Osteoporosis
advertisement

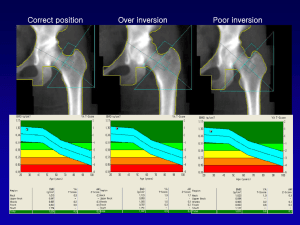
687314019 1 Estrogen or Raloxifene for Postmenopausal Osteoporosis Therapy? S.L. Silverman and M. Wong Depts. of Medicine and Rheumatology, Cedars-Sinai Medical Center, University of California Los Angeles, Beverly Hills, CA, U.S.A. *Lilly Research Laboratories, Eli Lilly and Company, Indianapolis, IN, U.S.A. Summary Osteoporotic vertebral fractures cause increased morbidity and mortality in postmenopausal women. Estrogen alone (ERT, estrogen replacement therapy) or combined with progestin (HRT, hormone replacement therapy), and raloxifene, a selective estrogen receptor modulator (SERM), are therapeutic options for osteoporosis. The clinical trial evidence to support fracture efficacy of ERT/HRT and raloxifene are reviewed. Introduction In postmenopausal osteoporosis, declining estrogen levels produce accelerated bone loss, which lead to decreased bone mass and microarchitectural deterioration, and an increased risk of fractures, particularly in the vertebrae and hip [1]. Between 20 to 25% of women aged 50 yr and older have one or more vertebral fractures [2]. Clinical hip or spine fractures increases the mortality risk 6.7- and 8.6-fold respectively [3]. Pre-existing vertebral fractures increases morbidity and mortality [4] and decreases the quality of life [5]. Women with a pre-existing vertebral fracture have a 5-fold increased risk of a new vertebral fracture within the following year [6]. Therefore, the goal of osteoporosis therapy is prevention of new fractures. Materials and Methods For decades, ERT and HRT have been used for management of postmenopausal symptoms. Observational studies in postmenopausal women are often cited as evidence to support the use of ERT/HRT for osteoporosis, as there are very few well-designed clinical trials which examined fracture efficacy. Results from observational studies are influenced by selection bias and adherence bias, as women who use ERT/HRT tend to have a better health profile and follow physicians’ instructions compared to women who do not use these drugs [7]. Currently, demonstration of fracture risk reduction in long-term prospective double-blind, placebo-controlled, randomized clinical trials is required for regulatory approval of newer drugs such as raloxifene. These clinical trials last for at least 3 years, involve large numbers of patients, and require confirmation of vertebral fractures with radiographs. Such clinical trials are expensive, so many smaller studies use intermediate markers, such as bone mineral density (BMD). Low BMD and the presence of existing fractures both predict increased risk of future fractures, but increase in BMD with antiresorptive agents is a poor predictor of actual fracture risk reduction with therapy [8]. This review compares the clinical 687314019 2 trial evidence to support the use of ERT/HRT or raloxifene for reducing the risk of osteoporotic fractures. Results Despite the multitude of published studies on ERT/HRT in postmenopausal women, only 15 observational studies included fracture as a study endpoint [9]. These trials suggest that postmenopausal women who used ERT/HRT have reduced fracture risk compared with case-controls. In the Study of Osteoporotic Fractures, decreased fracture risk was associated with current or prolonged use of ERT/HRT [10]. The 3-year Postmenopausal Estrogen/Progestin Interventions trial of 875 women showed significant increases in spinal (5.3%-6.8%) and hip BMD (3.4%), compared with placebo, but the incidence of fractures was not significantly different and not assessed in radiographs [11]. Clinical fractures were not significantly different between HRT and placebo in the Heart and Estrogen/Progestin Replacement Study of 2673 women at low risk for osteoporosis [12]. HRT did not significantly reduce the overall nonvertebral fracture risk [13]. In a 1-year clinical trial of 75 women with osteoporosis, the estrogen therapy significantly decreased the risk of vertebral fractures by 61% when expressed as events per person-year [14]. This evidence, along with many studies which show increased BMD, suggest that ERT/HRT may reduce fracture risk. Raloxifene increased spine BMD by 2.6% compared with placebo at 3 years in 1145 healthy postmenopausal women [15]. In the 3-year randomized, double-blind, placebo-controlled Multiple Outcomes of Raloxifene Evaluation (MORE) trial of 7705 postmenopausal women with osteoporosis [16], raloxifene 60 mg/d significantly decreased