Traumatic Dislocation of the Hip Joint
advertisement

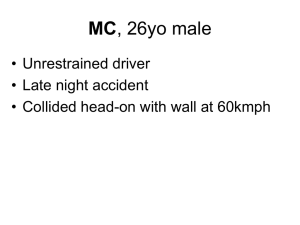
Lower limbs trauma 2010 first lecture Dr .Alaa A. Hussein Al-algawy Traumatic Dislocation of the Hip Joint Traumatic dislocation of the hip joint may occur with or without fracture of the acetabulum or the proximal end of the femur. It is most common during the active years of life and is usually the result of high-energy trauma, unless there is preexisting disease of the femoral head, acetabulum, or neuromuscular system. The head of the femur cannot be completely displaced from the normal acetabulum, unless the ligamentum teres is ruptured or deficient because of some unrelated cause. Traumatic dislocations are classified according to the direction of displacement of the femoral head from the acetabulum. Posterior Hip Dislocation Usually, the head of the femur is dislocated posterior to the acetabulum when the thigh is flexed, for example, as may occur in a head-on automobile collision when the knee is driven violently against the dashboard. Posterior dislocation is also a complication of hip arthroplasty. Clinical features :The significant clinical findings are shortening, adduction, and internal rotation of the extremity. Anteroposterior, lateral and, if fracture of the acetabulum is demonstrated, oblique radiographic projections (Judet views) are required. Common associated injuries : include fractures of the acetabulum or the femoral head or shaft and sciatic nerve injury. The head of the femur may be displaced through a tear in the posterior hip joint capsule. The short external rotator muscles of the femur are commonly lacerated. Fracture of the posterior margin of the acetabulum can create instability. Reduction: If the acetabulum is not fractured or if the fragment is small, reduction by closed manipulation is indicated. General anesthesia provides maximum muscle relaxation and allows gentle reduction. Reduction should be achieved as soon as possible, preferably within the first few hours after injury, as the incidence of avascular necrosis of the femoral head increases with time until reduction. The main feature of reduction is traction in the line of deformity followed by gentle flexion of the hip to 90 degrees with stabilization of the pelvis by an assistant. While manual traction is continued, the hip is gently rotated into internal and then external rotation to obtain reduction. The stability of the reduction is evaluated clinically by ranging the extended hip in abduction and adduction and internal and external rotation. If stable, the same movements are repeated in 90 degrees of hip flexion. The point of redislocation is noted, the hip is reduced, and an anteroposterior radiograph of the pelvis is obtained. Soft tissue or bone fragment interposition will be manifested by widening of the joint space as compared to the contralateral side. 1 Indication of surgery : Irreducible dislocations, open dislocations, and those that redislocate after reduction despite hip extension and external rotation (usually because of associated posterior wall fracture of the acetabulum) are indications for immediate open reduction and internal fixation if necessary. Most authors agree that a widened joint space on radiograph, despite a stable reduction, is also an indication for immediate arthrotomy. Others prefer obtaining a CT scan first, to further delineate the incarcerated fragments and associated injuries before surgery. Minor fragments of the posterior margin of the acetabulum may be disregarded, but larger displaced fragments are not usually successfully reduced by closed methods. Open reduction and internal fixation with screws or plates is indicated. Post reduction treatment will vary according to the type of initial surgery. A strictly soft-tissue injury with a stable concentric reduction may be treated with light skin or skeletal traction for a few days to a week before exercises are begun. Complications : include infection, avascular necrosis of the femoral head, malunion, posttraumatic degenerative joint disease, recurrent dislocation, and sciatic nerve injury. Sciatic nerve injury is present in 10–20% of patients with posterior hip dislocation. Although usually of the neurapraxia type, these lesions leave permanent sequelae in about 20% of cases. Anterior Hip Dislocation : Anterior dislocation of the hip is rare compared to its posterior counterpart. It usually occurs when the hip is extended and externally rotated at the time of impact. Associated fractures of the acetabulum and the femoral head or neck occur rarely. Usually, the femoral head remains lateral to the obturator externus muscle but can be found rarely beneath it (obturator dislocation) or under the iliopsoas muscle in contact with the superior pubic ramus (pubic dislocation). The hip is classically flexed, abducted, and externally rotated. The femoral head is palpable anteriorly below the inguinal flexion crease. Anteroposterior and transpelvic lateral radiographic projections are usually diagnostic. Closed reduction under general anesthesia is generally successful. Here also the surgeon must make sure of a concentric reduction comparing both hip joints on the post reduction anteroposterior radiograph. The patient starts mobilization within a few days when pain is tolerable. Active and passive hip motion, excluding external rotation, is encouraged, and the patient is usually fully weight bearing by 4–6 weeks. Skeletal traction or spica casting may rarely be useful for uncooperative patients. first lecture 2 Treatment The injury follows major trauma, so initial treatment is directed at assessment and resuscitation of the patient. Neurological injuries must be assessed and documented. The dislocated hip should be reduced as an emergency and other fractures addressed subsequently. 