Meniere`s Disease
advertisement
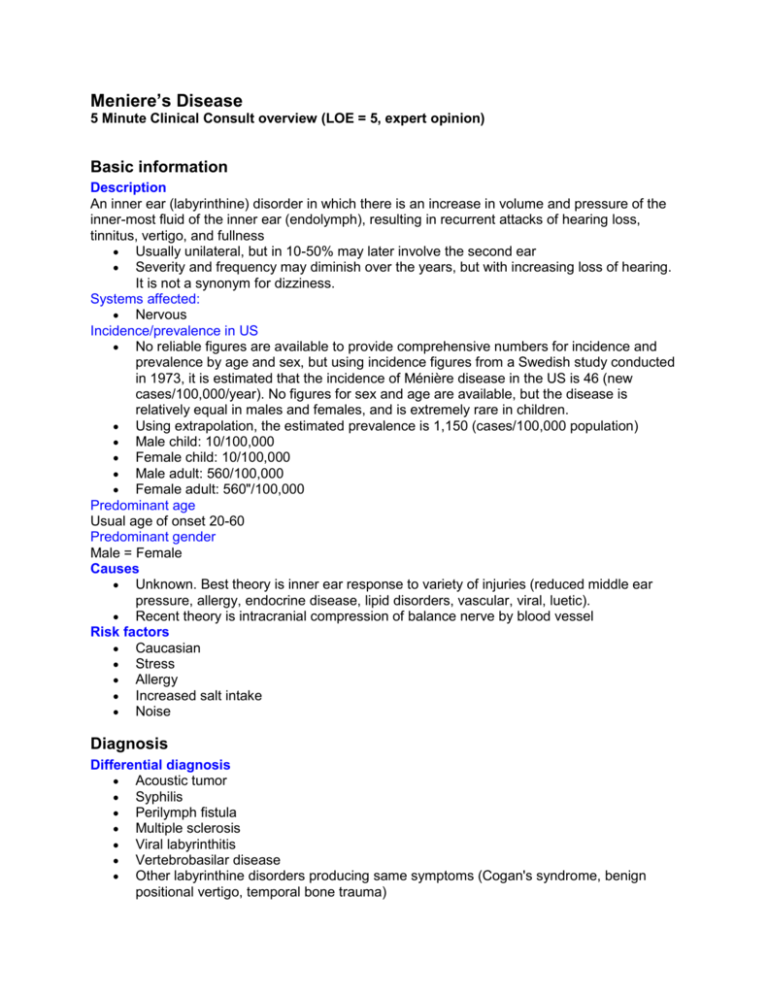
Meniere’s Disease 5 Minute Clinical Consult overview (LOE = 5, expert opinion) Basic information Description An inner ear (labyrinthine) disorder in which there is an increase in volume and pressure of the inner-most fluid of the inner ear (endolymph), resulting in recurrent attacks of hearing loss, tinnitus, vertigo, and fullness Usually unilateral, but in 10-50% may later involve the second ear Severity and frequency may diminish over the years, but with increasing loss of hearing. It is not a synonym for dizziness. Systems affected: Nervous Incidence/prevalence in US No reliable figures are available to provide comprehensive numbers for incidence and prevalence by age and sex, but using incidence figures from a Swedish study conducted in 1973, it is estimated that the incidence of Ménière disease in the US is 46 (new cases/100,000/year). No figures for sex and age are available, but the disease is relatively equal in males and females, and is extremely rare in children. Using extrapolation, the estimated prevalence is 1,150 (cases/100,000 population) Male child: 10/100,000 Female child: 10/100,000 Male adult: 560/100,000 Female adult: 560"/100,000 Predominant age Usual age of onset 20-60 Predominant gender Male = Female Causes Unknown. Best theory is inner ear response to variety of injuries (reduced middle ear pressure, allergy, endocrine disease, lipid disorders, vascular, viral, luetic). Recent theory is intracranial compression of balance nerve by blood vessel Risk factors Caucasian Stress Allergy Increased salt intake Noise Diagnosis Differential diagnosis Acoustic tumor Syphilis Perilymph fistula Multiple sclerosis Viral labyrinthitis Vertebrobasilar disease Other labyrinthine disorders producing same symptoms (Cogan's syndrome, benign positional vertigo, temporal bone trauma) Associated conditions Cochlear hydrops (hearing problem only) Vestibular hydrops (balance problem only) Drop attacks Associated conditions Cochlear hydrops (hearing problem only) Vestibular hydrops (balance problem only) Drop attacks Signs and symptoms Hearing loss - low frequency, fluctuating Vertigo - spontaneous attacks, duration 20 minutes to several hours Ear fullness Occurs as attacks, with intervening remission During severe attacks o Pallor o Sweating o Nausea and vomiting o Falling o Prostration o All symptoms aggravated by motion o Between attacks may experience motion-related imbalance without vertigo Laboratory Lab studies done to rule out other conditions Serologic tests specific for Treponema pallidum - microhemagglutination (MHA), fluorescent treponemal antibody (FTA), Treponema immobilization test (TPI) Thyroid studies Lipid studies Drugs that can alter labs Any medication that produces a significant degree of sedation is likely to affect vestibular testing and invalidate it Conditions that can alter labs Many conditions may produce auditory and vestibular findings identical to those associated with Ménière disease, making it a diagnosis of exclusion. A low frequency sensorineural hearing loss (nerve loss as opposed to conductive loss) is seen on audiometry, and a reduced caloric response on caloric testing is usual. Pathological findings Autopsy only. Shows dilation of inner ear fluid system (endolymph). Special tests Otoscopy with air pressure applied to the tympanic membrane Auditory o Hearing test (audiometry using pure tone and speech) to show low frequency sensorineural [nerve] loss and impaired speech discrimination) o Tuning fork test (Weber and Rinne) to confirm validity of audiometry o Auditory Brainstem Response audiometry (ABR) to rule out acoustic neuroma