophic in type, scarring is always due to excess damage to the collagen comprising the dermis. This may arise from direct laserinduced thermal damage or from complications such as postoperative infection. In general, the risk of scarring is low with pigment-specific lasers, pulsed vascular lasers, nonablative laser systems, and pulsed hair-removal laser systems. Cutaneous laser resurfacing (both carbon dioxide and erbium) has the highest risk of scarring because of the intended destruction of dermal tissue as well as the increased risk of infection in the deepithelialized skin. Factors such as the number of passes delivered and the energy used may affect the risk of scarring, while technology that uses a cooling system works to minimize this risk. Owing to the unique attributes of the individual’s skin receiving treatment, this complication may occur even at the hands of the most experienced surgeon and may occur in only a portion of the treatment field. Other Complications Delayed wound healing Although rare, delayed wound healing has been identified as a complication particular to carbon dioxide or erbium laser skin resurfacing. Once cutaneous infection and other systemic conditions (eg, lupus erythematous, connective-tissue disease) have been excluded as potential causative factors of the poor wound-healing response, its idiopathic nature is best managed with conservative wound management. Unfortunately, tissue fibrosis and scarring are common sequelae of a delayed woundhealing response. Wound infection Cutaneous wound infection is most common after laser skin resurfacing, although it is sometimes noted in any laser case in which the epidermis has been damaged. Superficial viral, bacterial, and fungal infections are possible. Herpes simplex virus may be reactivated in a patient during reepithelialization after cutaneous laser treatments, especially hair removal and resurfacing. Antiherpetic prophylaxis is thus recommended for all perioral or full-face laser resurfacing procedures. Bacterial infections are typically caused by staphylococcal or pseudomonal species and have been shown to appear more often in patients who have used occlusive wound dressings for a prolonged period after surgery. Similarly, candidal infections may occur. One case of parapharyngeal abscess formation after laser resurfacing has been reported. Darkening of flesh-colored cosmetic tattoos First noted upon irradiation of cosmetic (eyeliner, lipliner, browliner) tattoos with the Q-switched ruby laser, this phenomenon has also been reported with Q-switched Nd:YAG, Q-switched alexandrite, and 510-nm pulsed dye lasers. Darkening is attributable to the laser-induced conversion of ferric oxide to ferrous oxide in the cosmetic tattoo ink, producing an insoluble black pigmentation within the skin.7 Chrysiasis after laser treatment Q-switched laser treatment (eg, of lentigines) has led to persistent hyperpigmentation in treated areas in patients who have received gold therapy for other conditions.8 The hyperpigmentation is thought to be related to alteration of gold particles already present in the skin. Allergic reactions after laser treatment of tattoos Allergic reactions (including anaphylaxis) have been reported with Q-switched laser treatment of tattoos and are thought to be caused by altered antigenicity of the tattoo pigment by the laser. It also may be noted with some red tattoos. 9 Postoperative erythema Some degree of erythema lasting less than 24 hours is present in virtually all laser procedures. More prolonged erythema may occur as an unwanted adverse effect but is also transient in almost all patients treated with nonablative lasers. More prolonged erythema is noted in all patients after ablative laser skin resurfacing. Its duration (from days to several months) depends on the depth and degree of dermal wounding. Erbium lasers typically produce less postoperative erythema than carbon dioxide lasers. This may largely be a function of the more superficial treatment commonly performed with erbium lasers, although it may also be attributable to the lower degree of residual thermal necrosis produced in the dermis upon erbium laser irradiation. An unusual reticulate erythema has been reported with diode lasers in hair removal. 10 Contact dermatitis to topical postoperative medications Allergic contact dermatitis or irritant contact dermatitis can develop after any type of laser procedure, most commonly to a topical antibiotic. Because of the difficulty in distinguishing contact dermatitis from infection in patients who have had laser resurfacing, many practitioners avoid the use of topical antibiotics in such patients. References 1. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. Apr 29 1983;220(4596):524-7. [Medline]. 2. Fisher GH, Geronemus RG. Short-term side effects of fractional photothermolysis. Dermatol Surg. Sep 2005;31(9 Pt 2):1245-9; discussion 1249. [Medline]. 3. Sawchuk WS, Weber PJ, Lowy DR, Dzubow LM. Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: detection and protection. J Am Acad Dermatol. Jul 1989;21(1):41-9. [Medline]. 