1. Closed reduction should be performed within 6 hours of the dislocation. This can sometimes be achieved in the emergency room, with adequate analgesia but often a full general anesthetic is required. With a posterior dislocation, greater mechanical advantage for traction can be achieved with the patient on the operating room floor. If the reduction is stable, 2.5 to 5 kg of skin or skeletal traction should be applied. AP X-rays will confirm the reduction, and when there is doubt about the congruity of the reduction, a CT scan should be obtained. 2. Immediate open reduction is required when the dislocation cannot be reduced or the hip is grossly unstable. The joint should be opened, the hip reduced and the rim fracture stabilized. 3. Retained loose fragments should be removed by arthrotomy or hip arthroscopy. Fragments can abrade the articular surface and accelerate post traumatic degenerative change. 4. Significant rim fractures require open reduction and internal fixation under appropriate conditions. Where there is less than one third of the posterior rim remaining, the hip may be unstable. 5. Mobilization can start after closed or open reduction as soon as pain allows. patients should start to move the hip early and be mobilized when their pain permits, usually around 5 to 10 days, with partial weight-bearing for 6 weeks, increasing to full weight-bearing over the next 6 weeks. Prognosis: The prognosis is related to the period of dislocation, velocity of the trauma and extent of any associated fracture. A simple dislocation carries a better prognosis than a large rim fracture, and a delay in reducing the hip of greater than 24 hours carries a poor outcome. Excellent or good results, in terms of pain, return to function and degenerative change, can be expected in 7 5% of patients with an anterior dislocation . Avascular necrosis and post-traumatic osteoarthritis may occur up to 5 years after a dislocation. first lecture 3 Complications 1- Avascular necrosis: IO-35% . 2-Post-traumatic osteoarthritis: 20-30%. 3-Heterotopic bone formation: 3%. 4- Sciatic nerve palsy: 10-19%. HIP FRACTURE Fractures of the proximal femur involving the intertrochanteric and neck regions of the femur are very common injuries. They typically occur in elderly female patients. Anatomy, classification and epidemiology Fractures of the hip are divided into two main groups depending on their relationship to the capsule of the hip joint. 1 - Intracapsular fractures Fractures of the subcapital and mid-cervical region of the femoral neck. .2- Extracapsular fractures Fractures at the base of the neck or in the trochanteric region . The vascular supply of the femoral head is also of paramount importance. There are three main sources of vascular supply: (1) the retinacular vessels arising from the lateral femoral circumflex artery and the inferior metaphyseal artery and then running beneath the synovium along the neck, which they penetrate proximally both anteriorly and posteriorly; (2) the interosseous circulation crossing the marrow spaces from distal to proximal; and (3) unreliably, the ligamentum teres artery. Fractures of the femoral neck always disrupt the interosseous circulation; the femoral head then relies only on the retinacular arteries, which may also be disrupted or thrombosed . Secondary avascular necrosis of part or all of the femoral head can result. the incidence of nonunion is very high . Intertrochanteric fractures usually do not suffer this same fate. The capsule (and vessels) are still attached to the proximal fragment after fracture, and thus the blood supply remains patent. The demographic features of both injuries are similar - they usually occur in older female patients. The mean age is 75 years and the female male ratio is 4 to 1. Dementia or some degree of cognitive impairment is common and typically present in 25-30% of cases. Significant medical comorbidities are present in 70% of patients Clinical findings: There is usually a history of a fall. In displaced Intracapsular or Extracapsular fractures the leg is typically shortened and externally rotated. Neurovascular injury is very rare, but about 10% of patients will have an additional fracture, usually a proximal humeral or distal radial fracture. first lecture 4 Management: In the past some of these fractures were treated non-operatively in traction, but in modern orthopaedic practice there is no role for this unless the patient is moribund on admission and not expected to survive. Intracapsular fractures Femoral Neck Fractures Femoral neck fractures are intracapsular fractures. Because of the already mentioned unusual vascularization of the femoral head and neck, these fractures are at high risk of nonunion or avascular necrosis of the femoral head. The incidence of avascular necrosis increases with the amount of fracture displacement and the amount of time before the fracture is reduced. Fractures of the femoral neck occur most commonly in patients over age of 50 . The involved extremity may be slightly shortened and externally rotated. Hip motion is painful, except in the rare cases of nondisplaced or impacted fractures, where pain may be evident only at the extremes of motion. Good quality anteroposterior and lateral