FAQ: Photography for pressure ulcer documentation:
advertisement
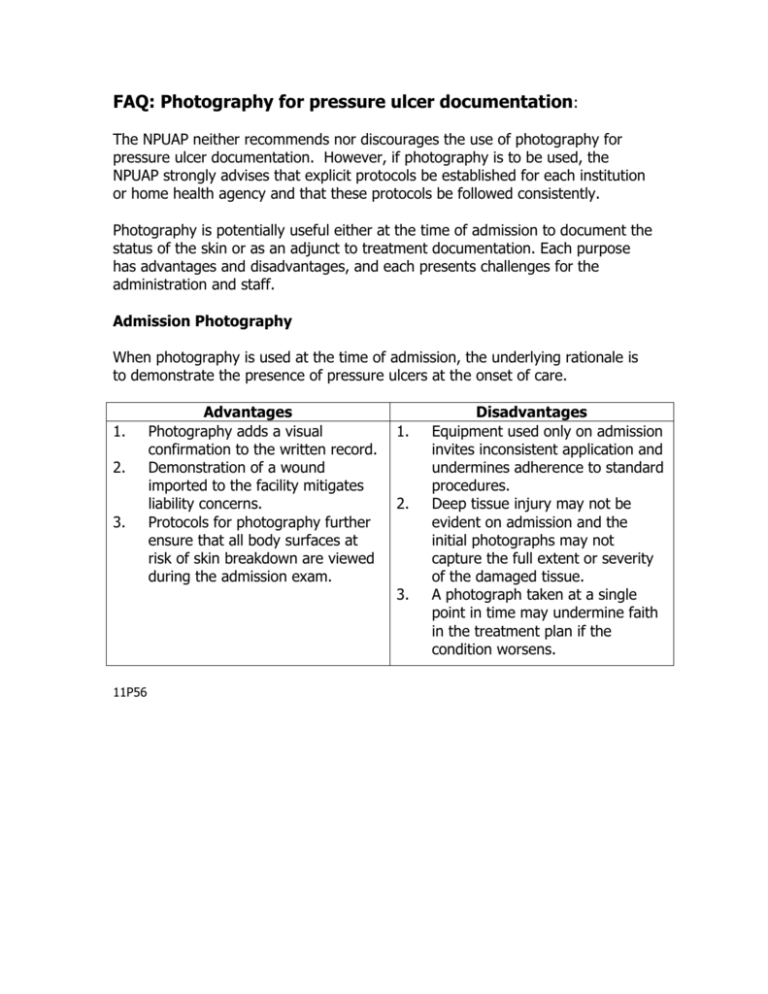
FAQ: Photography for pressure ulcer documentation: The NPUAP neither recommends nor discourages the use of photography for pressure ulcer documentation. However, if photography is to be used, the NPUAP strongly advises that explicit protocols be established for each institution or home health agency and that these protocols be followed consistently. Photography is potentially useful either at the time of admission to document the status of the skin or as an adjunct to treatment documentation. Each purpose has advantages and disadvantages, and each presents challenges for the administration and staff. Admission Photography When photography is used at the time of admission, the underlying rationale is to demonstrate the presence of pressure ulcers at the onset of care. 1. 2. 3. 11P56 Advantages Photography adds a visual confirmation to the written record. Demonstration of a wound imported to the facility mitigates liability concerns. Protocols for photography further ensure that all body surfaces at risk of skin breakdown are viewed during the admission exam. 1. 2. 3. Disadvantages Equipment used only on admission invites inconsistent application and undermines adherence to standard procedures. Deep tissue injury may not be evident on admission and the initial photographs may not capture the full extent or severity of the damaged tissue. A photograph taken at a single point in time may undermine faith in the treatment plan if the condition worsens. Documentation Photography Photography used as an adjunct to ongoing treatment provides a visual record to enhance documentation, but there are further issues that may arise: 1. 2. 3. Advantages Photography may offer a more 1. accurate means for assessment of wound dimensions and wound base characteristics over time. Rates of healing, and therefore measures of therapeutic efficacy, are more readily appreciated when the data are held in a visual format. A serial, visual record verifies staff 2. attention to the problem and mitigates liability concerns 3. Disadvantages Serial photography as a means for measuring pressure ulcer healing and to assess the efficacy of therapy requires a higher level of technological accuracy, and therefore, up-front costs for the equipment and ongoing costs for data storage. The demand for consistency underscores the need for staff training and credentialing. Photographs of large pressure ulcers can be inflammatory in a jury trial despite compliance with all reasonable standards. Other Issues Technical challenges are also different for the different applications. An admission photograph needs only to be able to visualize the skin surfaces, and there is greater flexibility in format, e.g. Polaroid® or regular photographic film, or digital photography (see below). The NPUAP strongly encourages that the protocol includes a means for patient identification, date and time marking and a sample measure (e.g. a 10 cm strip of paper tape) in each frame, and that the photographs become part of the medical record. Photographic standards for serial measurements used to document ongoing