4. Handley JM. Adverse events associated with nonablative cutaneous visible and infrared laser treatment. J Am Acad Dermatol. Sep 2006;55(3):482-9. [Medline]. 5. Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. Mar 1998;24(3):315-20. [Medline]. 6. Willey A, Anderson RR, Azpiazu JL, et al. Complications of laser dermatologic surgery. Lasers Surg Med. Jan 2006;38(1):1-15. [Medline]. 7. Anderson RR, Geronemus R, Kilmer SL, Farinelli W, Fitzpatrick RE. Cosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatment. Arch Dermatol. Aug 1993;129(8):1010-4. [Medline]. 8. Geist DE, Phillips TJ. Development of chrysiasis after Q-switched ruby laser treatment of solar lentigines. J Am Acad Dermatol. Aug 2006;55(2 Suppl):S59-60. [Medline]. 9. Ashinoff R, Levine VJ, Soter NA. Allergic reactions to tattoo pigment after laser treatment. Dermatol Surg. Apr 1995;21(4):291-4. [Medline]. 10. Lapidoth M, Shafirstein G, Ben Amitai D, Hodak E, Waner M, David M. Reticulate erythema following diode laserassisted hair removal: a new side effect of a common procedure. J Am Acad Dermatol. Nov 2004;51(5):7747. [Medline]. 11. Alster TS, Lupton JR. Treatment of complications of laser skin resurfacing. Arch Facial Plast Surg. OctDec 2000;2(4):279-84. [Medline]. 12. Bernstein LJ, Kauvar AN, Grossman MC, Geronemus RG. The short- and long-term side effects of carbon dioxide laser resurfacing. Dermatol Surg. Jul 1997;23(7):519-25. [Medline]. 13. Chan HH. Effective and safe use of lasers, light sources, and radiofrequency devices in the clinical management of Asian patients with selected dermatoses. Lasers Surg Med. Sep 2005;37(3):179-85. [Medline]. 14. Fisher AA. Lasers and allergic contact dermatitis to topical antibiotics, with particular reference to bacitracin. Cutis. Oct 1996;58(4):252-4. [Medline]. 15. Formica K, Alster TS. Complications of cutaneous laser resurfacing: a nursing guide. Dermatol Nurs. Oct 1998;10(5):353-6. [Medline]. 16. Garman ME, Orengo I. Unusual infectious complications of dermatologic procedures. Dermatol Clin. Apr 2003;21(2):321-35. [Medline]. 17. Horton S, Alster TS. Preoperative and postoperative considerations for carbon dioxide laser resurfacing. Cutis. Dec 1999;64(6):399-406. [Medline]. 18. Kilmer SL, Casparian JM, Wimberly JM, et al. Hazards of Q-switched lasers. Lasers Surg Med. 1993;suppl 5:56. 19. Kim YJ, Lee HS, Son SW, Kim SN, Kye YC. Analysis of hyperpigmentation and hypopigmentation after Er:YAG laser skin resurfacing. Lasers Surg Med. Jan 2005;36(1):47-51. [Medline]. 20. Laws RA, Finley EM, McCollough ML, Grabski WJ. Alabaster skin after carbon dioxide laser resurfacing with histologic correlation. Dermatol Surg. Jun 1998;24(6):633-6. [Medline]. 21. Levine VJ, Geronemus RG. Adverse effects associated with the 577- and 585-nanometer pulsed dye laser in the treatment of cutaneous vascular lesions: a study of 500 patients. J Am Acad Dermatol. Apr 1995;32(4):6137. [Medline]. 22. Lim SP, Lanigan SW. A review of the adverse effects of laser hair removal. Lasers Med Sci. Sep 2006;21(3):1215. [Medline]. 23. Manuskiatti W, Fitzpatrick RE, Goldman MP. Long-term effectiveness and side effects of carbon dioxide laser resurfacing for photoaged facial skin. J Am Acad Dermatol. Mar 1999;40(3):401-11. [Medline]. 24. Marra DE, Yip D, Fincher EF, Moy RL. Systemic toxicity from topically applied lidocaine in conjunction with fractional photothermolysis. Arch Dermatol. Aug 2006;142(8):1024-6. [Medline]. 25. Mortimer NJ, Chave TA, Johnston GA. Red tattoo reactions. Clin Exp Dermatol. Sep 2003;28(5):508-10. [Medline]. 26. Nanni CA. Postoperative management and complications of carbon dioxide laser resurfacing. Cosmetic Laser Surgery. 1993;37-55. 27. Nanni CA, Alster TS. Complications of cutaneous laser surgery. A review. Dermatol Surg. Feb 1998;24(2):20919. [Medline]. 28. Nanni CA, Alster TS. Laser-assisted hair removal: side effects of Q-switched Nd:YAG, long-pulsed ruby, and alexandrite lasers. J Am Acad Dermatol. Aug 1999;41(2 Pt 1):165-71. [Medline]. 29. Ragland HP, McBurney E. Complications of resurfacing. Semin Cutan Med Surg. Sep 1996;15(3):200-7. [Medline]. 30. Rendon-Pellerano MI, Lentini J, Eaglstein WE, Kirsner RS, Hanft K, Pardo RJ. Laser resurfacing: usual and unusual complications. Dermatol Surg. May 1999;25(5):360-6; discussion 366-7. [Medline]. 31. Sommer S, Sheehan-Dare RA. Atrophie blanche-like scarring after pulsed dye laser treatment. J Am Acad Dermatol. Jul 1999;41(1):100-2. [Medline]. 32. Tanzi EL, Alster TS. Side effects and complications of variable-pulsed erbium:yttrium-aluminum-garnet laser skin resurfacing: extended experience with 50 patients. Plast Reconstr Surg. Apr 1 2003;111(4):1524-9; discussion 15302. [Medline]. 33. Walia S, Alster TS. Cutaneous CO2 laser resurfacing infection rate with and without prophylactic antibiotics. Dermatol Surg. Nov 1999;25(11):857-61. [Medline]. 34. Weisberg NK, Greenbaum SS. Pigmentary changes after alexandrite laser hair removal. Dermatol Surg. Apr 2003;29(4):415-9. [Medline].