ORIGINAL ARTICLE INCIDENCE OF SURGICAL SITE INFECTION
advertisement

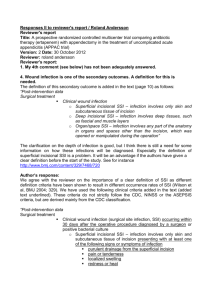
ORIGINAL ARTICLE INCIDENCE OF SURGICAL SITE INFECTION IN CLEAN ORTHOPAEDIC PROCEDURES LIKE DYNAMIC HIP SCREW SURGERY: A LIAISON BETWEEN SURGEONS AND INFECTION CONTROL PERSONNEL Archana G1, Hanume Gowda S. N2 HOW TO CITE THIS ARTICLE: Archana G, Hanume Gowda S. N. “Incidence of surgical site infection in clean orthopaedic procedures like dynamic hip screw surgery: a liaison between surgeons and infection control personnel”. Journal of Evolution of Medical and Dental Sciences 2013; Vol2, Issue 31, August 5; Page: 5748-5754. ABSTRACT: Postoperative SSI in orthopaedic procedures involving implants is one of the most costly complications. Studies estimated that SSIs prolong total hospital stays by a median of two weeks per patient. Moreover, orthopaedic patients with SSIs have substantially greater physical limitations and significant reductions in their quality of life. Aim was to establish infection control policy and assess the incidence of SSIs in DHS and also validate the infection control policy of our hospital by comparing rates with already published reports. The study was conducted at a multispecialty tertiary care centre. 70 patients with intertrochanteric fracture undergoing DHS surgery during the period of Jan-2011 to Dec-2011 with an NHSN risk index of 0 were enrolled into the study. A minimum follow up was for 1 year. Of the 70 surgeries, 1(1.4%) Superficial incisional SSI was noticed and it settled down with debridement and antibiotics. No deep or organ space infection was noted. Our result was favorably comparable with the NHSN data between 2006-2008 showed 0.67-2.4 per 100 operations and also other similar published reports. CONCLUSION: “BUGS ARE AHEAD OF HUMANS”. We have to evolve ourselves beyond drug therapy to fight SSI. Prevention of SSIs is based on structured protocols, which are evolved by the hospital infection control committee. The policy has to be specific to the hospital based on broad guideline already published. A more holistic approach with a dedicated team to monitor the infection control protocols and the infection rates along with antibiotic policy is order of the day. There is a scope for improvement as ever and the goal is to reduce the SSI incidence to near 0%. Based on our findings we can with confidence say that we can reduce the incidence of SSIs to near 0% with a good protocol of infection control policy. INTRODUCTION: Postoperative SSI (Surgical Site infection) in orthopaedic procedures involving implants is one of the most costly complications. This is due to hospital readmissions, extended length of stay at the hospital, the need for additional procedures( removal and re implantation of implanted hardware), convalescent or nursing home care between procedure, and significant increases in direct hospital cost(eg, prolonged antimicrobial therapy). It also affects the patient’s social and economic status1&2. One study estimated that orthopaedic SSIs prolong total hospital stays by a median of two weeks per patient, approximately double readmission rates, and increase healthcare costs by more than 300%. Moreover, patients with orthopaedic SSIs have substantially greater physical limitations and significant reductions in their quality of life.1 In light of the serious consequences, antimicrobial prophylaxis is well accepted in procedures involving the implantation of foreign materials.3, 4 Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5748 ORIGINAL ARTICLE Skin flora is the most frequent organisms involved in SSIs in orthopaedic procedures. The most common pathogens in orthopaedic procedures are S. aureus, gram- negative bacilli, coagulasenegative staphylococci (including S. epidermidis) and B-hemolytic streptococci.5-10 Contributing factors to SSIs are the bacterial bio-film which confers antimicrobial resistance and makes antimicrobial penetration difficult. 11-15 There has been an increased awareness and drive towards preventing this menace. A liaison between the Infection control in charge and the surgeons has become a mandatory activity to track the surgical site infections through aggressive surveillance. NEED FOR STUDY There are no published prospective studies regarding SSI in orthopaedic surgeries. With a standardised protocol on infection prevention we want to assess the incidence of infection in orthopaedic surgeries with implant. This study is to assess the utility of the protocols put forward towards the prevention of SSs in our set up. OBJECTIVES OF THE STUDY To assess the incidence of SSIs in DHS To validate the infection control policy of our by comparing rates with already published reports MATERIALS AND METHODS: Criteria for patient selection: 1. Proximal femoral fractures undergoing DHS (DYNAMIC HIP SCREW) surgery. 