Videostrobolaryngoscopy
advertisement

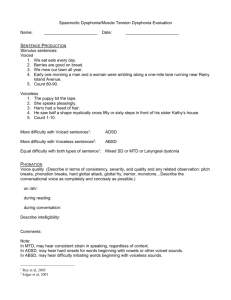
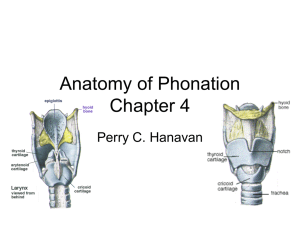
Laryngology Seminar Muscular Tension Dysphonia R3 陳佳弘 2002/05/08 INTRODUCTION muscular tension dysphonia (MTD) (Morrison & Rammage, 1983) other terms: vocal hyperfunction (Froeschels, 1952); vocal fatigue (Sander & Ripoich, 1983); hyperkinetic dysphonia; myasthenia larynges; laryngeal tension-fatigue syndrome (Koufman & Blalock, 1988) functional dysphonia (FD): absence of mucosal or neurogenic disease of the larynx; exclusion of organic disease; fluctuant course more than 40% of dysphonic p’ts have no identifiable organic or mucosal disease more than 50% of FD: due to vocal abuse or misuse ETIOLOGY & PATHOPHYSIOLOGY excessive or “imbalanced” activity of intrinsic and extrinsic muscles normal phonation: contraction of lateral cricoarytenoid (LCA) and interarytenoid mm.; relaxation of posterior cricoarytenoid (PCA) m. in MTD, contraction of LCA and interarytenoid mm.; without adequate relaxation of PCA m. compensated by tightening of thyroarytenoid m. apposition of vocal folds (VFs) convex reverse bowing of the glottic aperture + posterior glottic chink sources of excessive muscle activity: psychological, and/or personality factors; technical misuse + extraordinary voice demands; learned adaptation following URI; compensation of underlying disease phonotrauma: heat dispersing and shearing force during high-frequency vibration SYMPTOMATOLOGY neck or shoulder stiffness; excessive vocal effort, vocal fatigue, intensified with extended vocal use. EXAMINATION physical Examination focal palpation: 1) extent of laryngeal elevation, 2) focal tenderness or tender trigger points, 3) voice effect of applying downward pressure over the superior border of the thyroid lamina, 4) extent of sustained voice improvement following circumlaryngeal massage pressure 1) over the major horns of the hyoid bone, 2) over the superior cornu of the thyroid cartilage, and 3) along the anterior border of the SCM m. and 1 into the suprahyoid musculature, the posterior belly of the digastric m. Laryngoscopic features: plica ventricularis, anteroposterior compression, posterior glottic chink, and hard glottal attack Videostrobolaryngoscopy abnormal findings on the vocal folds (89.7%), especially during vibration uneven VF mucus surface (83%); vessel dilatation or neovascularization on the surface of vocal folds (53.8%), abnormal glottal closure (43.5%), and bilateral vibratory asymmetry(8.6%). multiple: 73.8% (Hsiao) Morrison-Rammage classification of MTD (1986) Sama A: laryngeal isometry (37%); lateral supraglottic pressure (60%) in the dysphonics; less frequent: glottic lateral contraction, incomplete adduction, and bowing 1) MR 1 (laryngeal isometric): generalized tension in all the laryngeal muscles; an open posterior chink due to persistent PCA m. pull during phonation. 2) MR 2 (lateral hypercontraction): lateral compression of larynx; tense-sounding voice; high laryngeal resistance forces; “vocal fatigue”; may be triggered by an infection or chronic reflux; “habituated hoarseness” (Koufman 1982); generalized postural misuse and tension subtype 2a: glottic contraction; subtype 2b: supraglottic adduction/squeezing, approximation of false VF during phonation; “plica ventricularis”; psychologically based 3) MR 3 (anterior-posterior supraglottic contraction): technical misuse; a petiole of epiglottis moved toward the arytenoids during phonation “Bogart-Bacall” syndrome: tension-fatigue dysphonia (Koufman 1982); reduced A-P diameter; compression dropped voice pitch 4) MR 4 (conversion dysphonia): psychological; generalized hypertonicity; highpitched, squeaky, or breathy, “la belle indifference”. VFs are away from the midline during phonation but function well for other types of vegetative phonation, e.g. cough, laughter. 