Why Am I Having So Much Trouble Curing The Pyoderma?
advertisement

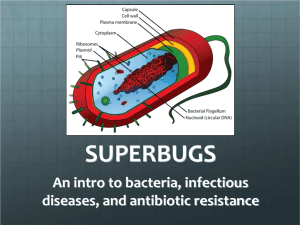
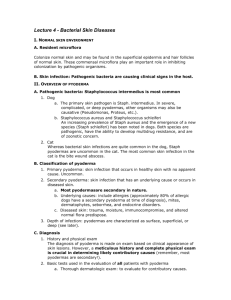
WHY AM I HAVING SO MUCH TROUBLE CURING THE PYODERMA? Candace A. Sousa, DVM Diplomate, American Board of Veterinary Practitioners Canine and Feline Practice Diplomate, American College of Veterinary Dermatology Senior Veterinary Specialist, Veterinary Specialty Team Pfizer Animal Health The word pyoderma literally means “pus in the skin” and refers to any purulent skin disease. In veterinary medicine the term is most commonly used to refer to a bacterial colonization or infection of the skin and/or hair follicle. Colonization occurs when there is bacterial overgrowth with minimal reaction (i.e. neutrophils) on the part of the body. An infection is the combination of the invasion of the body by a pathogenic microorganism and the reaction of the tissue to their presence and to the toxins generated by them. In dogs, bacterial pyoderma is stated to be the second most commonly diagnosed skin disorder, behind flea allergy dermatitis. However, with the advent of newer, highly effective flea-control products, this order may well have switched. Staphylococcus spp can be identified in about 94% of canine patients with bacterial pyoderma, with S intermedius identified in approximately 84% of these pyodermas. S schleiferi subsp coagulans and S aureus are a less common cause of bacterial pyoderma, isolated from approximately 8 % and 1% of patients, respectively. Bacterial pyoderma in dogs develops secondarily. Successful management involves identification of the causative underlying factor(s), recognition of the type (see below), correct antibiotic treatment and appropriate supportive care. Classification Canine bacterial pyodermas can be classified by depth of involvement, pattern, location or clinical outcome (see chart below). The most superficial form of pyoderma is surface colonization of the stratum corneum. Examples of this are intertrigo (skin-fold pyoderma) and pyotraumatic dermatitis (“hot spots”). The generalized erythema seen in dogs with chronic allergic skin disease may be due to this type of bacterial infection. Cytologic evaluation of these surface pyodermas shows only keratinocytes and bacteria. The term superficial pyoderma is used to describe an infection that extends below the stratum corneum more deeply into the epidermis and/or into the hair follicle. Impetigo, superficial folliculitis, and superficial spreading pyoderma are examples of this type of infection. Neutrophils are typically seen on cytologic evaluation of these types of pyoderma. A deep pyoderma occurs when the infection extends through the epidermis or hair follicle and causes a pyogenic inflammation of the dermis or subcutis. In cases of deep pyoderma, in addition to Staphylococcus, Gram-negative bacteria such as Proteus, Pseudomonas, Klebsiella or Escherichia coli may be cultured. If an antibiotic is chosen that is effective against the S intermedius, in most cases the other organisms are also eradicated. 1 Depth (Ihrke method) Pattern (Encyclopedia method) Location (Anatomist method) Surface Pyotraumatic dermatitis Intertrigo (folds) Superficial Epidermal collarettes Papules Subcorneal pustules Deep Bacterial folliculitis/furunculosis Cellulitis Puppy pyoderma (impetigo) Superficial spreading Folliculitis / Furunculosis Bullous impetigo Breed specific: German shepherd dog, plush-coated dog, etc. Folds - lip, face, tail, perivulvar (intertrigo) Complicated by obesity Friction areas - axillae, groin Trunk - generalized Pododermatitis/Interdigital Clinical Outcome Simple: resolves and does not recur Chronic recurrent: resolves with significant periods between episodes, but returns frequently Treatment failure: no response, no resolution or recurs in less than 7 days of ending therapy Using these classification schemes simultaneously to describe an individual patient’s bacterial pyoderma has value for planning subsequent diagnostic and therapeutic steps. Standardization of description will facilitate future evaluations as pyoderma is a recurring disorder. The presence of bacterial colonization or pyoderma is always secondary to an underlying cause. It is the obligation of the veterinarian to try to determine the precipitating cause and to treat or eliminate it in an effort to prevent re-infection. Unfortunately, this may be easier said than done. When an underlying or predisposing condition cannot be identified we refer to these cases as idiopathic (or primary) bacterial or staphylococcal pyoderma. Recurrent pyoderma is defined as a bacterial infection of the skin that responds entirely to appropriate systemic and / or topical therapy, but recurs shortly after cessation of therapy, usually within a month. Underlying Causes of Bacterial Pyoderma When evaluating a dog with pyoderma it is key to acknowledge that almost every dermatologic