2. Done by a single surgeon or under his guidance. 3. A minimum follow-up of 1year after surgery were selected. 4. NHSN (National Healthcare Safety Network) Risk Index (Table- 1) of 0 falling into the above criteria during the period of Jan 2011-dec 2011. -Operating time maximum of lees than 2hrs. -Clean (non-contaminated) case -ASA grade 2 or less Table-1-NHSN Risk Stratification was adopted which includes# 1. Operation lasting more than the duration of cut point hours, where the duration cut point is the approximate 75th percentile of the duration of surgery in minutes for the operative procedure, rounded to the nearest whole number of hours. 2. Clean or clean Contaminated (Class 3) or Dirty/infected (Class 4) wound class. 3. ASA classification of 3 or less(table-2) The patient’s SSI risk category is simply the number of these factors present at the time of surgery. Each criteria carrying 1 point. # Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5749 ORIGINAL ARTICLE Table-2 Physical Status Classification, American Society of Anaesthesiologists _______________________________________________________________________________________________________________ Code Patient’s Preoperative Physical Status 1 Normally healthy patient 2 Patient with mild systemic disease 3 Patient with severe systemic disease that is not incapacitating 4 Patient with an incapacitating systemic disease that is a constant threat to life 5 Moribund patient who is not expected to survive for 24 hours with or without operation Note: The above is the version of the ASA Physical Status Classification System that was current at the time of development of, and still is used in, the NNIS Risk Index. Meanwhile, the American Society of Anaesthesiologists has revised their classification system; the most recent version is available at http://www.asahq.org/profinfo/physicalstatus.html. _______________________________________________________________________________________________________________ Follow up was undertaken by the Infection control nurse (ICN). A structured SSI data sheet (Table3) was prepared to collect data. The operating surgeon, ICN and the clinical microbiologist were directly involved in collecting the data as a team. _______________________________________________________________________________________________________________ Table-3 Orthopedic SSI Worksheet Procedure __________________________________________________________________________________________________ Patient name_____________________________ ID _______________ Type of infection: Superficial______________________ Deep ______________ Organ space ___________________ Radiological evidence of infection ________________________________________________________________________ Date of surgery_______________________ Surgeon ________________________________ Purulent drainage? Yes/No.____________________________________________________ Antibiotic therapy? Yes/No. Antibiotic _______________________________________ Pain ________________ Redness________________ Other symptoms________________ Type of implant if applicable _______________ Blood loss ______________________ Transfusion? Yes/No.___________________________________________________________ Date of infection_______________ Date of admission to hospital _______________ Culture data # 1 date__________ Pathogen______________________________________ Other culture data _________ Date of readmission if applicable __________ Readmission diagnosis__________ Opened at bedside or I and D by surgeon_______________________________________ Return to surgery? Yes/No. Date ________________________________________________ Physicians’ diagnosis of SSI? Yes/No. If yes, by whom: Surgeon, Medical Attending Hospitalist, ED Physician, Others Notes: _______________________________________________________________________________________________________ Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5750 ORIGINAL ARTICLE _______________________________________________________________________________________________________________ The Strategies adopted to prevent SSI were based on the advisory, “surgical infection prevention collaborative”, in 2002 by center of medicare and Medicaid services. a. Delivery of intravenous antimicrobial prophylaxis with in 1 hour before incision ( 2hours are allowed for the administration of vancomycin and fluoroquinolones) b. Use of an antimicrobial prophylactic agent consistent with published guidelines c. Discontinuation of use of the prophylactic antimicrobial agent within 24 hours after surgery (discontinuation within 48 hours is allowable for cardio-thoracic procedures for adult