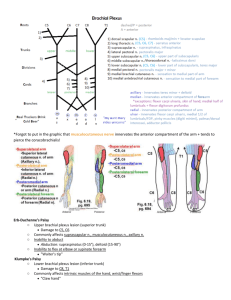
Blue Box Stuff From Moore

Blue Box Stuff From Moore
“Mmmhh hhehehhmm mmhehhmm … yeah, he said, ‘Butt.’”
– attributed to the great philosopher Butthead.
Blood Vessel Stuff
The femoral artery . This supplies most of the blood to the lower limb. Its first branch is the profunda femoris , found lateral to the femoral artery between the pectineus and adductor longus, supplying the adductor magnus and hamstrings. It also gives off the medial and lateral femoral circumflex arteries , which supply blood to the head and neck of the femur and may be dmged when the femur is fractured (more on this later). It runs posterior to the knee joint and as it leaves to popliteal fossa, branches into the anterior and posterior tibial arteries. The anterior tibial artery runs anterior to the interosseous membrane between the tibia and fibula, and continues in the foot as the dorsalis pedis artery . The posterior tibial then gives off a fibular branch. These two arteries run in the posterior compartment of the leg.
The posterior tibial continues on into the foot as two branches, the medial plantar artery and the lateral plantar artery .
The Great Saphenous Vein runs anterior to the medial malleolus and up the medial portion of the leg and thigh. It drains the dorsum of the foot and medial half of the lower limb. It then enters the femoral vein at the saphenous opening just inferior to the middle of the inguinal ligament. It is mostly cutaneous. In the leg, it is accompanied by the saphenous nerve , which supplies cutaneous innervation to most of the anterior aspect of the leg.
The Small Saphenous Vein runs along the posterior aspect of the leg. It then pierces the deep popliteal fascia to enter the popliteal fossa (more on this later). It drains the lateral and medial aspects of the leg. It too is mostly cutaneous, and is accompanied by the medial sural nerve , which supplies cutaneous innervation to the posterior aspect of the leg.
Collateral Circulations . If the proximal portion of the femoral artery must be ligated, blood can still get to the rest of the lower limb by flowing through the inferior gluteal artery into an anastomosis with the circumflex arteries , which then flow into the profunda femoris and then the femoral artery, or distally to the genicular arteries of the knee to the rest of the limb. If the popliteal artery must be ligated, blood can flow around the ligation through these genicular arteries to the rest of the leg.
The lateral plantar artery and the deep plantar branch of the dorsalis pedis artery (which runs on the dorsum of the foot along the tendon of the extensor hallucis longus) make the deep plantar arch (arterial arch) .
Nerve Stuff
Stuff that leaves the greater and lesser sciatic foramina . The piriformis leaves through the greater sciatic foramen. The gemelli and obdurator internus leave through the lesser sciatic foramen. The superior gluteal neurovascular bundle leaves the pelvis superior to the piriformis. The inferior gluteal neurovascular bundle , along with the sciatic nerve , posterior femoral cutaneous nerve , pudendal , nerve to the obdurator , and nerve to the quadratus femoris all leave inferior to the piriformis. To avoid injuring the sciatic nerve, injections in the gluteal area should be given in the superolateral quadrant of the buttocks, just inferior to the iliac crest.
The Sciatic Nerve and branches . It usually enters the lower limb between the inferior border of the piriformis and the superior border of the superior gemellus. It then supplies motor innervation to the hamstring muscles, and just superior to the popliteal fossa , branches into the common fibular nerve going laterally and anteriorly and the tibial nerve continuing distally. The common fibular nerve goes anteriorly, over the head of the fibula, and splits into the superficial and deep divisions around this area. The common fibular nerve is the most commonly injured nerve in the lower limb. (See foot drop below).
Cutaneous innervation of the lower limb : as mentioned before, the saphenous nerve and medial sural nerve supply most of the leg. The lateral aspect of the leg is supplied by branches from the common fibular nerve.
The lateral aspect of the thigh is supplied by the lateral femoral cutaneous (blast from the past), while the posterior aspect is supplied by the posterior femoral cutaneous . To round this up, the anterior aspect of the thigh is serviced by branches from the femoral nerve , and the inner thigh by the obdurator nerve .