disease of the dog can have bacterial pyoderma as a component. The most common disorders complicated by secondary pyoderma are the allergic or pruritic diseases such as flea allergy dermatitis, food allergy, or atopic dermatitis. The pyoderma will generally worsen the pruritus. These allergic diseases may also have Malassezia colonization. Diseases of cornification such as congenital or idiopathic "seborrhea", icthyosis, and sebaceous adenitis alter the normal surface microenvironment and allow the overgrowth of bacteria. Endocrine disorders including hypothyroidism, hyperadrenocorticism (either iatrogenic or naturally-occurring), and abnormalities of the sex hormones may cause changes in the cornified layer predisposing to secondary bacterial pyoderma. Genodermatoses that cause cutaneous anatomic abnormalities (color dilution alopecia, black hair follicular dysplasia, and follicular dysplasia) may have secondary bacterial overgrowth and require long term therapy with antibiotics as a part of their management. Parasitic diseases of the dog such as demodicosis, scabies, and Cheyletiella infestations and other infectious diseases of the skin such as dermatophytosis, deep fungal infections, 2 and Malassezia dermatitis very often have concurrent secondary colonization or infection with S intermedius. It has been suggested that immunologic incompetence is the reason that some dogs develop pyoderma or recurrent pyoderma. Unfortunately, there are only very basic tests available to veterinarians to use to assess the immune system of the dog. Serum immunoglobulin quantitation and the total lymphocyte count are the only tests that are available to private practitioners. Theoretically, an absolute neutrophilia with a lymphocyte count of at least 1000 cells/µl should be seen in immunologically normal dogs with bacterial pyoderma. Identification and quantification of subsets of lymphocytes using markers (CD3+, CD4+, CD8+, etc), neutrophil function tests, and in vitro lymphocyte blastogenesis are tests performed in some universities and in research situations. To date these have not been useful in identifying specific defects causing bacterial pyoderma. Very young or very old dogs, animals with a neoplastic disease, or those who are receiving immunosuppressive drug therapy (especially prednisone which can suppress innate immunity) are susceptible to bacterial skin infections secondary to immunoincompetence. Diagnosis The diagnosis of bacterial pyoderma involves evaluation of signalment, history and physical findings. Consideration of breed, age and the role physical characteristics is important. In most cases this is a clinical diagnosis. Cytologic examination of skin surface or lesion exudates is a key and routine adjunctive diagnostic step. In some situations additional diagnostic steps such as culture and sensitivity, biopsy and/or laboratory testing may be needed. Characteristic clinical lesions are erythema, alopecia, pustules, papules, crusts, and epidermal collarettes (raised borders of detaching stratum corneum present at the margins of circular areas of inflammation). With a deep pyoderma, there are often nodules, erosions, ulcers, and draining tracts. If cytologic examination of material from the surface of the skin, a pustule, or a draining tract shows large cocci, usually in pairs, it is highly suggestive of pyoderma caused by S intermedius. The concurrent presence of rods is indicative of a mixed infection. When bacteria are seen within the cytoplasm of a neutrophil it confirms that they are not just contaminants. Skin biopsy is another valuable tool for the diagnosis of bacterial pyoderma. A response to treatment with oral antibiotics alone strongly supports the diagnosis of a pyoderma. Treatment Treatment of bacterial pyoderma in dogs must address both the bacteria and the underlying causative factors. The choice of an appropriate antibiotic can be made empirically or based on results of a culture and sensitivity test. A culture and sensitivity test is usually recommended for those cases of bacterial pyoderma that have made no clinical improvement after 2 weeks of treatment with an antibiotic that is typically effective against staphylococcal infections, used at the correct dose and frequency. The depth of the infection can interfere with and/ or delay successful therapy. A culture and sensitivity can be of value at the initiation of treatment of deep pyoderma, for infections suspected to be caused by Gram-negative organisms or if the animal has been treated previously with several different antibiotics. Veterinarians must decide what the goal of therapy is. Is it reasonable to expect to “cure” a bacterial skin disease that is caused by an overgrowth of an organism that is part of the normal microflora of that dog? It is an unrealistic to expect to cure bacterial pyoderma in a dog unless you can absolutely resolve the initiating cause(s). Unless the veterinarian accepts this, it is not possible to adequately educate the pet owner about the future course of their pet’s skin health. More likely is controlling the current infection, managing the underlying cause(s) and managing the recurrences. 