Infection - Skin to Skin Contact
advertisement
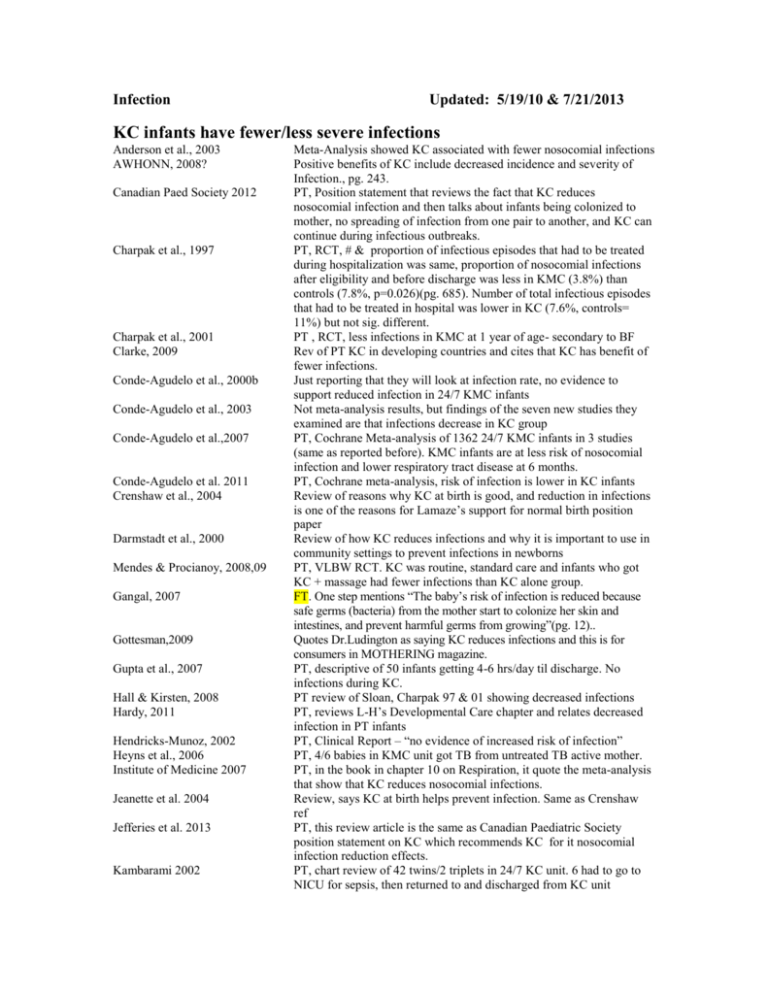
Infection Updated: 5/19/10 & 7/21/2013 KC infants have fewer/less severe infections Anderson et al., 2003 AWHONN, 2008? Canadian Paed Society 2012 Charpak et al., 1997 Charpak et al., 2001 Clarke, 2009 Conde-Agudelo et al., 2000b Conde-Agudelo et al., 2003 Conde-Agudelo et al.,2007 Conde-Agudelo et al. 2011 Crenshaw et al., 2004 Darmstadt et al., 2000 Mendes & Procianoy, 2008,09 Gangal, 2007 Gottesman,2009 Gupta et al., 2007 Hall & Kirsten, 2008 Hardy, 2011 Hendricks-Munoz, 2002 Heyns et al., 2006 Institute of Medicine 2007 Jeanette et al. 2004 Jefferies et al. 2013 Kambarami 2002 Meta-Analysis showed KC associated with fewer nosocomial infections Positive benefits of KC include decreased incidence and severity of Infection., pg. 243. PT, Position statement that reviews the fact that KC reduces nosocomial infection and then talks about infants being colonized to mother, no spreading of infection from one pair to another, and KC can continue during infectious outbreaks. PT, RCT, # & proportion of infectious episodes that had to be treated during hospitalization was same, proportion of nosocomial infections after eligibility and before discharge was less in KMC (3.8%) than controls (7.8%, p=0.026)(pg. 685). Number of total infectious episodes that had to be treated in hospital was lower in KC (7.6%, controls= 11%) but not sig. different. PT , RCT, less infections in KMC at 1 year of age- secondary to BF Rev of PT KC in developing countries and cites that KC has benefit of fewer infections. Just reporting that they will look at infection rate, no evidence to support reduced infection in 24/7 KMC infants Not meta-analysis results, but findings of the seven new studies they examined are that infections decrease in KC group PT, Cochrane Meta-analysis of 1362 24/7 KMC infants in 3 studies (same as reported before). KMC infants are at less risk of nosocomial infection and lower respiratory tract disease at 6 months. PT, Cochrane meta-analysis, risk of infection is lower in KC infants Review of reasons why KC at birth is good, and reduction in infections is one of the reasons for Lamaze’s support for normal birth position paper Review of how KC reduces infections and why it is important to use in community settings to prevent infections in newborns PT, VLBW RCT. KC was routine, standard care and infants who got KC + massage had fewer infections than KC alone group. FT. One step mentions “The baby’s risk of infection is reduced because safe germs (bacteria) from the mother start to colonize her skin and intestines, and prevent harmful germs from growing”(pg. 12).. Quotes Dr.Ludington as saying KC reduces infections and this is for consumers in MOTHERING magazine. PT, descriptive of 50 infants getting 4-6 hrs/day til discharge. No infections during KC. PT review of Sloan, Charpak 97 & 01 showing decreased infections PT, reviews L-H’s Developmental Care chapter and relates decreased infection in PT infants PT, Clinical Report – “no evidence of increased risk of infection” PT, 4/6 babies in KMC unit got TB from untreated TB active mother. PT, in the book in chapter 10 on Respiration, it quote the meta-analysis that show that KC reduces nosocomial infections. Review, says KC at birth helps prevent infection. Same as Crenshaw ref PT, this review article is the same as