download-link-title - York General Practice VTS
advertisement

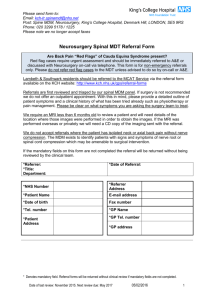
c/o NHS Barnsley Hillder House 49-51 Gawber Road Barnsley, S75 2PY Tel: (01226) 433 674 Fax: (01226) 433 797 www.yhscg.nhs.uk Our Ref: KC/MG Please ask for: Kim Cox 28 October 2009 To: Members of the West Yorkshire Neurosciences Commissioning Group Dear Colleague Re: Referral Guidelines to Neurosurgery A paper was presented to the February 2009 SCG Board meeting which detailed problems associated with access to neurosurgical services in Yorkshire and the Humber. The paper focussed on two approaches to addressing the problem; reducing inappropriate referrals and increasing capacity. To facilitate the reduction of inappropriate referrals the paper included referral guidelines to neurosurgery for patients with simple lumbar or cervical discogenic or degenerative spinal disease. The Board agreed to adopt the guidelines, which had been agreed between the three neurosurgical centres in Yorkshire and the Humber. The Specialised Commissioning Team (SCT) is working with providers to ensure the guidelines are incorporated into Directories of Services. As part of the implementation of the guidelines, the West Yorkshire Neurosciences Commissioning Group agreed to work with the SCT to ensure local GPs are aware of the guidelines. It was agreed that commissioners would work with their GPs in the most appropriate way to implement the guidelines and that this would be supported by a series of statements indicating why the guidelines had been produced and what they were designed to achieve. These statements are given below. I would be grateful if you would now undertake the necessary work with your GPs to ensure the guidelines are implemented. There is an identifiable and ongoing increase in referrals to neurosurgical services across the patch, but particularly to the Leeds service Referrals for spinal problems constitute a significant proportion of the work being sent. Only a relatively small percentage of the patients seen are appropriate for and will go on to have a surgical procedure (currently 20% or less), hence 80% of patients would be more appropriately managed by someone other than a neurosurgeon D:\687313981.doc 1 Neurosurgical colleagues consider that if referrers adhere to a clear set of referral guidelines for patients with spinal discogenic or degenerative disease patients are much more likely to be managed by the appropriate services Referral guidelines have been produced and agreed and are attached. Advice is included on the management of patients who are not appropriate for referral to a neurosurgeon. I would be grateful if you would inform me of the action you have taken to implement these guidelines by the end of November. Should you have any questions please do not hesitate to contact me. Yours faithfully Kim Cox Kim Cox Cc Abigail Tebbs Peter Barnaby Vicki Woodhead D:\687313981.doc 2 Referral Guidelines to Neurosurgery Discogenic/Degenerative Spinal Disease for Patients with Simple Lumbar or Cervical Who Should be Referred? 1. Acute severe radicular arm or leg pain, not showing any improvement with conservative measures (such as physiotherapy) by six weeks following onset. Note that some improvement is likely to imply eventual resolution without requirement for surgery. Pain will be in a nerve root distribution. Neurological symptoms (paraesthesia, numbness and/or muscular weakness) will be in a nerve root distribution and normally exacerbated by cough and/or movement. Progressive neurological symptoms and/or severe radicular pain are indications for urgent referral. 2. Refractive longer term radicular pain (i.e. greater than three months) significantly interfering with lifestyle, disturbing sleep, or causing extended periods off work. 3. Significant spinal claudication, (i.e., radiating leg pain/paraesthesia/numbness coming on with walking and distance-limiting). Pain progression is normally from buttocks to the periphery. Relief is gained by rest and bending forwards. Neurological symptoms (paraesthesia, numbness and/or muscular weakness) also resolve with rest. Peripheral pulses are normal. Urgent Referrals to the Neurosurgery On-call Team 1. Cauda Equina Syndrome. Symptoms include bilateral radiating leg pain with sphincter disturbance and reduced perianal sensation and perineal numbness. Also progressive motor weakness affecting more than one nerve root and/or gait disturbances. Referral must include the findings from perineal examination. 2. Severe motor weakness accompanying an acute onset lumbosacral radicular pain syndrome, i.e., inability to plantar flex (S1) or inability to dorsiflex (‘foot drop’, L5). 3. Patients with signs of myelopathy. All patients should be referred, whether asymptomatic or not, with positive long tract signs (see below) or when an MRI has been done and where, even in the absence of long tract signs, there is cord signal change at a stenotic spinal level. Symptoms include numb, clumsy hands, jumping, stiff legs, falls, poor balance and urinary frequency. Referrals to be Marked Urgent 1. Patients with neurological symptoms who fall into one or more of the following categories: Presentation younger than age 20 Onset of symptoms following violent trauma (e.g. RTA; fall from a height) Constant, progressive non-mechanical pain Thoracic pain Past medical history of carcinoma Patients who are using systemic steroids History of HIV and/or drug abuse Patients who are systemically unwell Patients with unexplained weight loss Patients with inflammatory disorders such as ankylosing spondylitis Who Shouldn’t be Referred? 1. Patients with referred pain. For the purposes of differential diagnosis, referred arm, leg or neck pain is more generalised in distribution and does not follow a specific nerve root distribution. Pain does not generally spread below the elbow or knee. 2. Patients with degenerative neck or back pain generally have no surgically remedial cause and so should not be referred. Patients should be managed with analgesia, advice and physiotherapy. 