3 Bacterial Culture/ Sensitivity Bacterial culture and antimicrobial sensitivity testing is beneficial for infections that are not responding to empirical therapy or may be complicated by Gram-negative organisms, when it is suspected that the infecting microorganism is resistant to the antimicrobial being used, when increasing the dose of the antimicrobial might have side effects, or when an antimicrobial might be very costly for the owner. Testing not only identifies the infecting organism(s) but also provides data regarding the in vitro efficacy of a drug. The Clinical and Laboratory Standards Institute (CLSI) [formerly the National Committee for Clinical Laboratory Standards (NCCLS)], promotes the development and use of voluntary consensus standards and guidelines for interpretation of sensitivity results. The M-31A document was developed by the Veterinary Antimicrobial Susceptibility Testing subcommittee of the NCCLS specifically for veterinary medicine. The standard methods for performing antimicrobial sensitivity tests are the KirbyBauer (disk-diffusion) or micro-well (tube) dilution. Other more automated systems such as the Sensititre and E-test systems are currently used by many laboratories. The diskdiffusion technique is a semiquantitative method of identifying sensitivity patterns. The drug concentration diffusing from the disk into the agar surrounding the disk creates a gradient from the disk outward that can be related to the anticipated drug concentration in the patient's serum when the drug is given at the recommended (label) dose. Measuring the zone of inhibition (that area around the disk where there is no bacterial growth) provides information about the relative efficacy of the antibiotic to slow growth or kill the microorganism. The micro-well dilution method provides more quantitative data regarding the amount of drug needed to inhibit bacterial growth. This technique evaluates the ability of bacteria to grow in media with increasing drug concentrations and thus determine the minimum inhibitory concentration (MIC) of the antibiotic. The culture is not sterilized and samples placed in an antimicrobial-free medium will grow again. An antimicrobial concentration that inhibits the growth of 50% of the isolates tested is termed the MIC50. The concentration that inhibits the growth of 90% of the isolates is termed the MIC90. When comparing the efficacy of various antibiotics, the MIC90 is the commonly used value. Although the MIC is an in-vitro quantification it allows comparison of the relative sensitivity of the microorganism to different drugs. This information will help with drug selection when comparing drugs that reach similar concentrations in the patient's serum. If the MICs for the same organism increases over time this indicates the possibility of the development of resistance. The breakpoint MIC of a drug is the MIC value below which the likelihood of treatment success is great and the likelihood of treatment failure is low. This estimation of successful treatment is derived from the MIC data obtained from efficacy studies, the pharmacokinetics and pharmacodynamics of the antibiotic in question, label dosage regimens and (if available) the efficacy of the drug established from well-controlled clinical studies of naturally occurring infections under field-use conditions. Bacterial isolates that have MICs exceeding the breakpoint MIC are not likely to respond to the drug under consideration using label dosage regimens. Exceeding the dosage regimen may enhance efficacy, but the safety margin of the product needs to be fully understood and evaluated before such treatment is used. Although MIC is specific information about a bacterium and drug, breakpoint MIC is specific to the host and drug. Breakpoint MICs may vary slightly between laboratories. Validated breakpoints are specific for a specific antimicrobial, a specific regimen of the antimicrobial (dose, route of administration, duration of therapeutic effect, frequency of dosing), animal species (possibly taking into consideration age or other factors), a specific pathogen and a specific disease entity (including the site of the infection). Breakpoints for use in veterinary medicine are specified in the NCCLS M31-A document. It should be noted 4 that the vast majority of companion animal antimicrobials use breakpoints established for humans. The relationship between these breakpoint MICs and efficacy in veterinary species has not been established. Bacteria are classified as sensitive (S), intermediate (I), or resistant (R), based on either the size of the zone of inhibition (from disk-diffusion methods), or on the MIC