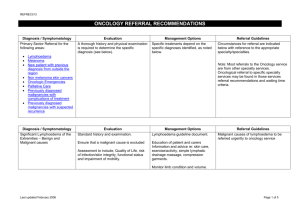
Referral Guidelines
advertisement

REFREC019 PAIN MANAGEMENT REFERRAL RECOMMENDATIONS Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Pain management problems are addressed under the following headings: Acute back pain Cancer pain Headache Persistent pain Shingles Last updated February 2006 Page 1 of 7 REFREC019 Diagnosis / Symptomatology Acute Back Pain Evaluation History and physical examination. Exclude rare serious conditions requiring urgent investigation/interventions (‘Red Flags’): Infection (Discitis, Osteomyelitis) (.5%) Fracture (Osteoporosis!) (3%) Tumour (1%) Cauda Equina Syndrome/widespread bilateral motor weakness Realise that majority (95%) of low back pain is non-specific; in these cases do not perform routine plain X-rays or other investigations. Common findings in patients with low back pain also occur in asymptomatic people and may not be cause of pain! A specific patho-anatomic diagnosis is not necessary; differentiation between somatic referred pain and radicular pain might be useful. Consider early in evaluation psychosocial and occupational risk factors for pain becoming chronic (‘Yellow Flags’) Prior history of low back pain. Poor physical fitness/general health. Smoking. Psychological distress/depression. Disproportionate pain behaviour. Last updated February 2006 Management Options Referral Guidelines Provide effective communication along the lines of: ‘Back pain is not a disease, but a common bodily symptom and activity intolerance’. Avoid alarming diagnostic labels (‘disc out of place, trapped nerve’). Use neutral terms (‘symptom of physical dysfunction, out of condition’). Address natural history of early recovery, but possibility of recurrence and persistent mild symptoms. Refer Category 2 for acute back pain episodes exceeding 3 months duration without improvement and persistent significant functional impairment/disability. Develop management plan with patient Advice to stay active. Advice to avoid bed rest. Advice to return early to work, even if only light duties. Use of short course of manipulation. Advice to use heat wraps. Use of analgesics as required (paracetamol, NSAIDs, tramadol, opioids [only shortterm]) to facilitate above treatment goals. Consider comedication with low dose tricyclics and/or in particular in radicular pain anticonvulsants. Review carefully if symptoms persist and disability develops – be aware of the relevance of ‘yellow flags’ for the progression from acute to chronic pain, while clinical factors are only weak predictors. Page 2 of 7 REFREC019 Last updated February 2006 Low job satisfaction. Personal problems. Medicolegal proceedings. If persistence beyond 6 weeks Initiate incremental aerobic exercise and fitness programme. Apply behavioural medicine principles. Liaise with workplace. Page 3 of 7 REFREC019 Diagnosis / Symptomatology Cancer Pain Evaluation History and physical examination. Assess type, severity and localisation of pain consider occurrence of multiple pains of various origins in many cancer patients. consider relevance of symptoms other than pain in cancer patients. Assess physical, but also functional, psychosocial and spiritual dimensions of pain include assessment of anxiety, depression, beliefs of patient. pay attention to cultural, ethnic and linguistic factors of pain experience. Management Options Referral Guidelines Follow principles of WHO analgesic ladder start at step appropriate for pain severity. adjust use of analgesics to alteration of pain type/severity. change step, not within step, if pain severity increases. try opioids in all patients with moderate to severe pain regardless of aetiology of pain. do not delay initiation of opioids due to unfounded fears and reassure patients and relatives about their fears. prescribe analgesia for continuous pain on regular basis, not PRN. prescribe all patients on regular opioids breakthrough analgesia at 1/6th of daily dose. titrate opioid doses to maximum effect and minimum side effects. while using opioids offer laxatives and antiemetics as needed. change strong opioid if intolerable side effects. use oral route whenever possible, subcutaneous only if oral route unavailable. consider adjuvant analgesics in defined pain states, eg neuropathic pain: tricyclics, anticonvulsants. Consider involvement of palliative care services and hospices as well as oncology and radiotherapy services Last updated February 2006 Refer Category 1 for any of the following: lack of access to above services. need for pain specialist assessment in unresponsive pain. need for interventional pain management techniques established. consider pain relieving anticancer therapy and radiotherapy in defined