RESPI RA TORY PHYSIOLOGY
advertisement

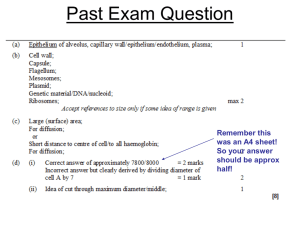
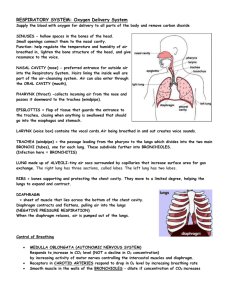
PHYSIOLOGY LECTURE OUTLINE: RESPIRATORY PHYSIOLOGY The Primary Functions of the Respiratory System 1. Ventilation (Inspiration - Expiration) to exchange air with the body and environment. 2. To exchange gases, oxygen and carbon dioxide, between lungs and blood. 3. To homeostatically maintain pH of body fluids. 4. For vocalization and sound production. Respiratory System The Respiratory System includes structures involved in ventilation and gas exchange. The respiratory system divided into upper and lower tracts as well as conduction and respiratory portions. Below is a basic outline of the anatomical structures: Upper tract Nose, nasal cavity, mouth, pharynx (throat) and larynx (voice box). Lower tract Trachea (wind pipe), left and right primary bronchi, secondary and tertiary bronchi, bronchioles, terminal and respiratory bronchioles, alveolar duct, alveolar sac and alveoli - the end where gas is exchanged). The conducting portion consists of the airways from environment that lead to the exchange surface of lungs (from nose to terminal bronchioles). The respiratory portion is from the respiratory bronchioles to the alveoli (the surface area for gas exchange). The diameter of airways get progressively smaller, but total cross-sectional surface area increases. Velocity of air flow is therefore highest in trachea, lowest in terminal bronchioles. Air moves down its pressure gradient caused by the changes in volume of the thoracic cavity. The lungs are located in the thoracic cavity and as the volume of the thoracic cavity increases, the pressure inside this cavity (and thus in the lungs) decreases. As the volume of the thoracic cavity decreases, the pressure increases. Thus, movement of thorax creates alternating conditions of high and low pressure within lungs. This creates air exchange in response to pressure gradients. The relationship between the pressure and volume of a gas is described by Boyle's Law (P 1 V1 = P2 V2). As volume decreases, pressure increases and vice versa. Changes in volume of chest cavity during ventilation cause pressure gradients. Increase chest volume - decrease pressure - air moves in from atmosphere. Decrease chest volume - increase pressure - air moves out from body. The Bones and Muscles of the Thorax Surround the Lungs The thoracic cage is created by the bones and muscles bounding the thorax: The ribs and spine; chest wall; and the diaphragm, a dome-shaped skeletal muscle forming thoracic floor. The internal and external intercostal muscles connect the 12 rib pairs. The sternocleidomastoids and scalenes connect the head and neck to the first 2 ribs. Because the muscles of the thorax are skeletal muscles, they are innervated by somatic motor neurons. Control of those neurons originates in a network of respiratory neurons in the medulla oblongata. The thorax is functionally a sealed cavity with 3 membranous bags. The pericardial sac contains the heart and there are 2 pleural, each sac containing one lung. 2 Pleural Sacs Enclose the Lungs Lungs are light, spongy tissue mostly occupied by air-filled spaces.. The narrow apex of each lung is at the top of the thoracic cavity, under the upper ribs and clavicle. The bronchi connect lungs to trachea to the atmosphere. Each lung is divided into lobes: the right lung into three lobes, and the left lung into two (tri before you bi). Because of the space occupied by the heart, the left lung is smaller than the right. Each lung is contained in double-walled pleural sac. It is like an air-filled balloon surrounded by a water-filled balloon. The pleura contains elastic connective tissue and capillaries. The pleural fluid holds opposing pleural layers together, creating a slippery surface allowing movement of membranes as lungs move. It holds lungs tight and stretched against thoracic wall due to fluid's cohesiveness. The Alveoli are the Site of Gas Exchange An alveolus has a single layer of thin exchange epithelium and is the site of gas exchange. There are 3 types of cells in alveoli: 1. Type I alveolar cells: Very thin, allowing gas exchange. 