determined quantitatively. There is typically a 2-fold dilution difference between the MIC’s of organisms considered sensitive and intermediate, and a 4-fold dilution difference between MICs defining sensitive and resistant organisms. Bacterial isolates that are identified as intermediate should be carefully evaluated to determine whether aggressive therapy would be beneficial. From a laboratory perspective, the intermediate category serves as a "buffer" between sensitive and resistant categories to account for laboratory variability. Hence, the intermediate category should not be over-interpreted. However, intermediate isolates found in tissue sites where drug achieves high concentrations (e.g. urinary tract) may respond well to routine therapy. On the other hand, if the intermediately sensitive isolate was cultured from a tissue where there is poor drug penetration alternative therapy should be considered. Types of Antibiotics There are 2 groups of pharmacodynamically different antimicrobials. In the first group, activity improves as the drug concentration relative to the MIC of the pathogen increases. These are referred to as "concentration-dependent antibiotics” (e.g. aminoglycosides or fluoroquinolones). For these antibacterials, the ratio of the maximum plasma or serum concentration to the MIC (ratio of Cmax: MIC), known as the inhibitory quotient (IQ), and should exceed 8-10:1. It has been suggest that IQs higher than 10:1 may reduce the emergence of antibiotic resistance. The ratio of the AUC (area under the plasma concentration:time curve): MIC is known as the area under the inhibitory curve (AUIC). If a ratio of >125 can be achieved then this, too, may predict clinical efficacy for a dose-dependent antibiotic. The concern for drug safety prevents indiscriminate increases in dosage to increase the drug plasma concentration. If a drug is a time-dependent antibiotic (e.g. β lactams such as the penicillins, cephalosporins, sulfonamides, or lincosamides such as lincomycin or clindamycin) then clinical efficacy is dependent upon the amount of time that the drug concentration remains above the MIC for that microorganism. The half life of the drug then determines the frequency that the drug needs to be administered. The drug concentration should remain above the MIC for a minimum of 50% of the dosing interval to be effective. For drugs with substantial protein binding, this often means that concentrations of total (bound plus free) drug should exceed the MIC for the entire dosing interval. Antibiotic Selection The results of bacterial culture and sensitivity can provide veterinarians with valuable information, but the application of this must consider patient factors such as site of the infection, concurrent diseases or age. The relative potency of an antimicrobial and its pharmacodynamic properties must be balanced against the amount of active drug that will reach the site of infection and the duration of time the active drug remains at the site of infection. The effects of the local environment on the drug, including pus and scar tissue, and the ability of the microbe to impair the drug's efficacy must also be taken into account. Antibiotic therapy for canine pyoderma is based on recognition that the majority of cases are caused by S intermedius. Thus, empirical therapy should be an antibiotic with known efficacy against greater than 90% of the isolates of S intermedius. The second factor in the choice of an antibiotic is the safety of the drug based on published reports of side effects and on clinical experiences. These include even the annoying side effects such as diarrhea. The third is ease of administration, knowing that 5 owner compliance decreases in direct proportion to the frequency that the drug needs to be administered and for some delivery methods, and increases for chewable or tasty medications. And lastly, the cost to the owner should be considered, based on size of their dog and the anticipated length of therapy, needs to be considered. There are several different antibiotics that are useful for treating surface or superficial staphylococcal infections (see table for dosages and frequency of administration. Note: these are listed in the chart in alphabetical order, not in order of preference.) Antibiotics can be classified as narrow spectrum (an antibiotic that affects only a limited number of microorganisms i.e. most Gram+ but few if any Gram-; i.e. penicillin), extended spectrum (an antibiotic that has an extended spectrum of activity against the Gram- and the microorganisms that produce the β-lactamases i.e. Simplicef), or broad spectrum (an antibiotic that is active against a wider spectrum of microorganisms i.e. tetracycline). Due to the wide safety margin, low cost and extensive clinical experience, generic cephalexin, registered for use in humans, is probably the most commonly prescribed antibiotic used by veterinarians to