radiographs are mandatory. Classification The Garden classification for acute fractures is the most widely used system: Type 1: Valgus impaction of the femoral head Type 2: Complete but nondisplaced Type 3: Complete fracture, displaced less than 50% Type 4: Complete fracture displaced greater than 50% This classification is of prognostic value for the incidence of avascular necrosis: The higher the Garden number, the higher the incidence. The benefits of either skeletal or skin traction are unclear prior to definitive treatment. Traction may offer comfort in some patients but do not improve overall outcome. Undisplaced intracapsular fractures are generally treated by internal fixation using screws. Although they can be treated non-operatively, 15% will displace and it is safer to treat these injuries surgically. Avascular necrosis occurs in 5% of cases and conversion to arthroplasty may be required later if this is symptomatic, Displaced intracapsular hip fractures are almost always in the subcapital region of the femoral neck. Reduction and fixation is possible, but there is a high rate of early nonunion and fixation failure. Avascular necrosis affects about 15% of those that do unite. Overall, 40% of patients treated in this way will require conversion to some form of hip arthroplasty at a later stage. first lecture 5 Most surgeons, therefore, choose to treat the majority of these patients with an arthroplasty in the first instance. Reduction and fixation should be considered in younger patients (<60 years). However, many younger patients with these injuries have risk factors that predispose to osteoporosis (alcohol abuse, steroid treatment, epilepsy treatment, renal or other metabolic bone disease). If risk factors are present then arthroplasty should be considered For most displaced intracapsular hip fractures, hip arthroplasty is the treatment of choice. The choices are either some form of hemi-arthroplasty or a total hip arthroplasty Complications The most common sequelae of femoral neck fractures are loss of reduction with or without hardware failure, nonunions or malunions, and avascular necrosis of the femoral head. This latter complication can appear as late as 2 years after injury. According to different series, the incidence of avascular necrosis for Garden type 1 fractures varies from 0 to 15%, for type 2 fractures 10–25%, for type 3 fractures 25– 50%, and for type 4 fractures 50–100%. Secondary degenerative joint disease appears somewhat later. Extracapsular fractures Extracapsular hip fractures in the trochanteric region of the proximal femur. The clinical features are the same as for subcapital hip fractures. Characteristically, the fracture occurs in an elderly female and the leg is shortened and externally rotated at presentation Since the blood supply of the femoral head is not endangered, internal fixation is the treatment of choice. The most commonly used device is a sliding hip screw and plate. Alternative devices that involve intramedullary fixation are also commonly used, particularly for subtrochanteric fractures, especially if they extend a long way down the femoral shaft The main complications of surgery are failure of fixation (<5%), non-union (1-2%) and infection (<5%). Treatment The aim of treatment is to achieve early mobilization of the patient, avoiding the attendant complications of prolonged bed rest. Young patients should be treated in the same manner. Rehydration and urgent medical assessment of all patients is vital. Surgery should be performed within 48 hours of the fracture, as confusion, pneumonia, the incidence of pressure sores and the duration of hospital stay all increase significantly after a period if surgery is further delayed. first lecture 6 1. Closed treatment, with skin or skeletal traction for 6-8 weeks will usually achieve sound union and should be reserved for the 2 or 3% of patients where surgery is contraindicated or declined. Undisplaced fractures can be treated with early mobilization and partial weight-bearing. The fracture should be reassessed regularly with X-rays. Where pain persists, the fracture displaces or the patient is unable to cooperate with mobilization, internal fixation should be performed. 2. Internal fixation is the treatment of choice, followed by early mobilization and weight-bearing as tolerated. Careful placement of the patient on the fracture table is essential and an anatomical reduction can often be achieved before opening the fracture. A variety of devices may be used a sliding hip screw-plate system a ( dynamic hip screw) is the most popular. Short intramedullary devices may be used, but are less popular. Flexible IM nails, inserted into the femoral neck and head from the condylar region. Subtrochanteric fractures can be treated with a sliding hip screw or of an intramedullary device by closed means with sound fixation by locking screws into the femoral head is preferable. 3. Isolated greater and lesser trochanter fractures are rare and can usually be treated symptomatically Outcome after hip fracture: Irrespective of the location of the hip fracture, the outcome is frequently poor. This is more a reflection of the frail medical state of these patients, rather than the nature of the surgery required. The 1-year mortality rate for all hip fractures is 30%, but in demented patients it is 50% . Rehabilitation in a non-acute institution is required in 35-40% of patients. Ultimately 70% of patients return home, but the remainder require some form of residential care. first lecture 7