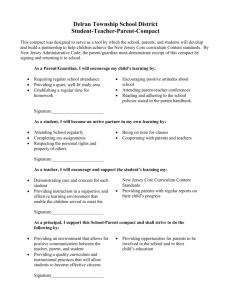
document approval & tracking
advertisement

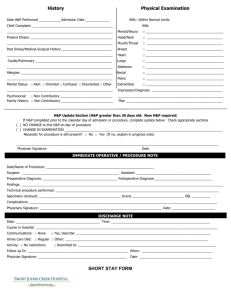
Applies To: All HSC Hospitals Responsible Department: Office of Clinical Affairs Documentation of Clinical Activities by Medical Staff and House Staff Title: Patient Age Group: ( ) N/A (x ) All Ages Policy ( ) Newborns ( ) Pediatric ( ) Adult DESCRIPTION The purpose of this policy is to ensure that Medical Staff and House Staff documentation of clinical activities supports and promotes: 1) high-quality clinical care; 2) patient safety and quality improvement; 3) accurate billing for provided services; 4) compliance with regulatory requirements such as Medicare conditions of participation, JCAHO standards, LCME and ACGME requirements, and state and federal law. DETAILED POLICY STATEMENT 1. General Documentation Principles a. Medical Staff and House Staff shall chart legibly and completely, and shall authenticate each entry by signature, date, and time. All orders shall be authenticated by the ordering Medical Staff or House Staff by signature, date, and time. b. Any addenda to previously recorded entries shall be made under a separate entry, and shall be authenticated by signature, date, and time the addendum was made. c. Documentation of routine clinical encounters shall be completed in a timely manner, preferably immediately following the provision of care, but no later than 24 hours after the clinical encounter. This includes completion of both the dictated or written clinical entry and any relevant billing. d. Clinical documentation shall contain information to justify the patient’s admission, continued hospitalization, treatment, and diagnosis; and shall document the patient's progress and response to treatment. e. Attending Physicians and other Medical Staff shall document their physical presence during the key portion of a service provided by a House Staff in accordance with regulatory and billing requirements. f. Medical students may perform history and physical examinations as appropriate, and will make appropriate notations in the medical record. The notation must be signed by the supervising House Staff or Attending Physician. The supervising physician will be required to cosign the last page of the history and physical examination form only. 2. Documentation of Medical History & Physical Examination (H&P) a. The minimal contents of an admitting inpatient H&P shall be: i. those elements of the H&P that are immediately pertinent to the chief complaint or presenting problem; ii. the history of present illness; relevant past medical history; medications; and allergies; iii. vital signs and pain assessment (which may he performed by a nurse or other qualified practitioner and reviewed by the Attending Physician); Title: Documentation of Clinical Activities by Medical Staff and House Staff Owner: Associate Dean for Clinical Affairs Effective Date: 02/15/2006 Page 1 of 6 iv. examination of the cardiovascular system, pulmonary system, and abdomen; v. additional elements of the H&P necessary for the safe and effective treatment of the patient. b. The minimal contents of an outpatient H&P shall be: i. those elements of the H&P that are immediately pertinent to the patient’s chief complaint or presenting problem; ii. additional elements of the H&P necessary for the safe and effective treatment of the patient. c. An admission H&P shall be completed and dictated or electronically entered by the Attending Physician, house officer, or allied health practitioner (AHP)no more than thirty days before or twenty-four hours after a patient’s admission for a procedure or an inpatient stay. i. If the admission H&P was completed prior to the patient’s admission, the admitting practitioner shall: 1. document at admission that the previous H&P is to be used as the admitting H&P, and either state that there are no significant updates, or document any significant, and 2. verify that the earlier H&P is available in the patient’s medical record. d. A timely H&P, as delineated above, must be present in the medical record of every patient prior to a surgery or an invasive procedure, except in emergencies. e. The Attending Physician may delegate all or part of the H&P to other qualified practitioners, but the Attending Physician must review and sign sign the H&P, and assumes full responsibility for these delegated activities. 