treat staphylococcal pyoderma. It is a broad-spectrum, bactericidal cephalosporin that comes in a capsule or liquid form. Resistance develops very rarely. It is now available by prescription at many pharmacies and on line for a very low cost ($4 for 30 days, $10 for 90 days, or even free at some stores.) Cefa-Tabs® (cefadroxil) is a veterinary-labeled cephalosporin that is labeled to be used twice daily. Simplicef® (cefpodoxime proxetil) is a newer veterinary-approved cephalosporin with known activity against staphylococci. The benefits of this drug are that it is labeled to be administered once daily and the small size of the pill. Simplicef should not be used in dogs that are hypersensitive to penicillin or cephalosporin. Safety in pregnant and lactating animals or breeding male dogs has not been established. Convenia® (cefovecin) is the first antibiotic for dogs that provides an assured full course of treatment in a single veterinarian-administered dose. A single subcutaneous injection of Convenia effectively provides up to 14 days of treatment for the most common types of skin infections in dogs.3 Convenia is not for use in dogs or cats with a history of allergic reactions to penicillin’s or cephalosporin’s. Similar to other cephalosporin’s, side effects for both dogs and cats include vomiting, diarrhea, decreased appetite/anorexia and lethargy. The safety of Convenia has not been determined in lactating or breeding animals. Clavamox® (amoxicillin trihydrate / clavulanate potassium) is a broad spectrum, bactericidal β-lactam antibiotic combined with a β-lactamase inhibitor that has a spectrum of activity similar to that of cephalexin. In vitro susceptibility of 100% of coagulase-positive staphylococci over an 18 month period was demonstrated at The Ohio State University as well as in 100% of the isolates in a study from the United Kingdom.4,5 Antirobe® (clindamycin hydrochloride) is a narrow spectrum, β-lactamase-resistant lincosamide that has been shown to be effective in treating staphylococcal pyoderma at the label dose given twice daily or once daily based on a published report.1,2,6-8 In clinical trials, vomiting and diarrhea were occasionally observed. Clindamycin has also been shown to be effective in the treatment of deep pyodermas caused by susceptible strains of staphylococci.1 Lincocin® (lincomycin hydrochloride) is another lincosamide that has been shown to be safe and effective for treatment of canine staphylococcal pyoderma.7 Primor® (sulfadimethoxine / ormetoprim) is a potentiated sulfonamide that is labeled for use once daily.9,10 Clavamox®, Lincocin®, and Primor® should not be used in dogs with a history of hypersensitivity to the respective active ingredient. For detailed information about expected adverse events you should refer to the prescribing information. Tribrissen® (trimethoprim / sulfadiazine) and generic trimethoprim / sulfamethoxazole are other potentiated sulfonamides that can be useful in the treatment of canine staphylococcal pyoderma. 6 For dogs that have mixed bacterial cutaneous infections or deep pyoderma, Antirobe, Clavamox, or one of the fluoroquinolone antibiotics would be an appropriate empirical antibiotic choice. Fluoroquinolones are extended-spectrum, bactericidal antibiotics that have excellent activity against multiresistant organisms and very rapid killing activity. Because they are concentration-dependent and possess a prolonged postantibiotic effect, they are best administered once a day. Fluoroquinolones accumulate in phagocytes which accounts for the high drug levels documented in skin biopsies from dogs with deep pyoderma. Baytril® (enrofloxacin), Dicural® (difloxacin) and OrbaxTM (orbifloxacin) are 3 fluoroquinolones labeled for use to treat staphylococcal infections in dogs. Zeniquin® (marbofloxacin) has been shown to be very effective in the treatment of staphylococcal skin infections.11,12 As with all fluoroquinolones, Zeniquin® is not recommended for use in immature cats or dogs during the rapid growth phase, or in cats or dogs known to be hypersensitive to fluoroquinolones. The most common adverse reactions observed during clinical studies were decreased activity, loss of appetite, vomiting and diarrhea. Topical antibacterial therapy is an integral part of the initial treatment of a bacterial pyoderma and is also useful in preventing reoccurrences of the condition. The owner can be instructed to shampoo the dog as often as the dog needs it and as often as they are able (generally 2-3 times per week initially then once weekly once the infection is under control). Shampoos containing benzoyl peroxide, chlorhexidine, triclosan, or ethyl lactate have antimicrobial activity and are good choices for this adjunctive therapy. Owners are advised to let the shampoo contact the dog for a minimum of 10 minutes before rinsing. Use of a final leave-on rinse after bathing will assure that the active