5) MR 5 (psychological dysphonia with bowed VFs) excluding senile atrophy or sulcus vocalis; “habituated hoarseness” following a trigger. 6) MR 6 (adolescent transitional dysphonia) perpetuated falsetto; tension at the posterior glottis; high larynx; tight neck Van Lawrence Fibreoptic features of vocal hyperfunction (1987) 2 common features in the dysphonics: harsh approximation of arytenoids, decreased vocal length visibility, excessive vertical movement, and anteroposterior compression (40-50%). vestibular fold and lateral compression: less (25–40%). the prevalence of Van Lawrence features in control subjects: similarly high. In the nondysphonics (Sama A et al) features of hyperfunction: also prevalent in the nondysphonics; cannot distinguish between patients with FD 60% of the nondysphonics demonstrate one or more of the features classically associated with FD 50% of the control population did demonstrate abnormal vocal technique Koufman’s diagnostic criteria for six types of functional voice disorders Electromyography (EMG) 3 Stemple (1980): biofeedback Milutinovic (1988): 2-4-fold increase of EMG activity (7/11) Hocevar-Boltezar (1998): 6-8-fold increase of EMG activity and/or an alternation of the EMG activity level in the perioral (upper lip; m. orbicularis oris)& supralaryngeal (m. thyrohyoideus, m. omohyoideus, m. sternohyoideus, platysma) muscles before and during phonation (7/11); excessive tension of both the internal and external laryngeal mm. TREATMENT Topical lidocaine injection 3 cc of 4% lidocaine using 25-gauge needle (Dworkin) abrupt cough reactions; a sensation of laryngeal/ tracheal numbness; slight difficulty with dry swallows persistently high-pitched shrill vocal quality was converted to near normal voice patterns within 15 mins after transcricothyroid membrane injection break the perverse cycle of hyperactive glottal and supraglottal muscle contractions sensorimotor mechanism of action Manual laryngeal tension reduction in diagnosis and management (Roy) A. Medial suprahyoid musculature is palpated at rest and during upward pitch glide maneuvers. Focal sites of tenderness and taut bands signal excessive muscle activity B. Signs of excess laryngeal tension are assayed by 1) evaluating presence of focal sites of pain or nodularity, 2) determining size of thyrohyoid space, and 3) observing voice effect of downward traction over superior border of thyroid lamina and during circumlaryngeal massage C. Larynx is compressed by exerting anterior-to-posterior pressure over inferior border of hyoid bone D. Manual tension reduction procedure (circurmlaryngeal massage) with hand configuration and placement. Pressure is applied in circular motion over tips of hyoid bone and within thyrohyoid space. Procedure is repeated over posterior borders of thyroid cartilage and larynx is gently pulled downward. 4 Voice therapy effective in 69% of the p’ts failure: continued tobacco use, noncompliance, premature termination of therapy 1) progressive relaxation: (Jacobson, 1938) alternatively tensing and relaxing all the muscles from the scalp to the toes 2) chewing exercise (Froeschels, 1952) ask p’ts to image they are chewing food (Wilson) 3) yawn-sigh approach (Boone) a. eliminate abusive vocal initiations and to reduce tension of the larynx. b. “yawn”: expand the pharynx and stretch extrinsic laryngeal muscles lowering the larynx position, forward placement of