Nursing Process Study Guide Definition of Nursing Process Used to
advertisement

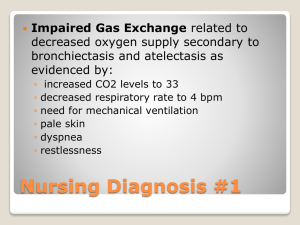
Nursing Process Study Guide Definition of Nursing Process Used to identify, diagnose and treat human RESPONSES to health and illness NURSING PROCESS STEP 1: ASSESSMENT= systematic collection of data 2 steps: Collection and verification of data from primary and secondary sources Analysis of data to develop nursing diagnoses and develop plans of care Purpose: to establish a plan about the client’s perceived needs, health problems and responses to these problems Data Collection Think critically about what to assess First: Observational Overview Second: differentiate important data Cue = information you obtain Inference = Your interpretation of cues Ex: patient crying = cue “patient is sad” = inference Problem focused approach Focus on patient situation and begin with problematic areas Ask follow-up assessment questions Types and Sources of Data 2 types of data: Subjective: stated by client Objective: observable or obtained by testing 2 sources of data Primary: provided by patient Secondary: provided by family/significant other, medical records, health care team Data Collection: Types of Data Subjective: (interview) “I am feeling nauseated.” Daughter states, “Dad hasn’t been eating for the past week.” Objective: (detected by observer) Skin cool to touch. Client’s face grimacing while turning in bed. BP 139/78. Lungs clear bilaterally. Data Collection: Interviewing “Planned conversation with a purpose” Purpose: to get/give info, identify problems, evaluate changes, teach, provide support and counseling Initial Interview Introduce yourself & explain your role Establish a caring, therapeutic relationship with the client Gain insight about patient’s concerns and worries Determine patient’s goals and expectations Obtain cues about what requires in-depth investigation Interviewing Approaches Two approaches: Direct: closed questions Nurse controls questioning highly structured to obtain specific information Ex: “What meds do you take?” Indirect: Open questions Client controls Ex: “What brought you into the hospital?” Objective Data Systematic collection of information through use of inspection, auscultation, palpation and percussion Usually carried out from head to toe Complete Exam versus Focused Exam Observation of Patient’s Behavior Level of function Are nonverbals matching verbal behaviors? Review of Diagnostic and Lab Data Results can identify or verify alterations identified in interview and physical exam. Next step: Validating Data “Double- Checking”: Is it Complete? “Validate data”: follow-up if conflict between subjective and objective information occur or extremely abnormal data exists BP today 200/160; yesterday was 140/90: Is it an error? Equipment malfunction? True reading that needs to be immediately reported? Patient crying but states “I am fine.” Discover reason for crying Next Step: Data Analysis Sort out normal from abnormal data Data Clustering: Recognize a pattern or trend; compare with standards; make a conclusion Pattern= 10lb weight loss, poor appetite, etc. Standard = no weight loss should occur Conclusion = Nutritional intake problem Assessment: Documenting Data Relate facts only, no interpretation Example: Ate 50% breakfast, not “good appetite” Record subjective data in client’s own words in quotes: Client states, “I am very sad.” Write legibly; use medical terminology; look up words you don’t know how to spell. NURSING PROCESS STEP 2: NURSING DIAGNOSIS After assessing the client, the next step is to form diagnostic conclusions to determine level of care. Consists of: Nursing diagnoses (treated by nurses) Collaborative problems (treated by several disciplines) Diagnosing NANDA official definition of a Nursing Diagnosis: A clinical judgment about individual, family, or community responses to actual or potential health problems (NANDA, 2005). A nursing diagnosis is the basis to select nursing interventions to achieve patient outcomes. A medical diagnosis is identification of a disease A collaborative problem is a complication that nurses monitor to detect the onset or changes in status. Medical or Nursing Diagnosis? Medical diagnosis refers to a disease process and is treated by a physician, PA or NP Nursing diagnosis refers to what nurses can treat independently based upon their judgment Describes a client’s physical, sociocultural, psychologic and spiritual response to an illness or health problem Medical vs. Nursing Diagnosis Example: Nurses are not educated to treat Diabetes, this is a medical diagnosis But nurses CAN diagnose Knowledge Deficit, Ineffective Coping or Imbalanced Nutrition, all which can accompany Diabetes Who Can Make a Nursing Diagnosis? Only RNs can make a diagnosis (= ANALYSIS of data) Other personnel (LPNS, CNAs) can contribute data and implement care Critical Thinking in Diagnosing Cluster data and recognize “defining characteristics” Compare data with “healthy patterns” It is a significant cue for a diagnosis if: Points to +/- change in health status (Ex: I have recently become SOB) Varies from norms of client population (Ex: BP > 140/90) Indicates developmental delay (Ex: 9 mo old baby should be able to sit; if not, this needs further assessment) Formulating Diagnosis Identify health problems, risk and strengths. Types of Nursing Diagnosis: Actual Risk Wellness Actual Diagnosis Problem is present at time of nursing assessment Based on associated signs and symptoms (Defining characteristics) Diagnosis: Risk Presence of risk factors indicates a problem is likely to develop unless nurses intervene Example: A patient who is immobile is at Risk for Impaired Skin Integrity Diagnosis: Wellness NANDA: “Describes human responses to levels of wellness in an individual, family or community that has readiness for enhancement” Indicates a patient’s STRENGTH that can be used to help coping Ex: Readiness for Enhanced Family coping Components of a Diagnosis: PES Problem (P) = NANDA dx Etiology (E) = “R/T” What contributes to the problem must be a condition nurses can treat Signs and symptoms (S) – “E/B” or “AMB” “Evidenced by” or “As Manifested By” = Defining characteristics shown by the client (symptoms/findings) Example: Ineffective Airway Clearance R/T Thick Secretions AMB Diminished Breath Sounds RLL and “Client