2. Type II alveolar cells: Thicker, secrete surfactant to ease lung expansion. 3. Alveolar macrophages: Protect and defend Alveoli do not contain muscle fibers and cannot contract. There are elastin fibers between alveoli and these do contribute to elastic recoil when lung tissue is stretched. Capillaries cover 80-90% of alveolar surface forming an almost continuous blood-air contact. Gas exchange occurs by simple diffusion. The single endothelial cell of the capillary and the single squamous epithelium of the alveoli have a fused basement membrane in between them, this arrangement allows for a rapid diffusion of gases. The Pulmonary Circulation is a High-Flow, Low-Pressure System At rest, the pulmonary circulation of the cardiovascular system contains about 0.5 L of blood (10% of total blood volume) with 75 ml in capillaries for gas exchange. The conducting portions of the respiratory tract that are not involved in gas exchange receive oxygenated arterial blood from the systemic circulation. But the deoxygenated venous blood leaving these regions does not return to the systemic circulation and the vena cava. Instead, it flows into the pulmonary veins along with freshly oxygenated blood from the alveoli. The addition of deoxygenated blood slightly lowers the oxygen content of the blood before it ever reaches the left side of the heart. The rate of blood flow through the lungs is greater than that of other tissues. The lungs receive the entire volume of right ventricle cardiac output (5 L/min). The pulmonary circulation has low pressure in, with an average pressure = 25/8 mm Hg compared to 120/80 mm Hg systemic blood pressure. This is correlated with low pulmonary resistance. The pulmonary arteries are much more compliant (distensibile, easier to stretch) than the aorta and systemic arteries. Also, the total length of pulmonary blood vessels is shorter. As we already know, this means that the right ventricle doesn't have to pump as hard to overcome peripheral resistance. This allows for low pulmonary blood pressure. In turn, there is low net hydrostatic pressure, yielding low fluid flow into interstitial space. Lymphatic system removes filtered fluid, a small volume of interstitial fluid, less than 0.5 L/day of fluid is lost from the pulmonary capillaries, compared to the loss of 3 L/day from the systemic capillaries. 3 GAS LAWS Air flow is similar to blood flow in that the driving force for air flow is a pressure gradient and it is opposed by resistance. Air Flow = P/R Air is a Mixture of Gases The atmosphere is mixture of gases and water vapor. In many parts of the world, pollutant gases such as ozone, sulfur dioxide, and carbon monoxide are also present in varying trace amounts. Dalton's Law The total pressure of a gaseous mixture is the sum of individual gas (partial) pressures. Individual gases move down partial pressure gradients. The sum of all partial pressures gives the total pressure for a mixture of gases (Dalton's Law). This is how individual gas exchange occurs: gases move from areas of higher partial pressures to areas of lower partial pressures. Partial pressures = Patm x % of gas in atmosphere. Partial pressures vary with amount of water vapor. e.g., air is a mixture of gases. N2 = 79% O2 = 21% CO2 = 0.03% If atmospheric pressure of air at sea level is 760 mmHg (a standard value, see section below) and air is a mixture of the above gases (N2, O2 and CO2), then we can calculate the partial pressure exerted by each gas in this mixture. The partial pressure of N2 is symbolized by PN2 and partial pressure of O2 is PO2, etc. Calculating Partial Pressures of gases in air at sea level: 1) PN2 = 760 mm Hg x % of gas in mixture (79%, = 0.79) = 760 mm Hg x 0.79 = 600 mm Hg 2) PO2 = 760 mm Hg x % of gas in mixture (21%, = 0.21) = 760 mm Hg x 0.21 = 160 mm Hg 3) PCO2 = 760 mm Hg x % of gas in mixture (0.03%, = 0.003) = 760 mm Hg x 0.003 = 0.24 mm Hg (which is negligible) 4 Boyle's Law Describes Pressure-Volume Relationship of Gases Gas pressure in a sealed container is created by the collision of gas molecules with the walls of the container and each other. The smaller the container, the more frequent the collisions, resulting in higher pressures. Boyle's Law states: P1 V1 = P2 V2. As