o Electrocochleography (ECOG) may be useful to confirm etiology Vestibular o Spontaneous nystagmus (rapid rhythmic eye motion) seen visually. Must avoid eye fixation by having patient use 40 diopter glasses for test. o Caloric testing - electronystagmography (ENG) may show reduced caloric response. Can obtain reasonably comparable information with use of 0.8 cc ice water instilled in ear canal, then noting duration and frequency of resulting nystagmus with 40 diopter lenses in place. Reduced activity on either side is consistent with Ménière diagnosis, but is not diagnostic. Imaging studies MRI to rule out acoustic tumor, which can produce identical symptoms and findings Treatment Treatment Appropriate health care Can usually be managed in outpatient setting. Inpatient for surgery. General measures Medications are given primarily for symptomatic relief of vertigo and nausea. There is no medication available that influences the disease process. For attacks, bedrest with eyes closed and protection from falling. Attacks rarely last longer than four hours. Streptomycin therapy for bilateral Ménière disease, when conventional management has failed. Streptomycin may be administered over a period of several days or weeks intentionally to damage the neuro-epithelium of the balance centers and reduce their function. Hearing must be carefully monitored during this time so that the treatment does not proceed to the point of damaging the hearing structures. This form of treatment should be administered only by an otolaryngologist and after careful patient education. Diet Limit total intake during attacks because of nausea. Otherwise diet is usually not a factor unless attacks are brought on by certain foods. A restricted salt diet may be useful in some cases. Activity Limit activity during attacks Between attacks patient may be fully active, but this may be limited by (1) fear of impending attack, (2) unsteadiness following attacks, (3) ear fullness or tinnitus, or (4) hearing loss in involved ear that may severely limit the patient's ability to perform work duties or to participate in social life Possible complications Failure to diagnose acoustic neuroma Loss of hearing Injury during attack Inability to work Medications Drugs of choice Acute attack. For severe episode, one of the following may be used. Adult doses are indicated o Atropine 0.2-0.4 mg IV o Diazepam (Valium) 5-10 mg IV slowly o Transdermal scopolamine, 1 patch, or smaller segment of patch, applied to skin surface and not replaced sooner than 3 days Maintenance. Adult doses are indicated (frequently must be reduced to avoid sedating effects) o Meclizine (Antivert, Bonine) 25-100 mg orally, either at bedtime or in divided doses o Ergotamine-belladonna-phenobarbital (Bellergal Spacetabs), one q 12 hr o Diazepam (Valium), 2 mg (or less) tid Contraindications Atropine - cardiac disease, especially supraventricular tachycardia and other arrhythmias Scopolamine - children and elderly Precautions Sedating drugs should be used with caution, particularly in elderly people. The need to reduce the dosage is common. Patients should be cautioned not to operate motor vehicles when they are sedated. Atropine, scopolamine, and Bellergal should be used with particular caution. If not prescribed frequently, refer to manufacturer's literature. Interactions Bellergal - oral anticoagulants, tricyclic antidepressants, phenothiazines, narcotics, beta blockers, estrogens, and others Transdermal scopolamine - anticholinergics, belladonna products, antihistamines, tricyclic antidepressants, and others Alternative drugs Acute attack o Droperidol, 1.5-2.5 mg IV slowly (in hospital setting) o Promethazine (Phenergan) 12.5-25 mg IV slowly o Diphenhydramine (Benadryl) 50 mg IV slowly o Carbogen (5% carbon dioxide and 95% oxygen) by mask from tank Maintenance o Dimenhydrinate (Dramamine) 50 mg q4-6h po o Promethazine (Phenergan) 12.5-25 mg q4-6h po o Diphenidol (Vontrol) 25-50 mg tid po o Diphenhydramine (Benadryl), 25-50 mg q6-8h po. Maximum, 100 mg/24 hours o Chlorothiazide (Diuril) 500 mg daily po with potassium supplement Follow-up Expected course Alternating attacks and remission Over time the balance problem tends to resolve, but the hearing worsens The great majority of patients can be managed successfully with medication. About 510% of patients require surgery for incapacitating vertigo. Very important not to overlook acoustic tumor, which produces an identical clinical picture Patient monitoring The most common complaint by Ménière patients regarding prior treatment is that the primary care physician did not take the condition seriously and that he or she did not seem interested in providing ongoing care. Because of the emotional impact alone, these patients need close followup care. It is important to monitor the status of their hearing, since it is at risk, and to continue to consider the possibility of a more serious underlying problem such as an acoustic tumor. Prevention and avoidance Reduce stress Reduce salt intake Don't smoke Avoid significant noise exposure, or use ear protectors Avoid use of ototoxic medications (aspirin, quinine, kanamycin, and many others) Patient education Many otolaryngologists keep booklets on Ménière disease as handouts. Ask your otolaryngology consultant for a supply. Miscellaneous Associated conditions Cochlear hydrops (hearing problem only) Vestibular hydrops (balance problem only) Drop attacks Age-related factors Pediatric Unusual, but occasional. Dizziness in children likely to be on basis of significant central nervous system disease. Geriatric Less likely to occur in elderly. Patients exposed to loud noise levels over many years are more susceptible. Other ages Usual onset age 20-60 Pregnancy Not a common problem, but difficult to treat because of risk of producing fetal abnormalities with medication Ménière syndrome Endolymphatic hydrops ICD9 codes 386.00: Meniere disease, unspecified Other notes Hearing loss References Lucente FE, Gady HE. Essentials of Otolaryngology. 4th ed. Philadelphia, Lippincott Williams & Wilkins, 1999:116-125 Web sites http://www.vestibular.org>Vestibular Disorders Association http://oto.wustl.edu/men>Washington University - The Ménière's Page http://www.geocities.com/hotsprings/spa/3143>Meniere&rtsinglequote;s Disease Home Page Author(s) Gale Gardner, MD Axial computed tomographic scan of the normal ear In an axial CT scan, several anatomic landmarks can be identified. These structures are important because their obliteration or alteration provides important clues in the diagnosis of otitic infections. A, superior CT section shows the head of the malleus and body of the incus, as well as the lateral semicircular canal (LSCC) and vestibule. The mastoid air cell system is well developed, with abundant pneumatization that emanates from the antrum. Middle ear infections often spread into the mastoid via the antrum. B, A CT section taken from a slightly more inferior position shows the turns of the cochlea (arrow). Acute infection of the inner ear structures can lead to permanent loss of vestibular function and profound deafness in the affected ear. Acute otitis media does not usually cause ossicular destruction. However, acute necrotizing otitis media, caused by -hemolytic streptococci, can lead to destruction of the blood supply to the ossicles and subsequent bony loss.