Physiologic differences between infants, children and adults
advertisement
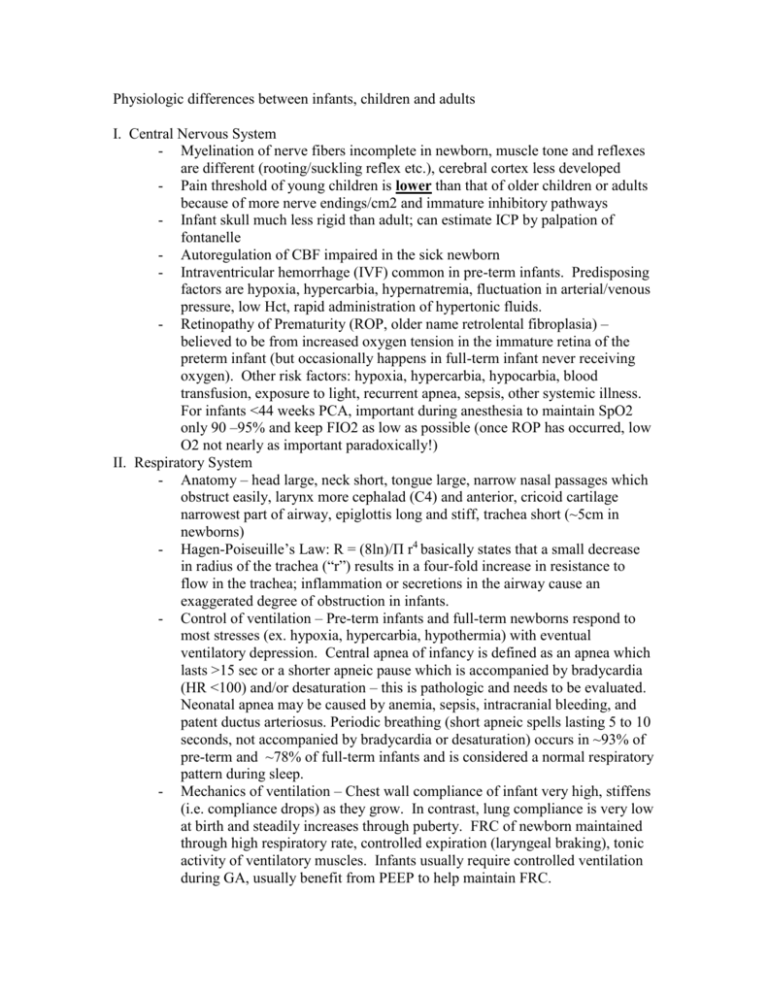
Physiologic differences between infants, children and adults I. Central Nervous System - Myelination of nerve fibers incomplete in newborn, muscle tone and reflexes are different (rooting/suckling reflex etc.), cerebral cortex less developed - Pain threshold of young children is lower than that of older children or adults because of more nerve endings/cm2 and immature inhibitory pathways - Infant skull much less rigid than adult; can estimate ICP by palpation of fontanelle - Autoregulation of CBF impaired in the sick newborn - Intraventricular hemorrhage (IVF) common in pre-term infants. Predisposing factors are hypoxia, hypercarbia, hypernatremia, fluctuation in arterial/venous pressure, low Hct, rapid administration of hypertonic fluids. - Retinopathy of Prematurity (ROP, older name retrolental fibroplasia) – believed to be from increased oxygen tension in the immature retina of the preterm infant (but occasionally happens in full-term infant never receiving oxygen). Other risk factors: hypoxia, hypercarbia, hypocarbia, blood transfusion, exposure to light, recurrent apnea, sepsis, other systemic illness. For infants <44 weeks PCA, important during anesthesia to maintain SpO2 only 90 –95% and keep FIO2 as low as possible (once ROP has occurred, low O2 not nearly as important paradoxically!) II. Respiratory System - Anatomy – head large, neck short, tongue large, narrow nasal passages which obstruct easily, larynx more cephalad (C4) and anterior, cricoid cartilage narrowest part of airway, epiglottis long and stiff, trachea short (~5cm in newborns) - Hagen-Poiseuille’s Law: R = (8ln)/П r4 basically states that a small decrease in radius of the trachea (“r”) results in a four-fold increase in resistance to flow in the trachea; inflammation or secretions in the airway cause an exaggerated degree of obstruction in infants. - Control of ventilation – Pre-term infants and full-term newborns respond to most stresses (ex. hypoxia, hypercarbia, hypothermia) with eventual ventilatory depression. Central apnea of infancy is defined as an apnea which lasts >15 sec or a shorter apneic pause which is accompanied by bradycardia (HR <100) and/or desaturation – this is pathologic and needs to be evaluated. Neonatal apnea may be caused by anemia, sepsis, intracranial bleeding, and patent ductus arteriosus. Periodic breathing (short apneic spells lasting 5 to 10 seconds, not accompanied by bradycardia or desaturation) occurs in ~93% of pre-term and ~78% of full-term infants and is considered a normal respiratory pattern during sleep. - Mechanics of ventilation – Chest wall compliance of infant very high, stiffens (i.e. compliance drops) as they grow. In contrast, lung compliance is very low at birth and steadily increases through puberty. FRC of newborn maintained through high respiratory rate, controlled expiration (laryngeal braking), tonic activity of ventilatory muscles. Infants usually require controlled ventilation during GA, usually benefit from PEEP to help maintain FRC. Lung volumes – Total lung capacity (90 ml/kg), dead space volume (2 ml/kg), tidal volume (7-9 ml/kg) all similar to adult values on a per kg basis. Oxygen consumption much higher in infants; 6-8 ml/kg/min compared to 3-4 ml/kg/min