3. Inpatient Progress Notes a. At University Hospital and Children’s Hospital, progress notes shall be entered on the chart by the assigned House Staff member at least daily. b. At University Hospital and Children’s Hospital, progress notes shall be entered on the chart by the Attending Physician at least daily. c. Frequency of progress notes at other UNM HSC component hospitals shall be determined by the component hospital’s policy. d. More frequent notes may be indicated by the patient’s clinical condition. e. Under unusual circumstances, less frequent notes may be justified. Lesser frequency of notes shall be approved in writing by the Attending Physician’s Department Chair. 4. Discharge Summaries and Abbreviated Hospital Summaries a. Discharge summaries shall be dictated or written within 48 hours after discharge. b. A discharge summary is required for all discharges following inpatient stays, except for normal newborns who stay for maternal reasons. 5. Operative and Procedural Reports a. All operative and procedural reports shall be written or dictated immediately after the surgery or invasive procedure and shall be available within twenty-four hours. b. All operative and procedural reports written or dictated by a House Staff shall be reviewed for accuracy and cosigned by the supervising Medical Staff. c. Prior to surgery or procedures (except in emergencies), oral surgeons and dentists must record evidence of a thorough review of the oral cavity to include a detailed Title: Documentation of Clinical Activities by Medical Staff and House Staff Owner: Associate Dean for Clinical Affairs Effective Date: 02/15/2006 Page 2 of 6 description of the dental problem, oral examination and pre-operative diagnosis. Operative reports should include statements regarding technique, findings, and the specific number of teeth and/or fragments. 6. Use of a Signature Stamp as an Official Signature a. Physicians who wish to use a signature stamp as their official signature shall: i. sign and have notarized a letter indicating their intention to use a signature stamp as their official signature (see the sample letter appended to this document), including samples of their usual signature and the signature stamp; ii. submit the original of this letter to the Office of Medical Staff Affairs to be filed in their Medical Staff file; iii. submit a copy of this letter to the office of Health Information Management (Medical Records) to be kept on file in that office. 7. Medical Records Completions and Delinquencies a. The Attending Physician will certify the quality and accuracy of the medical record's content. This record will include (when applicable): identifying data, complaint, history and physical examination, special reports (consultations, clinical laboratory, imaging, diagnostics), provisional diagnosis, medical or surgical treatment, operative report, pathological findings, progress notes, evidence of appropriate informed consent, final diagnosis, condition on discharge, instructions on physical activity, diet restriction, follow-up plan, medication list and autopsy (when applicable). b. A medical record is considered to be complete when all elements have been addressed and a signed discharge summary or abbreviated hospital summary is present. Any medical record not completed within fourteen (14) days of discharge of the patient, and without unusual extenuating circumstances that would preclude completion of the medical record, is defined as a delinquent medical record. c. If any House Staff or Medical Staff has delinquent medical records, and the member’s Department Chair has not been advised of any unusual extenuating circumstances that have precluded chart completion by the responsible physician (such as administrative, sick, bereavement or annual leave) the delinquent Staff may be placed on temporary suspension from training or patient care at UNMHSC until such time as all available delinquent medical records are completed and verified by Health Information Management (Medical Records). d. Such suspensions from training or patient care must occur in compliance with the UNM House Officers and the University Regulation and Benefit Manual, or the Medical Staff Bylaws, as applicable. APPLICABILITY This policy is applicable to all UNMHSC Medical Staff members and House Staff members. REFERENCES UNMHSC Medical Staff Bylaws University of New Mexico House Officers and the University Regulation and Benefit Manual UNMHSC Policy, Prohibited Abbreviations Title: Documentation of Clinical Activities by Medical Staff and House Staff Owner: Associate Dean for