volume decreases, pressure increases and vice versa. Changes in volume of chest cavity during ventilation cause pressure gradients, which create air flow. An increase in chest volume causes a decrease in pressure - air moves in from atmosphere. A decrease inchest volume causes an increase in pressure - air moves out from body. The Solubility of a Gas in Liquid Depends on Pressure, Solubility and Temperature Where air and water meet, a particular gas flows from the medium with higher partial pressure to medium with lower partial pressure. Movement of a gas into a liquid is directly proportional to 3 factors: 1. The Partial Pressure gradient of that gas. The greater the partial pressure gradient, the more soluble the gas in liquid. 2. Temperature of liquid and surroundings. The warmer the liquid, the less soluble the gas in it! Think of the soda can example. 3. Solubility of the gas in that liquid. Gases have different solubilities in liquids depending on their molecular chemistry. Solubility: The more soluble a gas is, the less partial pressure needed to force it into solution. Poorer solubility requires higher partial pressures to move even small amounts of gas. Oxygen is about 20 times less soluble in water than carbon dioxide is. This is why there is such a large partial pressure gradient for O2 (60 mm Hg) compared to the more soluble CO2 (6 mm Hg). Gases move between phases until equilibrium is reached. Partial pressure for a gas in the air phase at equilibrium = Partial pressure of that gas in liquid phase. This does not mean that concentrations are equal! Concentrations depend on solubility. Thus O2 needs oxygen-carrying compounds in blood, such as hemoglobin (Hb). VENTILATION Ventilation = Movement of air between environment and lungs, the first exchange. The Airways Warm, Humidify, and Filter Inspired Air The upper airways condition inspired air before it reaches alveoli in three main ways: 1. Warm air to body temperature (37 °C) to avoid alveolar damage. 2. Humidify to 100% to keep exchange epithelium moist. 3. Filter out foreign material, to protect delicate lung tissue. Most of this conditioning is done in the nasal cavity, that is why breathing through your nose has a different effect than breathing through your mouth. Heat and water from the mucosal lining of airways warms and humidifies the inspired air. Filtration occurs in the nasal cavity, trachea and bronchi. These areas are lined with ciliated epithelium that secrete mucus and dilute saline, which traps inhaled particles larger than 2 mm and has immunoglobulins to disable microorganisms. The cilia of the epithelial lining is referred to as the mucus escalator. The mucus is continuously moved toward pharynx, then swallowed or spat out! The stomach acids will further destroy microorganisms. Secretion of the watery saline layer beneath the mucus is a critical step in mucus escalator. Cilia would be 5 - trapped in mucus without it. Cystic fibrosis is a genetic disorder wherein there are defective Cl channels which inhibit saline production, so the mucus is thick and hampers cilia movement. During Ventilation, Air Flows Because of Pressure Gradients The lungs are held to the thoracic cage by pleural fluid and contraction of thoracic muscles creates the pumping action and the pressure gradients. Air moves in response to pressure gradients. The primary muscles involved in quiet breathing (eupnea) are: the diaphragm, intercostals and scalenes. Forced breathing is termed hypereupnea (e.g., exercise, wind instrument, blowing up a balloon): Other chest and abdomen muscles assist. Air flow in respiratory system obeys the same rules as blood flow: Air flow = P/R. Flow increases as the pressure gradient increases and decreases as resistance (R) increases. Various Respiratory Pressures 1. Atmospheric pressure is the weight of the column of air above you. This remains relatively constant, At sea level, this value is 760 mmHg. The pressure in the lungs must be higher or lower than atmospheric pressure for air flow to be created. 2. Intra-alveolar pressure (PA): The pressure inside the alveoli, where gas is exchanged. 