Risk Stratification of Upper Gastrointestinal Bleeding Singleton
advertisement
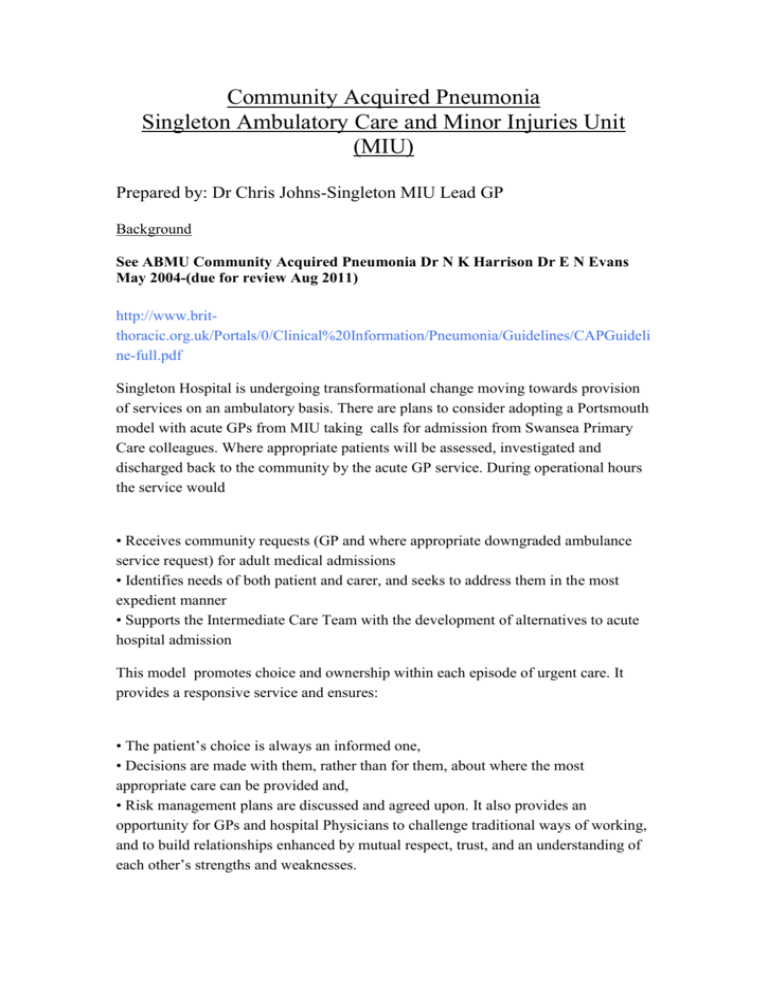
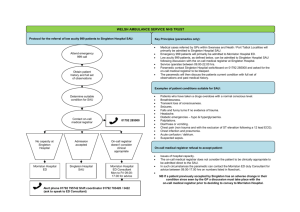
Community Acquired Pneumonia Singleton Ambulatory Care and Minor Injuries Unit (MIU) Prepared by: Dr Chris Johns-Singleton MIU Lead GP Background See ABMU Community Acquired Pneumonia Dr N K Harrison Dr E N Evans May 2004-(due for review Aug 2011) http://www.britthoracic.org.uk/Portals/0/Clinical%20Information/Pneumonia/Guidelines/CAPGuideli ne-full.pdf Singleton Hospital is undergoing transformational change moving towards provision of services on an ambulatory basis. There are plans to consider adopting a Portsmouth model with acute GPs from MIU taking calls for admission from Swansea Primary Care colleagues. Where appropriate patients will be assessed, investigated and discharged back to the community by the acute GP service. During operational hours the service would • Receives community requests (GP and where appropriate downgraded ambulance service request) for adult medical admissions • Identifies needs of both patient and carer, and seeks to address them in the most expedient manner • Supports the Intermediate Care Team with the development of alternatives to acute hospital admission This model promotes choice and ownership within each episode of urgent care. It provides a responsive service and ensures: • The patient’s choice is always an informed one, • Decisions are made with them, rather than for them, about where the most appropriate care can be provided and, • Risk management plans are discussed and agreed upon. It also provides an opportunity for GPs and hospital Physicians to challenge traditional ways of working, and to build relationships enhanced by mutual respect, trust, and an understanding of each other’s strengths and weaknesses. One of the areas of care the Portsmouth model has focused on is risk stratification and treatment of Community Acquire Pneumonia Singleton Minor Injuries GP could assess and treat and discharge low risk patients and arrange appropriate review with colleague GPs or OPD review. Moderate and high risk patients would be treated and seen in the usual way but there would be benefits of initial investigations having been completed. Many GPs will refer patients to SAU in this clinical category with SOB ? cause or ? PUO or have clinical suspicions on auscultation. Urgent on the day CXR with reporting and Pathology is often not available for GPs. Simple assessment and straight forward investigation would allow many patients to be assessed, treated and discharged by an acute GP unit. MIU assessment History, Examination following GP letter of referral Initial investigations 1. CXR 2. FBC 3. U and E, LFT and glucose 4. CRP 5. Further investigations dependant on history and clinical