in adults. Closing volume much higher in infants – may explain lower normal values for PaO2 during infancy. - Growth and development – alveoli start to develop at ~32 weeks GA (terminal bronchioles participate in gas exchange previous to this), number of alveoli increase rapidly over first 18 months of life (near adult levels) but morphologic and physiologic development continue through 1st decade - Volatile gas induction – infants more likely to develop laryngospasm (thus we avoid deep extubation in most infants < 1yr of age), also have depression of pharyngeal dilator muscles more quickly resulting in partial/complete airway obstruction while diaphragm continues to attempt breathing. - Uptake/distribution of volatile anesthetics 3x faster in infants than adults because of: 1. Increased alveolar-ventilation to FRC ratio 2. Decreased blood/gas partition coefficient. 3. Decreased tissue/blood partition coefficient 4. Increased C.O. (which should delay equilibration in adults, but in children this is overcome by the vessel-rich-group being a much larger percent of body weight in infants than in adults). - MAC for Isoflurane and Desflurane steadily increases from 24 weeks gestation and reaches a peak during infancy then steadily starts to decline. For Sevoflurane, MAC is relatively constant for neonates and infants (3.2%), and then decreases to 2.5% in children aged 6 mo. – 12 years. III. Cardiovascular System - Fetal circulation – “oxygenated” blood (PaO2 35!) returns from the placenta, most bypasses the liver via the ductus venosus. From the IVC, flows through the right atrium and majority streams across foramen ovale into left atrium. From left ventricle goes out aorta to head and neck vessels. Deoxygenated blood returning from head via SVC enters RA, majority into right ventricle and out pulmonary artery. Because of high PVR, 80% of this blood flows across ductus arteriosus (other 20% goes to lungs) and to remainder of body. - Changes at birth – PVR drops dramatically with first few breaths, flow reversed in ductus arteriosus as SVR increases when placenta is removed from circulation (prostaglandin supply shut off). Increased blood return via lungs to LA causes increased left sided pressure (increased SVR also contributes) which functionally closes foramen ovale (still patent in 25% of adults). Ductus arteriosus usually closes within first 24 hours due to increased oxygen saturation and removal of prostaglandins from circulation. - Transitional circulation – PDA doesn’t close, shunting across it may be L>R, R>L or bidirectional – newborn may revert to this under stress such as sepsis, hypoxia, hypercarbia, acidosis, congenital heart disease. By having a preductal and post-ductal pulse-oximeter, you can detect if PDA is open and shunting R>L (i.e. lower extremities have lower O2 sat than upper extremities). When PDA shunt is exclusively R>L, this is called “persistent fetal circulation”. - Neonatal myocardium – fewer contractile elements, limited ability to change stroke volume so CO is rate-dependent, ventricle is less compliant, much better ability to tolerate hypoxia - Blood– volume is 80ml/kg in the term infant (20% higher in preterm infant). 