3. Intra-pleural pressure: The pressure within the pleural fluid, which is always less than intra-alveolar. Inspiration Occurs When Alveolar Pressure Decreases Inspiration: Somatic motor neurons trigger contraction of diaphragm, inspiratory muscles. Diaphragm contraction - compression of dome shape, drops toward abdomen, causing 60-75% change of thoracic cavity volume. External intercostal and scalene contraction to move rib cage upwards and out, causing 2540% change of thoracic cavity volume. As thoracic cavity volume increases, pressure decreases and air moves into lungs. Typically, very small changes in alveolar pressure are required for ventilation. When thoracic cavity volume increase, inter-alveolar pressure drops about 2 mm Hg below atmospheric (to about 758 mm Hg) and air begins to flow into alveoli. Air flow continues until pressure inside lungs equals atmospheric pressure (760 mm Hg). At the end of inspiration, the somatic motor neurons to the diaphragm and external intercostals stop firing, causing relaxation. This allows for passive expiration, due to elastic recoil of lungs, not muscle contraction. Expiration occurs when intra-alveolar pressure exceeds atmospheric pressure (reaches about 762 mm Hg). Active expiration happens during exercise or forced heavy breathing. This occurs during voluntary exhalations and when ventilation exceeds 30-40 breaths/min. Uses internal intercostals and abdominals muscles, expiratory muscles. Diseases afflicting skeletal muscle can adversely affect ventilation. Myasthenia gravis is a disease in which ACh receptors on motor end plates are destroyed. Also, polio is caused by a virus that can paralyze respiratory muscles. Intrapleural Pressure Changes during Ventilation The lungs are "stuck" to the thoracic cage by pleural fluid and this aids in lung expansion and contraction. Intrapleural pressure is sub-atmospheric and sub-intra-alveolar (usually ranging from 754 to 758 mm Hg). Puncturing the pleural cavity leads to pneumothorax - a loss of the pressure gradient that keeps lungs in their stretched state. The afflicted lung will collapse under elastic recoil. Air must be removed from the intra-pleural space and puncture sealed to correct pneumothorax. 6 Lung Compliance and Elastance May Change in Disease States Compliance is the ability of the lungs to stretch. High-compliance lungs are easily stretched. Lowcompliance lungs require more force to stretch lungs (more work, which means more energy) Pulmonary Elastance = Elasticity. High compliance doesn't necessarily mean high elastance. Pulmonary Elasticity vs. Compliance Elasticity (elastance, elastic recoil) means that something is able to return to its original shape after the force stretching it has been removed. Compliant simply means that a substance can be stretched. In physiology, the normal lung is both compliant and elastic. Pulmonary elasticity is generated by 2 things: 1) Elastic Fibers These fibers are an integral part of lung tissue and the natural tendency of these fibers to recoil facilitates passive expiration. 2) Surface Tension The alveolar surface has a thin layer of water on it. The water molecules create surface tension between the air-fluid boundaries in the alveoli. Surface tension arises due to the strong attractive force that water has for itself. If we remember from the beginning of semester, one of the key properties of water is cohesion (water is said to have a high affinity for itself). The polarity of the water molecule means that it can form hydrogen bonds with itself, creating a cohesive layer of water, generating tension on the surface of the alveoli. Surface tension tends to make the bag-shaped alveoli collapse, the smaller it is, the closer water can be to itself and that suits the chemical nature of water. This assist elastic recoil but also increases the work needed to stretch the air-filled lung. Surfactant Decreases the Work of Breathing Molecules that disrupt the cohesive forces between water molecules will reduce the surface tension generated by water and decrease the work load of breathing. Surfactant is a phospholipoprotein made and released by alveolar type II cells. Surfactant molecules positions themselves in between water molecules, thereby reducing surface tension, creating more compliant lungs. Law of La