Gait Variations . Gluteal Gait – this occurs with denervation of the gluteus medius and minimus (Which nerve services these two wonderful muscles?). This is characterized by a falling of the pelvis towards the unaffected side at each step. It looks sorta waddly. Foot Drop – This is caused by injury to the common fibular nerve . Loss of eversion and dorsiflexion leads to a droopy foot. The patient has a high stepping gait with the foot raised higher than normal so the toes don’t hit the ground. The foot is brought down suddenly and clops on the floor. There may also be numbness on the anterolateral aspect of the leg and dorsum of the foot.
Stuff about the thigh
The thigh is enclosed by tough fascia called the fascia lata . It thickens along the medial edge into the iliotibial tract . The leg is enclosed by a continuation of this fascia called the crural fascia .
The femoral
. This is bounded laterally by the medial border of the sartorius , medially by the medial border of the adductor longus , superiorly by the inguinal ligament , and posteriorly by the pectineus and adductor longus muscles. This contains our ‘NAVEL’ – not the belly button, but the nerve, artery, blah, blah, you know the rest. The femoral artery, vein, and lymphatics are enclosed in the femoral sheath – the nerve is not. The mouth of the femoral sheath is called the femoral ring ; this is where femoral hernias extrude. Femoral hernias present as masses inferolateral to the pubic tubercle and medial to the femoral vein. The saphenous nerve runs in the triangle, then becomes superficial just superior to the medial condyle of the tibia.
The adductor magnus has both an adductor portion (innervated by the obdurator nerve) and a hamstring portion
(innervated by the tibial branch of the sciatic). A similarly versatile muscle is the biceps femoris , whose long head / hamstring portion is innervated by the tibial branch of the sciatic and short head / leg flexor portion is innervated by the common fibular portion of the sciatic.
Stuffed Knees
The Popliteal Fossa . This is bounded superolaterally by the biceps femoris , superomedially by the semitendinosus and semimembranosus , inferolaterally and inferomedially by the two heads of the gastrocnemius . The fossa contains the popliteal artery medially , the saphenous nerve laterally and the popliteal vein in between. The small saphenous vein feeds into the popliteal vein in this fossa. The popliteal artery gives off a number of genicular branches , which supply the knee joint.
If the knee is hit from the lateral side while it is locked, this can be bad news. Remember the three C’s , as these are the three structures that are injured: collateral ligament of the tibia , anterior cruciate ligament , and cartilage of the medial meniscus . If the tibia is forced posteriorly when the knee is flexed, as in sudden deceleration of a car accident, damage to the posterior cruciate ligament can occur. When either of these ligaments are ruptured / torn, it is near impossible to put weight on the injured knee.
The anterior cruciate ligament (ACL) goes from the anterior part of the intercondylar area of the tibia, superiorly, posteriorly, and laterally to the medial side of the lateral condyle of the femur. It prevents posterior displacement of the femur on the tibia and hyperextension of the knee joint . If one’s ACL is torn, then the tibia can move anteriorly when the leg is extended (ewww…).
The posterior cruciate ligament (PCL) goes from the posterior part of the intercondylar area of the tibia, superiorly, anteriorly, and medially to the lateral side of the medial condyle of the femur. It prevents anterior displacement of the femur on the tibia and stabilizes the femur, esp. when descending stairs or walking downhill . If one’s PCL is torn, the tibia can move posteriorly when the leg is flexed (also ewww…).
Stuff about the leg
Leg compartments: Anterior, Lateral, and Posterior. The anterior compartment contains (M to L) the tibialis anterior , extensor hallucis longus, and extensor digitorum longus , as well as the deep fibular nerve and anterior tibial vessels . The lateral compartment contains the fibularis longus and brevis , as well as the superficial fibular nerve . The posterior compartment is separated into deep and superficial portions. The superficial portion contains the soleus and gastroc . The deep portion contains (M to L) the flexor digitorum longus , tibialis posterior , and flexor hallucis longus , in addition to the posterior tibial and fibular vessels and the tibial nerve.
Foot stuffing
The superior extensor retinaculum is a thickening of the crural fascia on the junction between leg and foot, superior to the malleoli. The inferior extensor retinaculum is a V-shaped thickening of fascia anterior and inferior to the malleoli. These two retinacula bind the tendons of the extensor digitorum longus laterally and the extensor hallucis longus and tibialis anterior medially.