ingredient remains in contact with the skin and hair coat. Antibiotic creams or ointments are useful for spot treatment. Generic 2% mupirocin is a bactericidal antibiotic with excellent activity against Gram-positive cocci. Topical products that contain corticosteroids should be avoided when treating staphylococcal pyoderma. So why did my treatment fail (or why did the condition recur?) Although there are often identifiable reasons in a specific patient why therapy failed, it is essential to repeat that for the majority of dogs that develop bacterial pyoderma it will be a recurrent problem. It is the obligation of the veterinarian to try to identify and control all factors that are leading to the re-occurrences. But concurrent commitment to educating the pet owner to reasonable expectations about this disorder is key to successful management. That being said, the signs of pyoderma during the treatment period and for subsequent 4 -6 weeks should be controlled. If this is not achieved some of the possible reasons are: • Wrong diagnosis Not every case of pyoderma is due to a bacterial infection. Make sure that the condition is not mimicking bacterial pyoderma such as juvenile cellulitis (“puppy strangles,”) demodicosis, dermatophytosis, pemphigus foliaceus, Malassezia dermatitis, T-cell lymphoma, cutaneous drug eruption, erythema multiforme, sterile nodular panniculitis or sun-damaged skin. • Client compliance Not administering prescribed medications as instructed is a huge factor in apparent treatment failure and is much more likely than true antibiotic resistance. In humans, one study found that as many as 60% of prescriptions are never filled. Of the prescriptions filled, only 40% are taken at the correct dosage, frequency, or duration. Compliance in veterinary medicine is not an animal issue but an owner issue. The frequency of antibiotic administration is inversely proportional to compliance. Once daily dosing increases compliance compared to twice daily or more frequent dosing. Cefpodoxime (Simplicef), ormetoprim / sulfadimethoxine (Primor) or the fluoroquinolones 7 (i.e. marbofloxacin (Zeniquin)), all used once daily, can more assure that medications will be given. Cefovecin (Convenia) provides a method to achieve compliance more easily. A single injection will provide antibiotic treatment for up to 14 days. Wrong antibiotic “The most expensive antibiotic that you can dispense is the one that doesn’t work.” The empirical choice of an antibiotic should be based on efficacy first, safety second, convenience (=compliance) third, and lastly on cost. If there is any question about what antibiotic would be effective culture and sensitivity testing should be completed. Beta lactam antibiotics (amoxicillin / clavulanic acid, cefovecin, cefpodoxime, cephalexin, cefadroxil) are a great first line antibiotic. (<5% resistance). The lincosamides (clindamycin (Antirobe), lincomycin (Lincocin) [approximately 22% of S intermedius are resistant]) and macrolides (erythromycin, 28% resistant) can be good alternatives, particularly if a dog exhibits an allergic reaction to a penicillin or cephalosporin, or for the treatment of some resistant staphylococci. The sulfa drugs (ormetoprim/sulfadimethoxine (Primor), trimethoprim/sulfonamides (variable reports 0-70% resistance)) and chloramphenicol (30% resistant) are also useful first line choices. Due to the high incidence of resistance, penicillin, ampicillin, amoxicillin and tetracycline should not be used to treat staphylococcal pyoderma unless a culture and susceptibility has been done and the results support their use (40-83% resistance) The fluoroquinolones should be reserved to empirically treat the deep infections (as the drug is concentrated in the white blood cell and carried to the site of the infection,) where the results of a culture and susceptibility test indicate that they are the correct choice, or where a once daily oral antibiotic is indicated and Simplicef or Primor are not appropriate choices. Inadequate dose or interval Inadequate doses occur more commonly when treating larger dogs, often in an attempt to save on cost. Antibiotic treatment should always be rounded up to next most convenient dose. When using fluoroquinolones always aim to the higher end in order to achieve the highest ration of Cmax (or AUC) to MIC to increase the chance of a successful treatment. When using time-dependent antibiotics such as cephalosporins the length of time above the MIC is most important factor to achieve efficacy. Pay close attention to dosing interval (this is where cefovecin has such value as one injection provides days of therapy). Cephalexin has a shorter half life (2.4 hours) than cefpodoxime (6… hours) so successful treatment is less forgiving for missed doses. Inadequate duration of treatment Clients may discontinue treatment once they perceive their pet’s condition has improved. They may also stop treating