Place The law of La Place describes the force (pressure) that is created by a fluid sphere or bubble. The pressure (P) depends on surface tension (T) and radius (r). La Place's Law: P = 2 T/r Alveoli are analogous to spheres and behave much like balloons. If two alveoli have different diameters but are lined by fluids with the same surface tension, according to La Place's law, the pressure inside the smaller alveolus will be greater. This would force the smaller alveoli to collapse into the larger ones. If this were to happen, much of the convoluted surface area of the alveoli would be lost. Surfactants reduce surface tension and prevent all alveoli from collapsing, but is more concentrated in smaller alveoli, making surface tension is less than in the larger alveoli. This acts to equalize the pressures among the different sized alveoli. Newborn Respiratory Distress Syndrome (NRDS) typically occurs in premature babies, whose alveolar type II cells are not fully developed. Thus, they do not make adequate surfactant to prevent alveoli from collapsing, giving them low-compliance lungs and collapsing alveoli. Coupled with under developed 7 respiratory muscles, the newborn babies have a very difficult time breathing normally and must expend a great deal of energy to re-inflate the collapsed alveoli. The condition known as adult respiratory distress syndrome (ARDS) is not related to surfactant production. ARDS is caused by pulmonary edema that occurs when pulmonary capillaries become leaky to plasma proteins as a result of infection or autoimmune disease. Emphysema is a condition in which elastin fibers are destroyed. These lungs have high compliance and low elastance. They exhibit poor recoil during expiration. With the changes of emphysema, the lung becomes even more compliant but less elastic, resulting in a hyper-inflated lung and the "barrel-chest" associated with chronic emphysema. Restrictive lung diseases show reduced compliance. More work must be expended to stretch a stiff lung. Possible causes: Inelastic scar tissue, insufficient surfactant production Airway Diameter is the Primary Determinant of Airway Resistance Resistance to air flow also influences work of breathing Poiseuille's Law: Length (L), viscosity (), and radius (r) affect resistance (R) The radius of the airways becomes a primary determinant of resistance. The length and viscosity are virtually constant in respiratory system (as in the cardiovascular system). About 90% of airway resistance is due to trachea and bronchi, but the cartilage maintains a constant diameter. Control of Airway Resistance The diameter of bronchiole is adjustable (they do not have cartilage and do have smooth muscle). Bronchoconstriction increases resistance and decreases amount of fresh air to alveoli. These chnages are under nervous, hormonal, and paracrine control. If there is an increase in CO2, this leads to bronchodilation (increased air flow). If histamine is released from mast cells this causes bronchoconstriction (decreased air flow). Stimulation of the parasympathetic division of the ANS causes bronchoconstriction. Stimulation of the sympathetic division causes bronchodilation. Asthma is an allergic inflammatory condition characterized by significant bronchoconstriction. This significantly increases resistance to air flow, particularly inhibiting passive expiration. Although histamine release is a central trigger in the bronchoconstriction of asthma and anaphylactic shock, we now know that a variety of other chemical signals are also responsible. Leukotrienes are lipid-like bronchoconstrictors secreted by mast cells, macrophages, and eosinophils during the inflammatory response. Some of the newest drugs for treating asthma are the leukotriene receptor antagonists such as Pranlukast (Accolade). For instance, without medical treatment, the massive bronchoconstriction of an asthma attack or allergic reaction can be fatal. The quick administration of an epinephrine injection or a beta-agonist inhaler such as ephedrine or isoproterenol induces bronchodilation that relieves the problem. Question: During anaphylactic shock and severe allergic reactions, the release of histamine causes bronchoconstriction. Why doesn't the stress of the attack cause the release of epinephrine and bronchodilation? 