Canadian Paediatric Society position statement on KC which recommends KC for it nosocomial infection reduction effects. PT, chart review of 42 twins/2 triplets in 24/7 KC unit. 6 had to go to NICU for sepsis, then returned to and discharged from KC unit Kambarami et al, 1998 Kirsten & Kirsten 2000 Lamy Filho et al. 2013 Lawn et al., 2010 Lazarazo et al. 2012 Mendes & Procianoy 2009 Mendes & Procianoy, 2008 Rao et al., 2008 Schanler et al., 2005 Sizun et al., 2004 Sloan et al., 1994 Sosa et al., 1976 Suman et al. 2008 2013 PT, RCT, 37 KC (24/7 KC) infants “were ill less frequently” than 37 controls. PT, RCT BF in KMC reduced incidence of NEC (10% vs 2.8%) PT, RCT to determine if 28 hours of more of KMC over 7 days reduced colonization of nostrils of infants who have MRSA. Both groups reduced colonization, but twice as many KMCers did than controls. Meta analysis of KMC. It is particularly effective in reducing severe morbidity, particularly from infection. PT, retrospective chart review of 374 24/7 KMC PTs who had shorter length of stay, more stable temp and fewer nosocomial infections PT, RCT, VLBW. Less infection in KC + massage group than in KC alone group. PT, RCT, VLBW. Less infection in KC+massage (4 times a day from 48 hours oflife until discharge) than KC alone infants. PT, RCT, more controls than KMCers had nosocomial sepsis (p.19) PT, RCT, infants in mother’s own milk group (who also got significantly more episodes and significantly more duration of KC than preterm formula and donor milk groups) had fewer infection events (late onset sepsis, UTI, meningitis, NEC), but KC per se was not correlated to number of infection-related events. States that KC has shown fewer infections in developing countries but that these findings may not be relevant in high tech countries. Cites Charpak et al., 2001 as source of infection data. PT, RCT, decrease in severe infections such as pneumonia, septicemia in KMC infants over first 6 months of life In all 3 RCTs, FT infants who got 45 min of KC beginning after episiotomy repair had fewer episodes of infection (moniliasis, impetigo, and medicated illness). PT, FT (SGA) RCT of 24/7 KMC and KMC infants had fewer infections than controls. PT, reports that l hr of KMC in am and again in pm per day for 7 days decolonized mrsa infected infants but controls also were decolonized over this time period but were only half the number decolonized in the KC group. KC infants have more/more severe infections OR is risk factor for it Sakaki et al., 2009 PT, Descriptive prospective study of incidence of MRSA among 961 infants. KMC was a predictor of MRSA. Visser et al., 2008 PT, descriptive of 23 preterm infants who came down with nosocomial RSV associated pneumonia one month after same strain appeared in general pediatric ward of same hospital in Gauteng, South Africa. There is also a reference for TB spreading in KMC wards KC infants have no different infection rates than other infants/ no diff between maternal & paternal KC on infection rates Bauer, Sontheimer,et al., 1996 Cerezo & deLeon, 1992 Charpak et al., 1997 PT, VLBW, infection rate measured with maternal and paternal KC No difference between mat/paternal KC and infection rate. No sig diff by blood cultures and no sig diff in other cultures PT, RCT, # & proportion of infectious episodes that had to be treated during hospitalization was same, proportion of