Cranial Nerve Tests
advertisement

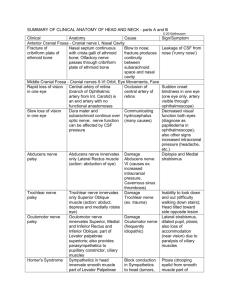
Cranial Nerve Tests Olfactory Nerve - applying substances with different odors to each nostril in turn Fractures of anterior cranial fossa or cerebral tumors of frontal lobes may produce lesions of olfactory nerves Anosmia - loss of smell Optic Nerve First ask patient if any changes in eyesight have been noted Acuity tested by using charts with lines of print of varying size Examination of optic disc - intracranial subarachnoid space extends forward around the optic nerve to back of eyeball Retinal artery and vein run in optic nerve Rise in CSF pressure in subarachnoid will compress thin walls of retinal vein Results in congestion of retinal veins, edema of retina, and bulging of optic disc (papilledema) Visual field tests Central scotoma - loss of central area of the field Hemianopia - blindness in one-half of each visual field Homonymous hemianopia - loss of same region of field in both eyes Lesion of optic tract and optic radiations Bitemporal hemianopia - lateral halves of fields of both eyes are lost Most commonly caused by tumor of pituitary, pressing on optic chiasm, where visual information crosses Oculomotor Supplies all orbital muscles except superior oblique and lateral rectus Also supplies levator palpebrae superioris, smooth muscles related to accommodation (sphincter pupillae and ciliary muscle) Complete third nerve paralysis - the eye cannot be moved upward, downward, or inward At rest, the eye looks laterally (external strabismus) - lateral rectus pulls laterally, superior oblique pulls down Patient will have double vision (diplopia) and ptosis (drooping of eyelid, loss of levator palpebrae superioris)( Pupil is widely dilated and unresponsive to light Accommodation of eye is paralyzed Trochlear Innervates superior oblique Fourth nerve paralysis - Patient will complain of double vision and looking straight downward Because SO is paralyzed, the eye will move medially as the inferior rectus pulls the eye downward Trigeminal Sensory and motor roots Sensory root - passes to trigeminal ganglion Opthalmiic (V1) Maxillary (V2) Mandibular (V3) Motor root - joints mandibular division Sensory function test - cotton wisp over each area of the face supplied by divisions of trigeminal nerve Motor function - ask patient to clench teeth Masseter and temporalis can be palpated to determine if they are contracting Facial Nerve Supplies muscles of facial expression, supplies anterior 2/3 of tongue with taste fibers, and is secretomotor to lacrimal, submandibular, and Sublingual glands Motor function test - patient asked to show teeth by separating the lips with teeth clenched, and then close eyes Taste on each half of tongue can be tested for different types of taste Upper motor neuron lesion - corticobulbar fibers from both cerebral cortices also innervate muscles of upper part of face Upper motor neuron lesion will leave corticobulbar fibers intact - paralysis to lower part of face Lower motor neuron lesion - all muscles on affected side of face will be paralyzed Lower eyelid will droop, angle of mouth with sag, tears will flow from lower eyelid, and saliva will dribble from corner of mouth Patient will be unable to close eye and cannot expose teeth fully on affected side Loss of taste over anterior 2/3 of tongue - seventh nerve damage proximal to point where it gives off chorda tympani Vestibulocochlear Innervates utricle and saccule, vestibular system, sensitive to changes in dynamic equilibrium Also innervates cochlea, sensitive to sound Disturbances of vestibular function - include dizziness (vertigo) and nystagmus (uncontrollable pendular movement of eyes) Disturbances of cochlear function reveal themselves as deafness and ringing in ears (tinnitus) Sensory tests - patient's ability to hear voice of tuning fork should be tested, with each ear tested separately Glossopharyngeal nerve Supplies stylopharnygeus muscle and sends secretomotor fibers to parotid gland Sensory fibers innervate posterio 1/3 of tongue Sensory test - patient's general sensation and that of taste on posterior third of tongue 1 Vagus Need to test branches to pharynx, soft palate, and larynx Pharyngeal reflex - touch lateral wall of pharynx with spatula, should cause patient to gag Soft palate test - ask patient to say "ah" Normally, soft palate rises and uvula moves backward in midline All muscles of larynx are supplied by recurrent laryngeal branch of vagus, except cricothyroid muscle (external laryngeal branch) Hoarseness of loss of voice can occur if recurrent laryngeal is damaged Accessory Nerve Supplies sternocleidomastoid and trapezius muscle by its spinal part Motor test - ask patient to rotate head to one side against resistance, causing SCM of opposite side to come into action Also, ask patient to shrug the shoulders Hypoglossal nerve Supplies muscles of the tongue Lesion - tongue will deviate towards the paralyzed side One of genioglossus muscles, which pull tongue forward, is paralyzed on affected side The other normal genioglossus muscle pulls unaffected side of tone forward, leaving paralyzed side stationaly This leads tip of tongue to deviate toward paralyzed side Long-standing paralysis - muscles on affected side are wasted, and tongue is wrinkled on that side Localizing the lesion Sixth and seventh nerves not functioning - suggests lesion within pons of brain Eighth and seventh nerves not functioning - suggests a lesion in internal acoustic meatus Excessive sensitivity to sound in one eary - lesion probably involves nerve to stapedius Loss of taste over anterior 2/3 of tongue - seventh nerve damage proximal to point where it gives off chorda tympani Abducens Innervates lateral rectus Sixth nerve paralysis - patient cannot turn eye laterally When looking straight ahead, lateral rectus is paralyzed, so unopposed medial rectus pulls eyeball medially Internal strabismus 2