8 Answer: It probably does, but not in amounts high enough to overcome the effects of the massive amounts of histamine being released. A typical subcutaneous injection for anaphylactic shock contains 0.3-0.5 mg of epinephrine, a pharmacological dose. Pulmonary Function Tests Measure Lung Volumes During Ventilation Spirometers are used to measure volume of moving air with each breath. Obstructive lung diseases involve diminished air flow during expiration due to narrowing of bronchioles. Lung Volumes Air moved during breathing is divided into four lung volumes: 1. Tidal volume (VT): Air volume moving in a single normal inspiration or expiration. 2. Inspiratory reserve volume (IRV): Additional volume inspired above tidal volume. 3. Expiratory reserve volume (ERV): Air exhaled beyond the end of normal expiration. 4. Residual volume (RV): Air in respiratory system after maximal exhalation (not measured directly). Residual volume is measured by having the subject breathe helium, then calculating the dilution of the helium upon re-breathing room air. Lung Capacities Lung capacities are the sums of 2 or more lung volumes (are calculated volumes). 1. IRV + ERV + VT = Vital capacity (VC). Maximum volume of air voluntarily moved through respiratory system 2. VC + RV = Total lung capacity (TLC) 3. VT + IRV = Inspiratory capacity 4. ERV + RV = Functional residual capacity Patients with restrictive lung disease such as fibrosis have a decreased inspiratory capacity. Emphysema patients who have lost elastic recoil cannot expel as much air during passive expiration and have an increased functional residual capacity. Auscultation of Breath Sounds Breath sounds have wide range of normal variation and are important to use as diagnostic tools, like heart sound auscultation. For example, air whistling through constricted airways produces the characteristic wheezing that accompanies an asthmatic attack. Rate and Depth of Breathing Determine the Efficiency of Breathing Total pulmonary ventilation = Volume of air moved into/out of lungs each minute. Ventilation rate x tidal volume = Total pulmonary ventilation 2. Measures effectiveness of ventilation. Normal adult rate = 12-20 breaths/min - Total pulmonary ventilation of 6 L/min. Anatomic dead space = Conducting airways not exchanging gas. 9 In some pathologies, there may also be alveolar dead space, that is, alveoli that are being ventilated but not being perfused. This might occur with low blood pressure, when the capillaries in the apex of the lung are collapsed. The combination of alveolar dead space and anatomic dead space is called physiologic dead space. Alveolar ventilation is more accurate indicator of ventilation efficiency. Alveolar ventilation = Ventilation rate x (tidal volume - dead space volume). At 12 breaths/min, alveolar ventilation rate under same conditions before = 4.2 L/min (vs. 6 L/min). Gas Composition in the Alveoli Varies Little During Normal Breathing PO2 and PCO2 vary during hypo- and hyperventilation. Hyperventilation: PO2 increases and PCO2 decreases. Hypoventilation: PO2 decreases and PCO2 increases. During normal breathing, partial pressures remain fairly constant. PO2 = 100 mm Hg. PCO2 = 40 mm Hg. Why? Oxygen entering alveoli approximately equals oxygen entering blood Fresh air entering lungs is only about 10% of total lung volume. Ventilation and perfusion are matched to ensure efficient exchange and delivery of gases. Oxygen transport in the blood is largely due to hemoglobin (Hb). Hemoglobin (Hb)-oxygen binding affinity is affected by: pH, CO2, temperature, and 2,3-DPG. These changes are reflected in the oxygen-Hb dissociation curve. Most CO2 is converted into H+ and HCO3- by carbonic anhydrase inside RBCs. The reaction is: CO2 + H2O H+ + HCO3. Therefore, body pH is related to PCO2 and ventilation. Respiration is under the control of a central pattern generator in the medulla oblongata and the pons. Chemical factors such as PO2, PCO2, and H+ of body fluids affect ventilation via central and peripheral chemoreceptors. We can also exert conscious control over breathing, but not past the point of chemoreceptor response.