suspicions If CXR shows Pneumonic change then progress to. Radiology or General Medical support to review X ray at Singleton if available CURB65 and CRB65 Clinical Severity Scoring Clinical factor Points Confusion 1 Blood urea nitrogen > 7mmol/l 1 Respiratory rate > 30 breaths per minute 1 Systolic blood pressure < 90 mm Hg or Diastolic blood pressure < 60 mm Hg Age > 65 years 1 Total points: 1 CURB-65 score Mortality (%) Recommendation 0 0.6 1 2.7 2 6.8 Short inpatient hospitalisation or closely supervised outpatient treatment 3 14.0 4 or 5 27.8 Severe pneumonia; hospitalise and consider admitting to intensive care CRB-65 score Mortality (%) 0 0.9 Very low risk of death; usually does not require hospitalisation 1 5.2 Increased risk of death; consider hospitalisation 2 12.0 3 or 4 31.2 Low risk; consider home treatment Recommendation High risk of death; urgent hospitalisation CURB-65 = Confusion, Urea nitrogen, Respiratory rate, Blood pressure, 65 years of age and older. CRB-65 = Confusion, Respiratory rate, Blood pressure, 65 years of age and older. Additional adverse prognostic features include: Coexisting disease Hypoxaemia (SpO2 <92%, PaO2 <8kPa) Bilateral/multilobe involvement COMMUNITY AQUIRED PNEUMONIA FLOWCHART Triage/Initial Assessment suggestive of CAP Result of CXR reviewed by clinician No consolidation Consolidation Reassess Does the patient meet Criteria for CAP? Yes No Treat according to clinical judgement and CURB65 severity score 0-1 Low severity (risk of death <3%) 2 Moderate severity (risk of death 9%) 3-5 High severity (risk of death 15-40%) Consider other diagnoses and treat as appropriate Other reasons for admission (unstable comorbidity, social No Hospital SAU Hospital SAU CURB65 Severity Score 1 point for each feature present Yes Home Antibiotics Review in MIU 24 hours later Hospital SAU Aim by 4 hours: diagnosis made and management including antibiotics started Confusion Urea > 7 mmol/l Respiratory rate ≥ 30/min Blood pressure (SBP <90 or DBP ≤ 60mmHg) Age ≥ 65 years Low Severity CAP Antibiotic Therapy (ABMU Formulary) Communityacquired pneumonia treatment in the community2,3 BTS 2009 Guideline Use CRB65 score to help guide and review:1 Each scores 1: Confusion (AMT<8); Respiratory rate >30/min; BP systolic <90 or diastolic ≤ 60; Age ≥65 years Score 0: suitable for home treatment; Score 1-2: hospital assessment or admission Score 3-4: urgent hospital admission Give immediate IM benzylpenicillin or amoxicillin 1G po D if delayed admission/life threatening Mycoplasma infection is rare in over 65s 1 IF CRB65=0: amoxicillinA+ or clarithromycin Aor doxycycline D If CRB65=1 & AT HOME amoxicillin A+ AND clarithromycin Aor doxycycline alone 500 mg TDS 500 mg BD 200 mg stat/100 mg OD 7 days 7 days 7 days 500 mg TDS 500 mg BD 200 mg stat/100 mg OD 7-10 days 7-10 days