3. Patients with non-specific neurological symptoms/somatisation disorder. Such patients should be referred to a neurologist or to the pain clinic. 4. Where radicular pain is significantly improving or resolved. 5. Where there is residual dermatomal numbness following a previous radicular pain episode. 6. Where the patient does not want any surgery (other than patients who are considered to be myelopathic). Long tract signs (also known as upper motor neuron or pyramidal signs) 1. Should be done/commented on for all patients with cervicovertebral or cervical radicular pain as a screen for an underlying myelopathy. 2. Signs to look for include: hyper-reflexia, Babinski, clonus, crossed-adductor reflexes, Hoffman’s, and loss of fine finger movements. D:\687313981.doc 3 On Making a Referral… 1. Arrange an MRI scan of the relevant spinal area to be available by the time of appointment (or if not possible, give in the referral letter sufficient information for such an investigation to be pre-ordered, e.g., pattern of pain radiation, any contraindications to MRI such as pacemaker). If scans have been performed prior to first out patient appointment, the images (preferably on CD) should accompany the referral letter. The scan report should, if possible, accompany the images but should not be a substitute for them. 2. Note that if a patient has had previous spinal surgery and an MRI is requested, the details of the surgery should be provided on the request, and in particular the request should be marked as requiring contrast/gadolinium. 3. Prescribe a trial of gabapentin if radicular symptoms and/or trial of amitryptilene 25mg ~ 6pm daily for sleep disturbing vertebral pain, in addition to standard analgesics (i.e., compound analgesic and strong anti-inflammatory such as diclofenac 50mg TDS). Tell patients about Transcutaneous Electrical Nerve Stimulation. Management of those Patients who should not be Referred Patients with either acute or chronic neck or back pain and no neurological signs and symptoms rarely have a surgically remedial problem. Such patients need a clear and informative explanation of why neurosurgical intervention will not be of benefit. They are then best managed in primary care through a combination of advice, appropriate medication and access to physiotherapy and chronic pain specialists. Referrers who have concerns regarding individual patients are encouraged to contact the neurosurgical department for advice prior to referral. D:\687313981.doc 4 SPINAL PATIENTS Referrers who have concerns regarding individual patients are encouraged to contact the neurosurgical department for advice prior to referral CAUDA EQUINA ACUTE / SEVERE RADICULAR PAIN eg. Sciatica, brachalgia PROGRESSIVE NEUROLOGICAL SYMPTOMS eg. Foot drop REFRACTORY TO OPIATES INCREASE ANALGESIA LOCAL A+E DEPT FOR EMERGENCY SCAN CHRONIC / REFRACTORY RADICULAR PAIN < 6 WEEKS INCREASE ANALGESIA ORGANISE MRI * SPINAL CLAUDICATION > 6 WEEKS PATIENT IS FIT FOR SURGERY AND WILLING TO CONSIDER AN OPERATION INCREASE ANALGESIA ORGANISE MRI * ORGANISE MRI * ORGANISE MRI * RED FLAGS NO RED FLAGS FAXED REFERRAL FLEXION / EXTENSION X RAYS NORMAL ABNORMAL ANALGESIA + PHSYIO SCAN POSITIVE EMERGENCY ON CALL REFERRAL BACK / NECK PAIN MYELOPATHY FAXED REFERRAL PRIMARY CARE REVIEW OUTPATIENT REFERRAL OUTPATIENT REFERRAL OUTPATIENT REFERRAL CHRONIC PAIN SPECIALIST REFERRAL OUTPATIENT REFERRAL *Arrange an MRI scan of the relevant spinal area to be available by the time of appointment (or if not possible, give in the referral letter sufficient information for such an investigation to be pre-ordered, e.g., pattern of pain radiation, any contraindications to MRI such as pacemaker). If scans have been performed prior to first out patient appointment, the images (preferably on CD) should accompany the referral letter. Note that if a patient has had previous spinal surgery and an MRI is requested, the details of the surgery should be provided on the request, and in particular the request should be marked as requiring contrast/gadolinium. D:\687313981.doc 5 NOTES ON SPINAL REFERRALS RED FLAGS SPINAL CLAUDICATION Presentation younger than age 20 Onset of symptoms following violent trauma (e.g. RTA; fall from a height) Thoracic pain Past medical history of carcinoma Patients who are using systemic steroids History of HIV and/or drug abuse Patients who are systemically unwell Patients with unexplained weight loss Persistent severe restriction of lumbar flexion Patients with inflammatory disorders such as ankylosing spondylitis Radiating leg pain, paraesthesia or numbness coming on with walking and distance-limiting. Pain progression is normally from buttocks to the periphery. Relief is gained by rest and bending forwards. Neurological symptoms (paraesthesia, numbness and/or muscular weakness) also resolve with rest. Peripheral pulses are normal. CAUDA EQUINA SYNDROME MYELOPATHY (cord compression) Symptoms include numb, clumsy hands; jumping, stiff legs; falls, poor balance and urinary frequency. Bilateral radiating leg pain Sphincter disturbance Reduced perianal sensation Perineal numbness Progressive motor weakness affecting more than one nerve root and/or gait disturbances Examine for long tract signs (also known as upper motor neuron or pyramidal signs) Signs to look for include: hyper-reflexia, Babinski, clonus, crossedadductor reflexes, Hoffman’s, and loss of fine finger movements. Referral must include the findings from perineal examination RECOMMENDED ANALGESIC REGIME Prescribe a trial of gabapentin if radicular symptoms and/or trial of amitryptilene 25mg ~ 6pm daily for sleep disturbing vertebral pain, in addition to standard analgesics (i.e., compound analgesic and strong anti-inflammatory such as diclofenac 50mg TDS). Tell patients about Transcutaneous Electrical Nerve Stimulation D:\687313981.doc 6