Clinical Affairs Effective Date: 02/15/2006 Page 3 of 6 UNMHSC Policy, Supervision of Physicians and Dentists in Training 42 CFR 482 Medicare Conditions of Participation and subsequent clarifying documents DEFINITIONS 1) ‘Signature’ – A signature is a legible and distinctive mark that identifies a particular individual. For the purposes of this document, examples of acceptable signatures include: a handwritten name (note that it must be legible); a legibly-printed name accompanying a less legible handwritten name; a signature stamp; an individual number accompanying a handwritten name (e.g., pager number, billing number); or an electronic medical record caregiver identification generated from an individual, password-protected login. 2) ‘Attending Physician’ – The attending physician is the Medical Staff member primarily responsible for the care of the patient. 3) ‘Allied Health Practitioner (AHP)’ – For the purposes of this document, an allied health practitioner is an advanced practice nurse or physician assistant who is a member of the Associate Medical Staff and the patient’s immediate treatment team. 4) ‘Invasive Procedure’ – An invasive procedure is a significant clinical procedure which involves puncture or incision of the skin; insertion of an instrument or foreign material into the body; administration of anesthesia; sedation; such procedures may include, but are not limited to surgeries; percutaneous aspirations and biopsies; cardiac and vascular catheterizations; laser procedures; endoscopies; angioplasties; implantations; electroconvulsive therapy; and conscious sedation. Invasive procedures do not include such things as simple venipuncture (‘phlebotomy’), routine placement of a Foley catheter, or routine placement of a peripheral IV. SUMMARY OF CHANGES Updated 2/11/08 KEY WORDS Documentation, medical record, delinquent medical record, operative report, discharge summary, progress note, signature, medical staff, house staff, medical history, physical examination, stamp Title: Documentation of Clinical Activities by Medical Staff and House Staff Owner: Associate Dean for Clinical Affairs Effective Date: 02/15/2006 Page 4 of 6 RESOURCES/TRAINING Resource/Dept Office of Clinical Affairs Health Information Management Internet/Link (505) 272-2525 (505) 272-0477 DOCUMENT APPROVAL & TRACKING Item Owner Committee(s) Nursing Officer Medical Director/Officer Official Approver Contact Associate Dean for Clinical Affairs Clinical Operations PPG Committee UNMHSC Medical Executive Committee Approval 02/08/08 xx/xx/2008 Judy Spinella, MBA, MSN, RN, Chief Nursing Officer Robert Bailey MD, Associate Dean for Clinical Affairs 02/11/08 Y Robert Katz, MD, Vice President for Clinical Affairs [Day/Mo/Year] Official Signature Official Approver Date Steve McKernan, Vice President for Clinical Operations Official Signature [Day/Mo/Year] Effective Date Origination Date Issue Date Item Owner Clinical Operations P&P Coordinator Contact Associate Dean for Clinical Affairs xxx xxx [Day/Mo/Year] Date Committee(s) UNMHSC Medical Executive Committee 02/xx/2008 Y Legal (Required) Vicki Hunt, HSC Legal Robert Bailey, MD; Associate Dean for Clinical Affairs; Office of Clinical Affairs Y Official Approver Official Signature [Day/Mo/Year] Effective Date Origination Date Issue Date xxx xxx [Day/Mo/Year] Clinical Operations P&P Coordinator Approval Y ATTACHMENTS 1) Sample letter for Medical Staff use of a Signature Stamp as an Official Signature Title: Documentation of Clinical Activities by Medical Staff and House Staff Owner: Associate Dean for Clinical Affairs Effective Date: 02/15/2006 Page 5 of 6 Attachment 1: Sample letter for Medical Staff use of a Signature Stamp as an Official Signature University Hospital 2211 Lomas Boulevard, NE Albuquerque, New Mexico 87106 [Date] To: Cc: From: Re: Office of Medical Staff Affairs Office of Health Information Management (Medical Records) John Doe, MD Use of a Signature Stamp as my official signature This is to notify you of my intention to use a Signature Stamp as my official signature on Medical Records. I am the only person in possession of this Stamp, and am the only one who will be using this Stamp. Below is a sample of my usual signature, and that of the Signature Stamp. Sincerely, Name: John Doe, MD Department: Surgery [Usual Signature] [Signature Stamp] Title: Documentation of Clinical Activities by Medical Staff and House Staff Owner: Associate Dean for Clinical Affairs Effective Date: 02/15/2006 Page 6 of 6