nosocomial infections after eligibility and before discharge was less in KMC (3.8%) than controls (7.8%, p=0.026)(pg. 685). Number of total infectious episodes Filho et al. 2008 Ghavane et al. 2012 Kadam et al., 2005 that had to be treated in hospital was lower in KC (7.6%, controls= 11%) but not sig. different. PT, clin eval of 8 NICUs with KC stepdown vs 8 units without KC stepdown. No difference in infections between units. PT, RCT micropreemie, no difference in infection rate between 24/7KMC unit and NICU incubator groups PT, RCT. # of sepsis in KMC =6, control =8. 6 KMC babies transferred back to regular care due to klebsiella pneumoniae. One KMC baby died from sepsis. Overall, no sig diff in sepsis incidence. Mechanisms by which KC affects infection Abouelfettoh et al., 2010 Canadian Ped Society 2012 Darmstadt et al., 2000 Gangal, 2007 Odent, 1989 Schanler 2001 WHO 1998 PT, descriptive study of 5 days of KC effects on skin hydration (increased) and TEWL (increased) and # of infections during hospitalization and within one month of discharge (no infections after KC). PT, Position statement that reviews the fact that KC reduces nosocomial infection and then talks about infants being colonized to mother, no spreading of infection from one pair to another, and KC can continue during infectious outbreaks. Review of how KC reduces infections and why it is important to use in community settings to prevent infections in newborns (Protection from mother’s milk) FT. One step mentions “The baby’s risk of infection is reduced because safe germs (bacteria) from the mother start to colonize her skin and intestines, and prevent harmful germs from growing”(pg. 12).. FT, Clin Report- baby feeds at breast right after delivery in KC and Gets lots of IgA antibodies and zinc and enzymes in colostrums. PT, review article says that KC provides specific protection over infection due to enteromammary pathway and possibly a dermal pathway FT. states that when a mother and her baby are in KC the baby is exposed to the normal bacterial on t`e mother’s skin, whIch may protect the baby from "becoming sick due to harmful germs.” Related Issues: Staff Perception Mallet et al., 2007 Trevisanuto et al., 2013 PT, Descriptive study of French NICU staff knowledge and barriers. Fear of nosocomial infection is a barrier to KC use. PT, 54 NICU providers ideas of what would reduce neonatal infections in Vietnam included KMC as a priority for prevention and control of infection in provincial hospitals in south and south central Vietnam. Hand washing, exclusive breastfeeding and safe disposal of medical waste were nominated by most participants as priorities for preventing neonatal infections. Education through instructional posters and written guidelines, family contact, kangaroo-mother-care, limitation of invasive procedures and screening for maternal GBS infection were advocated by a smaller proportion of participants. Related Literature InsTitute on Medicine, 2 02 Report of Preterm Birth conchudes that ‘stress’ and ‘infection’ contribute to"the racial-ethnic difference in infant mortality rate. Pammi, M., Abrams, SA. (2011) Oral lactoferrin fov the prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst Review Oct. 5 (10): CD00711177 Lactoferrin is a normal component of COLostrRUM, human milk, human saliva and tears. Oral lactoferrin reduces late-onset sepsis in VLBW infants