Case 3
advertisement

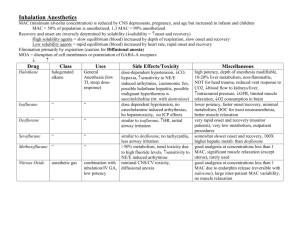
1 Chapter 16: General Anesthetics Case Study 3 MD is a 45-year-old white female who will be undergoing a lumpectomy to remove a malignancy in her right breast. MD has a history of reconstructive knee surgeries, which have left her with one kidney as a result of the large doses of cephalosporins she was administered to control postoperative infections. The surgeon and the anesthesiologist want to use a rapid onset/recovery general anesthetic with a minimum risk for nephrotoxicity. Recommend one of the following structures . 1. Identify the therapeutic problem(s) for which the pharmacist's intervention may benefit the patient. MD will have breast surgery and will undergo general anesthesia. No preinduction drugs 2 are needed and no skeletal muscle relaxants are required. The surgeon wants rapid onset/recovery general anesthesia with minimum nephrotoxicity. 2. Identify and prioritize the patient-specific factors that must be considered to achieve the desired therapeutic outcomes. MD is a middle-aged adult diagnosed with breast cancer. MD will undergo a lumpectomy requiring general anesthesia. MD has a history of reconstructive knee surgery. MD has only one kidney, the result of antibiotic therapy for postsurgical infections. A general anesthetic with minimal nephrotoxicity is required. 3. Conduct a thorough and mechanistically oriented structure–activity analysis of all therapeutic alternatives provided in the case. Structure 1 is a halogenated methyl ethyl ether. It has a blood gas partition coefficient of 1.4 and a minimum effective alveolar concentration (MAC) of 1.15. It has a rapid onset/recovery owing to its intermediate blood solubility. Structure 1 has a pungent odor and can cause coughing and laryngospasm during administration. Less than 0.2% of the administered dose is metabolized. The products of metabolism are fluoride ion and 3 trifluoroacetic acid. Fluoride ion is associated with nephrotoxicity. Structure 2 is also a halogenated methyl ethyl ether and can be considered an analog of structure 1. It has a blood gas partition coefficient of 12 and a MAC of 0.16. Therefore, it has a high solubility in blood, giving it a slow onset/recovery. Its MAC is the lowest of the halogenated anesthetics, making it the most potent. About 50% of the administered dose is metabolized, characterized by having the highest rate of fluoride ion production; hence, the greatest risk for nephrotoxicity. Structure 3 is also a halogenated methyl ethyl ether and has a blood gas partition coefficient of 0.42 and a MAC of 6.0. Its low solubility in blood gives it a rapid onset/recovery. Recovery from the anesthesia is about twice as fast as with structure 1. It has a low rate of metabolism with the generation of trifluoroacetic acid accounting for < 0.02% of the administered dose. It has the least likelihood of being hepatotoxic and nephrotoxic. Structure 4 is a halogenated methyl isopropyl ether. It has a blood gas partition coefficient of 0.60 and a MAC of 1.71. It has low blood solubility and a relatively high potency. Its advantage is that it is not irritating to the respiratory tract. It has a rapid onset/recovery and is metabolized to fluoride ion with an overall metabolism rate of 3%. 4. Evaluate the SAR findings against the patient-specific factors and desired therapeutic outcomes and make a therapeutic decision. Structure 2 (methoxyflurane) would be the least likely anesthetic to be used in this case. Its slow onset and recovery and its high rate of metabolism to toxic products make it well 4 known as a hepatotoxic and nephrotoxic agent. Isoflurane (structure 1), desflurane (structure 3), and sevoflurane (structure 4) are all viable candidates for the general anesthetic in this case. They all have the requisite rapid onset/recovery with low incidence of nephrotoxicity. Of the three, however, desflurane would be the best because it has the lowest metabolism to fluoride ion, though it is the least potent of the selections (MAC of 6.0). 5. Counsel your patient. Tell MD to divulge all medications to her physicians, especially if she is taking herbals because of possible herb–anesthetic interactions. Although there is no direct clinical evidence, it is possible that sedative herbs could enhance the effects of general anesthesia. These include such popular herbs as St. John's wort, valerian, kava, California poppy, Siberian ginseng, goldenseal, calamus, Jamaican dogwood, German chamomile, and catnip. MD will be groggy and may experience slight nausea, vomiting, and some postoperative chills. MD will also most likely be prescribed pain medication to help her through the healing process.