the tongue a slight opening between the vocal folds, and dilated pharynx c. “sigh”: produce a sustained inhalation. d. maximum power transfer theorem: the vocal tract input impedance was calculated [Sondhi and Schroeter (1987), Titze and Story (1997)] a wide epilarynx tube (laryngeal vestibule) matches well with low glottal resistance e. f. g. provide relief from laryngeal tension--> appreciate the sensation of laryngeal relaxation replace the sigh with words beginning with /h/ such as "hi", "hey", "home", "happy". produce phrases/sentences following the yawn, "Hi, how are you?", "He has hairy hands!" 4) biofeedback training: Stemple (1980) EMG biofeedback permitting p’ts to monitor the electric activities of their muscle & to exert some control. Other treatment modalities 1) role of microsurgery for hypertrophy of the ventricular folds: three stages (Kosokovic, 1973) stage I: reversible histological changes: and quick success in V/T stage II: reversible histological changes; prolonged and persistent V/T stage III: irreversible histological changes (connective hyperplasia) 2) laser therapy of dysphonia plica ventricularis: carbon dioxide laser for excision of the hypertrophied false VFs 3) botulinum toxin injection into the false vocal folds followed by speech therapy (Kendall 1997) 5 REFERENCE 1. Sama A, Carding PN, Price S, Kelly P, Wilson JA. The clinical features of functional dysphonia. Laryngoscope. 2001 Mar;111(3):458-63. 2. Hsiao TY, Liu CM, Hsu CJ, Lee SY, Lin KN. Vocal fold abnormalities in laryngeal tension-fatigue syndrome. J Formos Med Assoc. 2001 Dec;100(12):83740. 3. Roy N, Ford CN, Bless DM. Muscle tension dysphonia and spasmodic dysphonia: the role of manual laryngeal tension reduction in diagnosis and management. Ann Otol Rhinol Laryngol. 1996 Nov;105(11):851-6. 4. Titze IR. Regulating glottal airflow in phonation: application of the maximum power transfer theorem to a low dimensional phonation model. J Acoust Soc Am. 2002 Jan;111(1 Pt 1):367-76. 5. Hocevar-Boltezar I, Janko M, Zargi M. Role of surface EMG in diagnostics and treatment of muscle tension dysphonia. Acta Otolaryngol. 1998 Sep;118(5):73943. 6. Dworkin JP, Meleca RJ, Simpson ML, Garfield I. Use of topical lidocaine in the treatment of muscle tension dysphonia. J Voice. 2000 Dec;14(4):567-74. 7. Morrison MD, Rammage LA. Muscle misuse voice disorders: description and classification. Acta Otolaryngol. 1993 May;113(3):428-34. 8. Morrison MD, Nichol H, Rammage LA. Diagnostic criteria in functional dysphonia. Laryngoscope. 1986 Jan;96(1):1-8. 9. Koufman JA, Blalock PD. Functional voice disorders. Otolaryngol Clin North Am. 1991 Oct;24(5):1059-73. 10. Koufman JA, Blalock PD. Classification and approach to patients with functional voice disorders. Ann Otol Rhinol Laryngol. 1982 Jul-Aug;91(4 Pt 1):372-7. 11. Hillman RE, Holmberg EB, Perkell JS, Walsh M, Vaughan C. Objective assessment of vocal hyperfunction: an experimental framework and initial results. J Speech Hear Res. 1989 Jun;32(2):373-92. 12. Stemple JC, Weiler E, Whitehead W, Komray R. Electromyographic biofeedback training with patients exhibiting a hyperfunctional voice disorder. Laryngoscope. 1980 Mar;90(3):471-6. 13. Sapienza CM, Walton S, Murry T. Adductor spasmodic dysphonia and muscular tension dysphonia: acoustic analysis of sustained phonation and reading. J Voice. 2000 Dec;14(4):502-20. 14. Story BH, Titze IR, Hoffman EA. The relationship of vocal tract shape to three voice qualities. J Acoust Soc Am. 2001 Apr;109(4):1651-67. 15. Kendall KA, Leonard RJ. Treatment of ventricular dysphonia with botulinum toxin. Laryngoscope 1997 Jul;107(7):948-53. 6