patients) “The Surgical care improvement project”, a multi agency collaboration created in 2003, is an extension of the surgical infection prevention collaborative16 has further recommended Proper hair removal: No hair removal, or if required hair removal with clippers is considered appropriate. Controlling blood glucose level during the immediate postoperative period for patients undergoing surgery: Controlled 6:am blood glucose level (lower than 200mg/dl) on post operative day 2, with procedure day being post operative day 0 Maintenance of peri-operative normothermia for patients undergoing surgery17 SSI data for ortho clean case with implants (DHS)-2011 Total no of with implants cases2011 70 Total on of SSI 1 RATES PER 100 CASE A 1.4% RESULTS and DISCUSSION: Of the 70 surgeries, 1-(1.4%) Superficial incisional SSI was noticed and it settled down with debridement and antibiotics. Patient stayed with us for 11 days. There was no deep or organ space infection noted. Infective organism was Klebsiella pneumoniae18. (Lee et al. in the study showed that kleb. Pneumonia incidence was 1.6 in all orthopedic infections) The NHSN data between 2006 and 2008 showed 0.67-2.4 per 100 operations in patients undergoing hip prosthesis.19 According to the NHSN report, a large U.S. database for HAI aggregation and comparison report titled: “Data Summary for 2006 through 2008,” issued in December 2009, in Open reduction of fracture, for Risk index category 0 the pooled mean is 1.11, for 1 it is 1.78 and for 2, 3 it is 3.3619. C Edwards et aloin 2008 showed an overall SSI rate of 2.3 % in a study of surgically treated intertrochanteric cases20. Duckworth AD et al. in 2012 had an infection rate of 1.6% in a study of surgically treated proximal femoral fractures21. Ranjeetesh kumar, R N Singh et all in a study in 2012 had a SSI rate of 4% for all intertrochanteric fractures22. SSI rates are a constant reminder of any hospital’s wellbeing. It directly reflects on the quality of Administrative policies, operation theatre conditions, pre and post operative care, and the Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5751 ORIGINAL ARTICLE hygiene. The quality of nursing care is also reflected. More so in clean and elective cases, where infection is a complication of the procedure undertaken. It is important to note that to a larger extent it is a preventable complication. With proper protocols and guideline based on international recommendations, SSI can be brought to near 0%. But the guide lines need to be tailored to the institute based on the procedures undertaken and also conditions of the operation theatre. Our hospital has evolved a system and it was put to test by meticulous follow up of surgical cases and documentation of the events. The broad guidelines are: i. Appropriate preoperative management, which include assessment and optimization of various risk factors (Table 1) ii. Initiation of antibiotic prophylaxis to cover the common pathogens causing SSIs according to the procedure and hospital microbial flora. (Cefuroxime axetil was the preferred antibiotic.) iii. Control of operating theatre environment and avoidance of hypothermia. iv. Appropriate intra-operative management of the tissues and incision. v. Appropriate postoperative management which include optimization of blood glucose, supple-mental oxygenation, judicious use of blood transfusion & nutritional support. DHS was identified as the most common orthopaedic surgery conducted at our hospital. It was selected as the index surgery to evaluate and validate our infection control policy in clean surgeries with metal implantation. Based on our findings we can with confidence say that we can reduce the incidence of SSIs to near 0% with a good protocol of infection control policy. Implementation of the policies put up needs to be strictly monitored and corrective measures are to be undertaken time to time based on systematic analysis of the data. The process is ongoing and needs to be reviewed frequently. CONCLUSION: SSI has been a bugbear of all surgeons from the time surgery as a skill was developed. Infections were fought at different levels with different tools. With advent of carbolisation initially and antibiotics later it was thought that infection as a complication following surgeries was overcome. “THE BUGS ARE AHEAD OF HUMANS”. The micro-organisms seem to have all the ammunition to overcome the attack by antibiotics. Innumerable antibiotics from different families and chemical structure acting on different layers and parts of the micro-organisms have been used and abused over the decades with some success and disasters. In spite of all efforts SSIs continue to be a major cause of concern in surgical health care. Prevention of SSIs is based on structured protocols, which are evolved by the hospital infection control committee. It is structured to the hospital depending on the antimicrobial flora of the hospital and also type of procedures undertaken at the hospital. A more holistic approach with a dedicated team to monitor the infection control protocols and the infection rates along with antibiotic policy is order of the day. We have evolved a policy at our hospital with a HICC comprising of Medical Microbiologist, clinician, nursing staff and the administration. It is binding all and also compels active participation of all concerned. Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5752 ORIGINAL ARTICLE REFERENCES: 1. Whitehouse JD, Friedman ND, Kirkland KB et al. The impact of surgical-site infections following orthopedic surgery at a community hospital and university hospital: adverse quality of life, excess length of stay and extra cost. Infect Control Hosp Epidemiol. 2002; 23:183-9. 2. Boyd RJ, Burke JF, Colton T. A Double-blind clinical trial of prophylactic antibiotics in hip fractures. J Bone Joint Surg. 1973; 55:1251-8. 3. Mangram AJ, Horan TC, Pearson ML et al. Guideline for prevention of surgical site infection. Infect Control Hosp Epidemiol. 1999; 20:250-78. 4. Brown EM, Path FR, Pople IK et al. Prevention of postoperative infection in patients undergoing spinal surgery. Spine. 2004; 29:938-45. 5. Boxma H, Broekhuizen T, Patka P et al. Randomised controlled trial of single-dose antibiotic prophylaxis in surgical treatment of closed fractures: the Dutch Trauma Trial. Lancet. 1996; 347:1133-7. 6. Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord.2000; 13:422-6. 7. Trampuz A, Zimmerli W. Antimicrobial agents in orthopedic surgery: prophylaxis and treatment. Drugs. 2006; 66:1089-105. 8. Yamaguchi K, Adams RA, Morrey BF. Infection after total elbow arthroplasty. J Bone Joint Surg Am. 1998; 80:481-91. 9. Bohsali KI, Wirth MA, Rockwood CA Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006; 88:2279-92. 10. Fry DE. The economic costs of surgical site infections. Surg Infec (Larchmt). 2002; 3 (suppl 1): S37-43. 11. Meehan J, Jamali AA, Nguyen H. Prophylactic antibiotics in hip and knee arthroplasty. J Bone Joint Surg Am. 2009; 91:2480-90. 12. Costerton J W, Stewart P S, Greenberg E P. Bacterial biofilms: a common cause of persistent infections. Science. 1999; 284:1318-22. 13. Costerton JW. Biofilm theory can guide the treatment of device-related orthopaedic infections. Clin Orthop Related Res. 2005; 437:7-11. 14. Lewis K. Riddle of biofilm resistance. Antimicrob Agents Chemother. 2001; 45:999-1007. 15. Matthews P C, Berendt A R, McNally MA et al. Diagnosis and management of prosthetic joint infection. BMJ.2009; 338:1378-83. 16. Bratzler D W, Hunt D R. The surgical site infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 2006; 43:322-330. 17. Institute of Health care improvement. Available at: http://www.ihi.org/. Accessed May 1, 2007. 18. Lee J, Singletary R, Schmader K, Anderson DJ, Bolognesi M, Kaye KS. Surgical site infection in the elderly, following orthopaedic surgery. Risk Factors and Outcomes. J Bone Joint Surg 2006; 88(8):1705–1712. 19. Edwards JR, Peterson KD, Mu Y et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008. Am J Infect Control. 2009; 37:783-805. Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5753 ORIGINAL ARTICLE 20. C. Edwards, A. Counsell, C. Boulton, C. G. Moran, MD, FRCS(Ed), Department of Orthopaedics and Trauma, University Hospital, Nottingham, Nottingham NG7 2UH, UK. Manchester Royal Infirmary, Oxford Road, Manchester M13 9WL, UK. 21. Duckworth AD, Phillips SA, Stone O, Moran M, Breusch SJ, Deep infection after hip fracture surgery: predictors of early mortality. Injury. 2012 Jul; 43(7):1182-6. doi: 10.1016/j.injury.2012.03.029. Epub 2012 Apr 27. 22. Ranjeeteshkumar, RN Singh, BN Singh, comparative prospective study of proximal femoral nail and dynamic hip screw in treatment of intertrochanteric fractures Journal of clinical orthopedics and trauma, 2012 Jun, Vol 3 issue1: 28-36. AUTHORS: 1. Archana G. 2. Hanume Gowda S.N. PARTICULARS OF CONTRIBUTORS: 1. Associate Professor, Department of Microbiology, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore. 2. Associate Professor, Department of Orthopaedic Surgery, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore. NAME ADRRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hanume Gowda, S.N. AHA Ortho Care, 221, Nagarbhavi Main Road, 12th Block, Nagarbhavi, Bangalore -560072. Email – ahaortho@gmail.com Date of Submission: 24/07/2013. Date of Peer Review: 25/07/2013. Date of Acceptance: 29/07/2013. Date of Publishing: 31/07/2013 Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 31/ August 5, 2013 Page 5754