if their pet experiences any adverse side-effects such as a decreased appetite, vomiting or diarrhea. Veterinarians should dispense (or prescribe) enough antibiotics for a complete course of treatment and then schedule a recheck examination to decide if additional antibiotics are needed. Before accepting that there has been a treatment failure it is essential to determine if the medication was actually given. Antibiotic resistance Selection for bacterial resistance is greatest when the bacterial load is at its highest and antibiotic levels in target tissues fall below the concentration required to kill bacteria. With conventional antibiotic treatments, this situation can occur as antibiotic concentrations 8 decline between doses or when the course of treatment has been of insufficient duration. (FYI - by ensuring a full, two-week course of treatment in a single injection, Convenia eliminates the risk of missed doses or shortened treatments.) Recent publications have increased our awareness of the presence of methicillin resistant Staphylococci in both humans and pets. In vitro resistance to oxacillin is used to predict resistance to other penicillinase-resistant penicillins and -lactam antibiotics such as aminopenicillin-clavulanic acid combinations, cephalosporins, and carbapenems. There is concern in the veterinary community about a potential increase in the percentage of Staphylococci that are methicillin resistant. If an animal is not showing clinical improvement while being treated with an antibiotic that was selected empirically, a bacterial culture and susceptibility test should be performed to aid in the selection of the proper drug.13-23 S schleiferi and S aureus are more likely to be resistant to methicillin, oxacillin, and fluoroquinolones than S intermedius. Gram negative organisms such as Proteus, Pseudomonas, and E coli are rarely seen in simple, uncomplicated pyoderma. They can more often be cultured from special sites such as intertriginous areas (interdigital, axillae, perivulvar, lip fold, ear canals) and even more if the animal is obese. If rods are identified with cutaneous cytology a bacterial culture and susceptibility should be done. Other factors Possibly the most common reason that antibiotic therapy fails is due to failure to diagnose and manage underlying diseases. The most common underlying conditions that are missed are demodicosis, hypothyroidism and skin folds complicated by breed conformation and obesity that is untreated. Recurrent Staphylococcal Pyoderma As mentioned above, identification and control of the underlying cause of staphylococcal pyoderma is important in preventing recurrences. In some cases, however, despite our best efforts, a cause cannot be found. In those instances immunomodulatory therapy using products such as Staphage Lysate® or Immunoregulin® (Propionibacterium acnes bacterin) may be of benefit. As a last resort, some veterinarians and dermatologists will treat dogs with intermittent or pulse antibiotic therapy in an attempt to prevent re-infections. Some of the protocols that are advocated include a full course of therapy one week on, one week off; full course therapy 3 days out of the week; treatment 2 days out of the week 24 etc. There are no studies demonstrating the efficacy of one protocol over another however many dermatologists have used these protocols successfully to manage cases of idiopathic recurrent pyoderma. All of these regimes may contribute to the selection and emergence of resistant bacteria but again to date there is no concrete evidence to support this. 9 ANTIBIOTICS USEFUL IN CANINE DERMATOLOGY DRUG DOSAGE (mg/kg) 13.75 DOSAGE (mg/pound) 6.25 DOSE INTERVAL q 12 hours 10 q 12 hours 22 10 q 12 hours 8 3.6 5 - 10 2.3 - 4.6 subcutaneous, q 14 days up to 2 injections q 24 hours 5.5 - 33 11 1,2 5 - 10 2.5 – 15 5 2.3 - 4.6 q 12 hours q 24 hours q 24 hours 5 - 20 2.3 - 9.1 q 24 hours 10 22 (Lincocin®) 15.4 marbofloxacin 2.75 – 5.5 ® (Zeniquin ) orbifloxacin 2.5 - 7.5 TM (Orbax ) oxacillin 22 4.6 10 7 1.25 – 2.5 q 8 hours q 12 hours q 8 hours q 24 hours 1.1 - 3.4 q 24 hours 10 q 8 hours sulfadimethoxine / ormetoprim 25 (day 1) 12.5 (subsequent days) 6.8 q 24 hours 6.8 q 12 hours amoxicillin trihydrate / clavulanate potassium (Clavamox®) cephalexin 22 cefadroxil (Cefa-Tabs®) cefovecin sodium (Convenia®) cefpodoxime (Simplicef®) clindamycin (Antirobe®) difloxacin (Dicural®) enrofloxacin (Baytril®) erythromycin lincomycin 55 (day 1) 27.5 (subsequent (Primor®) days) sulfamethoxazole / 15 trimethoprim trimethoprim / 15 sulfadiazine q 12 hours 1. Scott, DW, Beningo, KE, Miller, Jr., WH, Rothstein, E. Efficacy of clindamycin hydrochloride for the treatment of deep pyoderma due to Staphylococcus intermedius infection in dogs. Can Vet J 39:753-56, 1998 2. Bloom, PB, Rosser, EJ. Efficacy of once-daily clindamycin hydrochloride in the treatment of superficial bacterial pyoderma in dogs. J