70-90% of Hb present at birth is of the fetal type which has a leftward shift on the oxyhemoglobin dissociation curve. (This enables it to “hold on” to oxygen better while circulating through the placenta.) During first few months of life, Hct drops (due to suppression of erythropoiesis and increased plasma volume) to nadir at 2-3 months of age (Hct ~30, even lower in premature infants). IV. Hepatic function - Term neonate has stores of glycogen in the liver and myocardium, premature infant has smaller stores and is unable to establish adequate gluconeogenesis. Hypoglycemia is common in the stressed neonate (level <40mg/100ml). Be careful with infants of diabetic mothers and those with Beckwith-Wideman syndrome. Hyperglycemia may also be a problem in patients on glucose therapy. Because of low stores of glycogen, ALL neonates should be receiving a glucose-containing solution while in the OR at maintenance rate (bolus with normal saline or LR however). - Unconjugated hyperbilirubinemia (physiologic jaundice) – common in first week of life, due to increased bilirubin load as well as decreased hepatic cell uptake of bilirubin and deficient hepatic conjugation. Preterm infants are more susceptible to kernicterus (neurologic damage) due to less effective blood-brain barrier. - Hypoxia, acidosis, hypothermia, hypoalbuminemia (i.e. all common occurrences in the OR!) all increase the danger of kernicterus - Plasma levels of albumin are lower at birth therefore there is less protein binding of administered drug and more active drug available; however, a larger volume of distribution offsets this and most drugs (on a mg/kg basis) do not need to be adjusted for age. - At birth most enzyme systems are present but not induced therefore metabolism is slower – important to keep in mind when giving repeated doses of a drug or running an infusion. - Newborn has lower levels of coagulation proteins at birth – vit K is given shortly after birth to stimulate production of these factors. - Relative hepatic “maturity” reached by ~ 6 months. - V. Renal Function - GFR is low at birth but rises rapidly over the first few weeks of life and reaches adult levels by 2 years of age.Reductions in GFR are seen with hypoxia, hypothermia or CHF. - Newborn infants are unable to handle excessive fluid or solute loads (which is why they typically are started on D10W at a lower rate for the first few days of life) - The capacity to excrete H+ increases with age - VI. VII. There is a lower renal threshold for HCO3 in infants (therefore their bicarbonate level may be lower than usual) Temperature Homeostasis - Infants have a large surface area:volume ratio which makes radiant heat loss (the major cause of heat loss in the OR) proportionally greater in the small infant. - Convective heat gain (from an under-body bair-hugger which is turned on before the patient enters the room) is probably the major force in maintaining normothermia in infants and children. - Infants are unable to shiver to raise their temperature, instead they are dependent on brown adipose tissue metabolism which is stimulated by norepinephrine release - Brown “fat” is found around the scapulae, in the mediastinum, and surrounding the kidneys and adrenal glands Gastorintestinal Function - At birth, gastric pH is alkalotic, but by the next day it has reached typical levels of acidosis. - Coordination of swallowing with respiration occurs at 4-5 months. Therefore the incidence of gastroesophageal reflux is relatively high.