The flexor retinaculum is located posteroinferiorly to the medial malleolus and confines the tendons of the muscles of the posterior compartment. The fibular retinaculum is located inferior to the lateral malleolus and confines the tendons of the muscles of the lateral compartment.
Ligaments of the foot . The deltoid ligament attaches the medial malleolus to the tarsal bones. This ligament resists foot eversion and is so strong that when the foot is hypereverted (rolling an ankle), the medial malleolus will actually fracture when the ligament pulls it off of the tibia. The ankle is unstable during plantarflexion, and is liable to hypereversion. This may result in Pott’s fracture , where the medial malleolus fractures as per above, and the fibula breaks superior to the lateral malleolus .
The lateral ligaments attach the lateral malleolus to the talus and calcaneus. These ligaments tear / rupture when the foot is hyperinverted . Severe hyperinversion may result in fracture of the medial malleolus , avulsion of the tuberosity of the pinky metatarsal , and rupture of the joint cavity encapsulating the ankle joint .
The foot has two arches, the longitudinal arch along the AP axis and the transverse arch along the ML axis. The longitudinal arch is maintained by the plantar calcaneonavicular (spring) ligament medially and the long plantar ligament laterally. The are bridged and supported by the plantar aponeurosis of the foot. The transverse arch is maintained by the tendon of the fibularis longus , enters the foot laterally and wraps around the sole of the foot medially to attach at the tuberosity of the fifth metatarsal.
Just stuff
Fractures of the neck of the femur may damage the circumflex femoral arteries , cut off blood supply to the head and neck of the femur, resulting in tissue necrosis (Bo Jackson, sportsfans?). This injury commonly occurs in elderly individuals with osteoporosis. Patients with broken femoral necks will present with the injured limb abducted and laterally rotated . Owing to contraction of the quadriceps, the injured limb may also appear to be shorter than the other limb. The sciatic nerve may be injured / compressed in such an injury, paralyzing the hamstrings and the muscles further south er … distal.
This injury is in contrast to a truly dislocated femur, which can occur in automobile accidents with the head of the femur forced posteriorly by the force of impact. Patients will present with injured limb adducted and medially rotated , and shorter than the other limb.
Stuff not associated with the lower limb but you’ll still find interesting
CN IV and V
I
do not enter the orbit through the anulus tendineus of the eye. CN II, III and VI do, as well as the opthalmic artery.
CN III and IV may be compressed by aneurysms around the posterior cerebral and superior cerebellar arteries.
(Look at a picture of the Circle of Willis that has a brain, too – Clemente Plate 493 or Moore 698). CN VI may be compressed by aneurysms around the anterior inferior cerebellar and the labyrinthine arteries.
CN XII and the lingual artery make a yummy sandwich of the hyoglossus. (Puts new meaning to ‘tongue sandwich,’ hardy har …). The nerve is lateral to the hyoglossus while the artery is medial to the muscle. All these are deep to the mylohyoid, so I guess we have ourselves a double-decker.
Lesions of CN VII may paralyze the stapedius muscle and destroy attenuation of loud sounds.
No more cranial nerves, argh! On to the pharynx – there are four gaps in the pharyngeal constrictors. Here’s what enters those gaps. (1) Where the superior constrictor attaches to the skull ~ levator veli palatini , auditory tube , ascending palatine artery (branch off the lingual a.). The retropharyngeal recess begins here. (2) Inferior to the superior constrictor and superior to the middle constrictor ~ stylopharyngeus , CN IX , stylohyoid ligament . (3)
Inferior to the middle constrictor and superior to the inferior constrictor ~ internal laryngeal nerve and superior laryngeal artery / vein . (4) Inferior to the inferior constrictor ~ recurrent laryngeal nerve and inferior laryngeal artery
The glottis is most responsible for phonation
If the external laryngeal nerve is damaged, the cricothyroids cannot tense the vocal ligament. As a result, the voice
‘tires easily’ and becomes hoarse after extended use.
Hey everyone, kick ass … er gluteal region on this final! Good luck to all, and happy holidays
Ray