Am Anim Hosp Assoc 37:537-42, 2001 10 References 1. Scott DW, Beningo KE, Miller, Jr. WH, Rothstein E. Efficacy of clindamycin hydrochloride for the treatment of deep pyoderma due to Staphylococcus intermedius infection in dogs. Can Vet J 39:753-56, 1998 2. Bloom PB, Rosser EJ. Efficacy of once-daily clindamycin hydrochloride in the treatment of superficial bacterial pyoderma in dogs. J Am Anim Hosp Assoc 37:537-42, 2001 3. Stegemann MR, Coati N, Passmore CA, Sherington J. Clinical efficacy and safety of cefovecin in the treatment of canine pyoderma and wound infections. JSAP 48:378-386, 2007 4. Lloyd DH, et al. Treatment of canine pyoderma with co-amoxyclav: A comparison of two dose rates. Vet Rec 141:439-41, 1997 5. Lloyd DH, Lamport AI, Feeney C. Sensitivity to antibiotics amongst cutaneous and mucosal isolates of canine pathogenic staphylococci in the UK, 1980-1996. Vet Derm 7:171-75, 1996 6. Littlewood JD, et al. Clindamycin hydrochloride and clavulanate-amoxycillin in the treatment of canine superficial pyodermas. Vet Rec 144:662-65, 1999 7. Harvey RG, et al. A comparison of lincomycin hydrochloride and clindamycin hydrochloride in the treatment of superficial pyoderma in dogs. Vet Rec 132:351-53, 1993 8. Noli C, Boothe D. Macrolides and lincosamides. Vet Derm 10:217-223, 1999 9. Scott DW, Miller, Jr. WH, Wellington JR. The combination of ormetoprim and sulfadimethoxine in the treatment of pyoderma due to Staphylococcus intermedius infection in dogs. Canine Prac 18:29-33, 1993 10. Messinger LM, Beale KM. A blinded comparison of the efficacy of daily and twice daily trimethoprim-sulfadiazine and daily sulfadimethoxine-ormetoprim therapy in the treatment of canine pyoderma. Vet Derm 4:13-18, 1993 11. Carlotti DN, Guaguere E, Pin D, et al. Therapy of difficult cases of canine pyoderma with marbofloxacin: a report of 39 dogs. J Sm Anim Prac 40:265-70, 1999 12. Paradis M, Abbey L, Baker B, Coyne M, Hannigan M, Joffe D, Pukay B, et al. Evaluation of the clinical efficacy of marbofloxacin (Zeniquin) tablets for the treatment of canine pyoderma: an open clinical trial. Vet Derm 12:163-169, 2001 13. Cherni JA, Boucher JF, Skokerboe TL, Tarnacki S, Gajawewski KD, Lindeman CJ. Comparison of the efficacy of cefpodoxime proxetil and cephalexin in treating bacterial pyoderma in dogs Intern J Appl Res Vet Med 4:85-93, 2006 14. Bemis DA, Jones RD, Hiatt LE, Ofori ED, Rohrbach BW, Frank LA, Kania SA. Comparison of tests to detect oxacillin resistance in Staphylococcus intermedius, Staphylococcus schleiferi, and Staphylococcus aureus isolates from canine hosts. J Clin Micro 44:3374-3376, 2006 11 15. Morris DO, Rook KA, Shofer FS, Rankin SC. Screening of Staphylococcus aureus, Staphylococcus intermedius, and Staphylococcus schleiferi isolates obtained from small companion animals for antimicrobial resistance: a retrospective review of 749 isolates (2003-04). Vet Derm 17:332-336, 2006 16. Pinchbeck LR, Cole LK, Hillier A, Kowalski JJ, Rajala-Schultz PJ, Bannerman TL, York S. Genotypic relatedness of staphylococcal strains isolated from pustules and carriage sites in dogs with superficial bacterial folliculitis. Am J Vet Res 67:1337-1346, 2006 17. Ganiere JP, Medaille C, Mangion C. Antimicrobial drug susceptibility of Staphylococcus intermedius clinical isolates from canine pyoderma. J Vet Med 52:25-31, 2005 18. Kania SA, Williamson NL, Frank LA, Wilkes RP, Jones RD, Bemis DA. Methicillin resistance of staphylococci isolated from the skin of dogs with pyoderma. Am J Vet Res 65:1265-1268, 2004 19. Zdovc I, Ocepek M, Pirs T, Krt B, Pinter L. Microbiological features of Staphylococcus schleiferi subsp. coagulans, isolated from dogs and possible misidentification with other canine coagulase-positive staphylococci. J Vet Med 51:449-454, 2004 20. Holm BR, Petersson U, Morner A, Bergstrom K, Franklin A, Greko C. Antimicrobial resistance in staphylococci from canine pyoderma: a prospective study of first-time and recurrent cases in Sweden. Vet Rec 151:600-605, 2002 21. Petersen AD, Walker RD, Bowman MM, Schott HC, Rosser EJ. Frequency of isolation and antimicrobial susceptibility patterns of Staphylococcus intermedius and Pseudomonas aeruginosa isolates from canine skin and ear samples over a 6-year period (1992-1997). J Am Anim Hosp Assoc 38:407-413, 2002 22. vanDuijkeren E, Box ATA, Heck MEOC, Wannte WJB, Fluit AC. Methicillin-resistant staphylococci isolated from animals. Vet Microbiol 103:91-97, 2004 23. Middleton JR, Fales WH, Luby CD, Oaks JL, Sanchez S, Kinyon JM, Wu CC, Maddox CW, Welsh RD, Hartmann F. Surveillance of Staphylococcus aureus in veterinary teaching hospitals. J Clin Microbiol 43:2916-2919, 2005 24. Carlotti DN, Jasmin P, Gardey L, Sanquer A. Evaluation of cephalexin intermittent therapy (weekend therapy) in the control of recurrent idiopathic pyoderma in dogs: a randomized, double-blinded, placebo-controlled study. Vet Derm 15 (suppl 1):8-9, 2004 12