situations. Page 4 of 7 REFREC019 Diagnosis / Symptomatology Headache Evaluation History and physical examination Assess nature and speed of onset, duration, frequency, severity and quality, location, alleviating/exacerbating factors, response to analgesics, history and pattern of previous headaches, change from previous headaches, family history, associated symptoms and neurology, current medications (including frequency and dosing of analgesics), past medical history, depression. Management Options Follow options outlined in neurology referral recommendations. Referral Guidelines Consider referral to neurology services along neurology referral recommendations. Refer Category 3 for persistent headaches with impairment of function and/or quality of life or disability and pain unresponsive to treatment. Perform neurologic examination, mental status, head, neck, eye examination. Exclude rare serious conditions requiring urgent investigation/intervention: Intracranial haemorrhage Intracranial tumour Intracranial infection Increased intracranial pressure Acute glaucoma Exclude other pathology causing headaches: Sinusitis Dental pathology Ocular pathology Vasculitis Establish diagnosis along the criteria of the International Headache Society (IHS). Last updated February 2006 Page 5 of 7 REFREC019 Diagnosis / Symptomatology Persistent Pain (not further specified) Evaluation History and physical examination. Exclude pain as a symptom of treatable underlying diagnosis by appropriate diagnostic measures, investigations and specialist referrals as required. Attempt to establish a diagnostic category: Nociceptive pain Neuropathic pain Identify ‘pathological’ pain, not to be misunderstood as in general of psychological/psychiatric origin, but often as a result of peripheral and central sensitisation. Examples of such ‘pathological’ pain states are Phantom limb pain Fibromyalgia Most chronic back pain Many visceral pain conditions such as irritable bowel syndrome, interstitial cystitis, loin pain haematuria syndrome Last updated February 2006 Management Options Explanation of symptoms and syndromes, often perceived as bizarre and ‘inappropriate’ by patients, relevant others and even health care professionals. Referral Guidelines Refer Category 3. Refer Category 2 in selected special circumstances outlined by referrer. Development of a management plan together with patient, which considers the biopsychosocial model of chronic pain and follows principles of behavioural medicine. In nociceptive pain (eg osteoarthritis) use of appropriate analgesics including regular paracetamol, NSAIDs, tramadol and even opioids should be tried, but only continued if resulting in significant pain relief and/or more importantly improvement of function. In neuropathic pain (eg diabetic polyneuropathy) use of tricyclics, anticonvulsants, tramadol and even opioids should be tried, but only continued if resulting in significant pain relief and/or more importantly improvement of function. In ‘pathological’ pain states analgesics are usually ineffective and initiation of opioids potentially harmful; again anticonvulsants and tricyclics can be tried as modifying sensitisation processes. Emphasis here should lie on physical activation and aerobic fitness programmes, cognitivebehavioural approaches and reintegration into work force. Page 6 of 7 REFREC019 Diagnosis / Symptomatology Shingles Postherpetic Neuralgia (PHN) Evaluation History and physical examination. Early diagnosis is encouraged; prodromal pain before the rash appears is possible. Increased risk of PHN development in advancing age (> 50 years) severe pain with rash prodromal pain Management Options Antiviral therapy for all patients with shingles within 72 hours of rash onset valaciclovir preferred agent as increased pain resolution Aggressive and effective acute pain management utilising titration with non-opioids (paracetamol), NSAIDs, tramadol and opioids. Additional systemic steroid use confers slight benefit on acute pain and quality of life with no effect on long-term pain and could be considered. Referral Guidelines Refer Category 1 for any of the following as early treatment prevents PHN: acute shingles with pain unresponsive to treatment early development of severe neuropathic pain after rash has healed Refer Category 3 for established PHN with impairment of function and/or quality of life or disability and pain unresponsive to treatment. Initiation of low dose amitriptyline (525 mg nocte) at first diagnosis for 3 months reduces PHN rate by 50%. In established PHN (>12 months) treatment success is limited, but tricyclics, anticonvulsants, tramadol and opioids should be tried. Last updated February 2006 Page 7 of 7