the risk of painful clinical vertebral fractures by 68% in the first year [17]. In women without pre-existing vertebral fractures, raloxifene 60 mg/d decreased the risks of new vertebral fractures by 55% [18], and of multiple (2) new vertebral fractures by 93% [19]. In women with pre-existing vertebral fractures, who are at greater risk of subsequent fractures, raloxifene 60 mg/d decreased the risk of new vertebral fractures by 30% at 3 years [16]. Long-term compliance with osteoporosis therapy is necessary to achieve benefits on fracture prevention. ERT/HRT has beneficial effects on treating postmenopausal symptoms, such as hot flashes, but the occurrence of breast tenderness and vaginal bleeding may limit adherence [20]. The occurrence of breast pain and vaginal bleeding with raloxifene was similar to placebo, while the incidence of hot flashes was increased [16]. More women discontinued use of estrogen (72%) compared to raloxifene (50%) after 2 years, with a notable difference in discontinuation evident at 6 months after the initial prescription [21]. Conclusions The beneficial effects on postmenopausal symptoms are well-known but the putative fracture efficacy of ERT and HRT is suggested by several observational studies. The MORE trial demonstrated that raloxifene decreases vertebral fracture 687314019 3 risk in postmenopausal women with osteoporosis as early as the first year. Compliance with raloxifene is superior to that for ERT/HRT. References 1. GENANT HK, et al. Interim Report and Recommendations of the World Health Organization Task-Force for Osteoporosis. Osteoporos Int 10: 259-64; 2000. 2. MELTON LJ 3rd. Epidemiology of spinal osteoporosis. Spine 22: 2S-11; 1997. 3. CAULEY JA, et al. Risk of mortality following clinical fractures. Osteoporos Int 11: 556-6; 2000. 4. KADO DM, et al. Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med 1999; 159: 1215-20. 5. SILVERMAN SL, et al. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum 2001; 44: 2611-9. 6. LINDSAY R, et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001; 285: 320-3. 7. BARRETT-CONNOR E, GRADY D. Hormone replacement therapy, heart disease, and other considerations. Ann Rev Public Health 1998; 19:55-72: 5572; 1998. 8. SARKAR S, et al. Relationships between bone mineral density and incident vertebral fracture risk with raloxifene therapy. J Bone Miner Res 17: 1-10; 2002. 9. MARCUS R, et al. Antiresorptive treatment of postmenopausal osteoporosis: comparison of study designs and outcomes in large clinical trials with fracture as an endpoint. Endocr Rev 23: 16-37; 2002. 10. CAULEY JA, et al. Bone mineral density and risk of breast cancer in older women: the study of osteoporotic fractures. JAMA 276: 1404-8; 1996. 11. PEPI TRIAL WRITING GROUP. Effects of hormone therapy on bone mineral density: results from the postmenopausal estrogen/progestin interventions (PEPI) trial. JAMA 276: 1389-96; 1996. 12. HULLEY S, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA 280: 605-13; 1998. 13. KOMULAINEN MH, et al. HRT and Vit D in prevention of non-vertebral fractures in postmenopausal women; a 5 year randomized trial. Maturitas 31: 45-54; 1998. 14. LUFKIN EG, et al. Treatment of postmenopausal osteoporosis with transdermal estrogen. Ann Intern Med 117: 1-9; 1992. 687314019 4 15. JOHNSTON CC Jr, et al. Long-term effects of raloxifene on bone mineral density, bone turnover, and serum lipids in early postmenopausal women. 3year data from two double-blind, randomized, placebo-controlled trials. Arch Int Med 160: 3444-50; 2000. 16. ETTINGER B, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: Results from a 3-year randomized clinical trial. JAMA 282: 637-45; 1999. 17. MARICIC M, et al. Raloxifene 60 mg/day has effects within 12 months in postmenopausal osteoporosis treatment and prevention studies. Arthritis Rheum 43: S197; 2000. 18. LUFKIN EG, et al. The role of selective estrogen receptor modulators in the prevention and treatment of osteoporosis. Rheum Dis Clin North Am 27: 16385; 2001. 19. LUFKIN EG, et al. Raloxifene decreases the relative risk of multiple (>2) new vertebral fractures in postmenopausal women with osteoporosis: Results from the MORE study. Abstract P-021, North American Menopause Society meeting, New Orleans, 2001. 20. STUENKEL C, BARRETT-CONNOR E. Hormone replacement therapy: where are we now? West J Med 171: 27-30; 1999. 21. KAYSER J, et al. Postmenopausal hormonal support: discontinuation of raloxifene versus estrogen. Menopause 8: 328-32; 2001.