care needs to be more stringent. The NPUAP strongly recommends digital photography with a density of at least 1.5 megapixels, while >3 megapixels is preferable and offers the best ratio of picture clarity versus the cost of equipment. These protocols should include explicit criteria that standardize the equipment, aperture settings, distance from the wound and field of view, as well as a means for patient identification, date and time marking, and a sample measure in the frame of the picture. The use of a computer program for planography is another option to improve the accuracy of the photographic record and to objectively assess healing over time. Implementation of any program should include in-service training with demonstrated competencies and periodic studies of inter- and intra-rater consistency. Digital photography, videos and tele-medicine technology offers the additional capability of sharing the images with the attending physician, surgical consultants and wound care colleagues to better assess the current state of the wound, its progress towards healing and to develop plans for future interventions. Sharing photographs via e-mail requires special security provisions to assure compliance with HIPAA regulations. Although digital photography is preferred in most clinical circumstances, the ease with which the image can be manipulated renders this form of documentation inadmissible in many court cases. Therefore, if photography is to be used solely at the time of admission, a more permanent format is recommended. References: The articles below relate to the use of Polaroid® or regular photographic film and offer suggestions for protocol development applicable to all forms of photographic documentation: Houghton PE. Kincaid CB. Campbell KE. Woodbury MG. Keast DH. Photographic assessment of the appearance of chronic pressure and leg ulcers. Ostomy Wound Management. 46(4):20-6, 28-30, 2000 Apr. Krainski, M. Photography in nursing. AJN/September, 1998. 98(9), 16BB. Hood CA, Hope T and Dove P. Videos, Photographs and Patient Consent. BMJ. 1998;316:1009-1011 Campbell C. and Sacremento L. Photodocumentation Reverses Medicare Reimbursement Denial. Ostomy/Wound Management. 1995;3(41):18-23. Louis DT. Photographing Pressure Ulcers to Enhance Documentation. Decubitus. 1992;5(7):38-45. Kutcher J and Arnell I. Documentation of Skin Using Photography. Ostomy/Wound Management. 1992;Nov/Dec,38:23-28. Pieper B, Miklos C, Mance B and Adams W. Nurses Documentation About Pressure Ulcers. Decubitus. 1990;3(1):32-34. Tele-Medicine references: Halstead LS. Dang T. Elrod M. Convit RJ. Rosen MJ. Woods S. Teleassessment compared with live assessment of pressure ulcers in a wound clinic: a pilot study. Advances in Skin & Wound Care. 16(2):91-6, 2003 Mar-Apr. Kodza L, Scheurich A. The impact of telemedicine on outcomes of chronic wounds in the home care setting. Ost/Wound Manag 2000;46(10):48–53. Wirthlin D, et al.Telemedicine in vascularsurgery: Feasibility of digital imaging for remote management of wounds. J Vasc Surg June 1998;1089–100. Special thanks to the following who contributed to the development of this FAQ response: Laurie Rappl Pat Boynton Ben Pierce