Hayley Wickens
advertisement
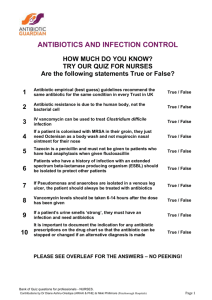
Smart use of antibiotics: building confidence in new approaches Dr. Hayley Wickens In this session • • • • Implementing antibiotic stewardship in the NHS Start Smart then Focus Gaps in our knowledge Starting appropriately, building confidence in the stop What is Antibiotic Stewardship? “…an activity that includes appropriate selection, dosing, route, and duration of antimicrobial therapy…”1 1. Dellit TH et al. Clin Infect Dis. (2007) 44 (2): 159-177 Antibiotic Stewardship in the NHS • Acute Trusts in England2 – 99% have empiric abx policy – 87% have iv-oral switch policy – 36% have automatic stop policy • Multidisciplinary Antimicrobial Management Teams – Cons micro/ID, abx/ID pharmacist, lead clinician, surgeon, senior nurse, senior pharmacist – Evidence-based guidelines & audit, abx usage/R monitoring, education – Smaller ward-based teams providing clinical review • National steering groups – – – – England – ARHAI N. Ireland – AMRAP implementation Group → ARAC Scotland – SAPG Wales - WARP 2. n=120, Wickens et al unpublished data 2011 Start Smart then Focus DH (Eng) Nov 20113 • Start Smart – Start abx on evidence of bacterial infection – Use local guidelines – Document on drug chart and notes: indication, duration/review date, route and dose – Obtain cultures first – Single dose surgical prophylaxis where evidence supports • Then Focus – Review diagnosis and abx by 48 hours, make the “Antimicrobial Prescribing Decision”: • • • • • Stop Switch IV to Oral Change/de-escalate Continue Outpatient Parenteral Antibiotic Therapy (OPAT) 3.http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/ documents/digitalasset/dh_131181.pdf Are you feeling lucky? Risk of undertreatment vs. risk of resistance • Guidelines: minimise broad spectrum abx, use narrow spectrum where possible • “But my patient is different” - Drs prioritise individual health gain over public health issue4: – ‘Non-compliant prescribing was mainly too broad compared with guideline-recommended therapy and rarely too narrow’ – 1/3 of all prescriptions too broad for empiric therapy; 2/3 too broad for culture-driven therapy, ‘streamlining’ not practiced. – ‘Availability of culture results had no impact on [policy] compliance in case of sepsis, but was associated with more compliance in UTI, and less compliance in LRTI’ – ‘Defensive behaviour may be driven by fear of high mortality rates and the fact that inadequate bacterial coverage has been correlated with increased mortality’ 4. Mol PGM et al (2006) Eur J Clin Pharmacol 62:297-305 Are you feeling lucky? Risk of undertreatment vs. risk of resistance • Are we treating a bacterial infection? – ‘Syndromic diagnosis’ – what combination of signs, symptoms, biochemistry, haematology will give us the confidence that we are treating a ‘real’ infection • How likely are we to be treating a resistant organism? – Lack of prospective epidemiology (apart from HIV/TB); US/EU data – transferable? – National R data? Local? 5. Meyer RJ et al (1997) NZ Med J 110:349-52 • Severity Scoring (e.g. CURB-65) – lack of validated scoring schemes apart from CAP, C.difficile, & low awareness5 – ‘low risk’ patients/confirmed pathogen could have narrow spectrum agents? • Lack of evidence on deescalation – All retrospective; outcomes good but may be risk averse on initiation. – Longer treatment courses →-ve effect? Summary • Implementing antibiotic stewardship in the NHS • Start Smart then Focus • Making sure the decision to start is sound – need for research into the sensitivity and specificity of combinations of signs/symptoms/biochemistry/haematology to predict bacterial infection requiring antibiotics – syndromic diagnosis • Choosing the narrowest-spectrum antibiotic that will cover the likely organisms empirically – need for research into evidence of (lack of) harm associated with starting narrow spectrum in low severity infection, escalating to broad spectrum if no response – any detriment to patient outcomes? • Building confidence in the stop/de-escalation – need for research into course duration and clinical outcomes; do longer treatment courses produce negative effects?