states, I can’t breathe.” Nursing Diagnosis: Review Focus should be on what a nurse can impact: a RESPONSE to a health care problem Cannot be a medical diagnosis unless stated as a Collaborative Problem Errors in making diagnosis occur when: Cues overlooked Insufficient data collected Error in interpretation Errors in data clustering Errors in the diagnostic statement NURSING PROCESS STEP 3: PLANNING In this phase, Nurses: Set patient centered goals Prioritize problems/diagnoses. Plan outcomes: what is the desired health status of the client? Plan interventions: How can we help achieve the desired outcomes? Planning: Setting priorities Classify priorities as high, intermediate or low: Highest priorities= if untreated, will result in harm to the patient or others Example: adequate oxygenation, safety, comfort Intermediate priorities = non-emergent, non-life threatening needs Example: Imbalanced nutrition, activity intolerance Low priorities: needs that may affect future well being Consider: Maslow’s hierarchy of needs: Life threatening/Physiologic needs = highest priority Interaction of diagnoses: what is ROOT problem? Client’s priorities Resources available Planning Patient Goals and Outcomes Outcomes must be: specific, observable, measurable, realistic, based on client’s abilities and limitation with a time frame/deadline Good example: Client will ambulate down hallway by September 20th. Poor example: Client will walk better PLANNING: Selecting Interventions Safe and appropriate for age, health and conditions Achievable with resources available Congruent with client’s values, beliefs and culture Congruent with other therapies Based on nursing knowledge/rationale Within established standards of care determined by state law, prof. assoc and policies of agency Types of Interventions Independent Nurse-Initiated Interventions: Interventions that nurses are licensed to implement based on their education and experience May be performed without a physician’s order Examples: Assistance with ADLs, health education, health promotion, counseling Physician Initiated Interventions Require orders or institutional protocol Requires technical nursing knowledge Example: administering IM injection Collaborative Interventions: require combined knowledge of multiple health professionals Ex: Home care including PT/OT ****POCI – Problems linked with the Outcomes, Cause (Etiology) linked with Interventions. If you have POCI in your care plan, it is written correctly!**** NURSING PROCESS STEP 4: IMPLEMENTATION = Putting the Plan of Care into Action Includes performing or delegating the interventions AND documenting specific nursing interventions with the client’s resulting response Nurses Responsibilities while Implementing Care Review planned interventions for appropriateness Realistic, safe based on client condition Ex: order to ambulate but client feels dizzy today Congruent with client’s beliefs, values, culture Evidence based? Lies within standards of care, state Practice Act, professional organizations, and policies of institution IMPLEMENTATION Process Reassess patient: is intervention still appropriate? Review/revise care plan as necessary Organize resources Equipment, personnel, environment (safety), patient (comfortable) Anticipate and prevent complications Identify areas of assistance Supervising/Delegating Assess client and be sure delegation is appropriate for his/her care Ex: unstable VS not appropriate for CNA Check that person task delegated to has knowledge and skills to safely & effectively implement care Nurse is legally responsible that delegated task is performed properly Set expectations clearly and verify understanding of instructions Offer and receive effective feedback Provide Direct Care Skills in Implementing include: Cognitive: Knowing what to do and why Technical: Knowing how to do it Interpersonal: Communicating with the client while doing so EFFECTIVENESS of nursing action and perception of CARING depends on nurses ability to communicate Provide counseling Help client recognize and cope with stressful situations Provide emotional, intellectual and possibly spiritual support Involve client Nurses do not plan for client but engage in partnership with client and family Protect client’s right to autonomy in decision making supported by Patient’s Bill of Rights Teach client/family Essential independent aspect of nursing Patient’s Bill of Rights mandates Make referrals Help clients use resources to meet their needs Involves knowledge of community resources Document Client record is a legal document and admissible in court Confidentiality mandatory by HIPAA and ANA Code of Ethics Documenting Legally: If it’s not written, it is considered not done Meds: should be documented immediately to avoid error Other client information: can write on a worksheet and then record throughout the shift NURSING PROCESS STEP 5: EVALUATION = Did the Plan work? ****Plan can be revised at anytime if patient condition changes or interventions not appropriate Continuous activity Determine if outcomes are met or not and why. Process of Evaluating Evaluate client’s condition and compare with outcomes: Were the outcomes achieved? If yes: Relate nursing interventions to outcomes Were the interventions effective? Were the interventions what actually caused the goal to be met or did something else occur? If not: identify reasons why not achieved: Incomplete data collection/assessment resulted in inappropriate diagnosis Outcome not appropriate Interventions not appropriate Interventions not implemented appropriately Review: Nursing Process is: Assessing and organizing data Analyzing the data Make diagnosis from data Planning intervention strategies and determining outcomes. Implementing and documenting interventions Evaluating outcomes and interventions Sample correct care plan: Nutritional deficit R/T knowledge deficit AMB BMI of 17, labs reflect low calcium and potassium, client states “my hair is brittle” Outcomes: The patient will have a BMI of 18.5 by 9/17 The patient’s calcium and potassium levels will be within normal limits by 917. Interventions: The nurse will teach the client about calcium and potassium rich foods by using the My Plate manual. The nurse will work with the dietician and other nursing staff encouraging the client to choose proper foods from the hospital menu.