Popliteal_Fossa_Block_Info
advertisement

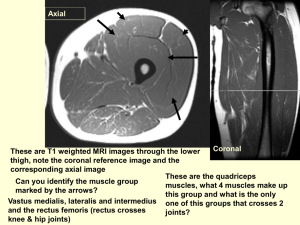
POPLITEAL FOSSA BLOCK INDICATIONS: Surgical procedures below the knee Foot/ankle surgery Achilles tendon surgery Sural nerve biopsy Short saphenous vein stripping DRUGS: CHLOROPROCAINE (NESACAINE) 2% for peripheral nerve block, maximum dose 800mg or 1000mg with epinephrine. Duration is < or equal to 1 hour plain or up to 1.5 hours with epinephrine. MEPIVICAINE (CARBOCAINE, POLOCAINE) 1-1.5% for peripheral nerve block, maximum dosage 400mg plain, 500mg with epinephrine. Duration is 1-4 hours plain, with epinephrine 2-5 hours. ROPIVACAINE (NAROPIN) 0.5-1% for peripheral nerve block, maximum dosage 250mg. Duration 2-8 hours LIDOCAINE (XYLOCAINE) 1-1.5% for peripheral nerve block, maximum dosage 300mg plain, 500mg with epinephrine. Duration is 1-1.5 hours plain, and 2-3 hours with epinephrine All agents expected to onset within 15-20 minutes. ADJUNCTIVE AGENTS: SODIUM BICARBONATE Increases the pH, creating a more lipid soluble solution. Less ionization results in increased speed across the cell membrane, producing a faster onset of action. VASOCONSRICTORS INCLUDING EPINEPHRINE, PHENYLEPHRINE OR NOREPINEPHRINE. Vasoconstriction at the site, decreases absorption, thereby increasing neuronal uptake and prolonging the duration of action and limiting toxic side effects. ANATOMY: NERVES: Sciatic nerve divides into the tibial and common peroneal nerves 7-10cm above the crease of the knee in the popliteal fossa. The tibial nerve is larger and runs parallel and slightly lateral to midline of the leg. The tibial nerve continues deep behind the gastrocnemius muscle and exits the popliteal fossa. The common peroneal nerve follows the tendons of the biceps femoris laterally and travels around the fibular head as it leaves the fossa. Common peroneal and tibial nerves innervate the entire leg below the knee, EXCEPT the antero-medial leg and foot which are innervated by the saphenous nerve (L2-L4). Depending on the location of the surgery being performed, a saphenous nerve block may be needed for adequate analgesia of the affected limb. MUSCLES: Posterior anatomy: the upper popliteal fossa is bound laterally by the biceps femoris tendon and medially by the semitendinosus and semimembranous tendons. Lateral anatomy: Biceps femoris and vastus lateralis muscles are identified by finding the lateral femoral epicondyle, which is easily palpated as a bony prominence on the lateral aspect of the knee joint. ARTERIES AND VEINS: The popliteal artery is lateral to the semitendinosus tendon and just above the crease of the knee. The popliteal vein is lateral to the artery. The tibial and common peroneal nerves are within a sheath and are just lateral to the vein and medial to the biceps tendon 4-6cm deep in the skin. TECHNIQUE: The popliteal block is achieved by injecting local into the popliteal fossa where the common peroneal and tibial nerves lie. There are two approaches, intertendinous and lateral. INTERTENDINOUS APPROACH: Have pt. assume prone position with feet off the edge of the bed to ease twitch identification. Pt. may flex knee joint to ease landmark identification. Three landmarks are identified and marked with pen: (1)popliteal crease, (2)tendons of biceps femoris (lateral) and (3)semitendinosus (medial). Insertion point is located and marked 7cm proximal to popliteal crease at the midpoint between each identified tendon. Prepare area using sterile technique. Using a 22 guage stimplex needle with nerve stimulator, the needle is inserted perpendicular to the skin with initial current of 1.5 mA. Advance anteriorly until desired nerve is stimulated. Stimulation of tibial nerve results in plantar flexion and inversion. Stimulation of common peroneal nerve results in dorsiflexion and eversion. If the nerve is not localized on the first needle pass, the needle is withdrawn back to the skin and re-directed laterally. When this maneuver fails, the needle is taken out and repositioned 1cm lateral to the original puncture site and the entire process is repeated. When stimulation response is localized, the output current of the nerve stimulator is then gradually adjusted to the lowest current at which these responses are still obtained (goal is less than 0.4mA). When the stimulation is obtained at current intensities of less than 0.2mA, the needle should be slightly withdrawn. Stimulation at such a small current intensity may indicate an intraneural placement of the needle. After appropriate stimulation at desired current level and aspiration of needle to ensure non-intravascular placement, injection of 30-40cc’s of local anesthetic may be injected for block. LATERAL APPROACH: This technique is utilized if patient’s are unable to turn prone, i.e. advanced pregnancy, morbid obesity, spine and hemodynamic instability, or mechanical ventilation. Start with pt. in supine position, and approach from lateral knee. Identify landmarks: Biceps femoris and vastus lateralis muscles are identified by finding the lateral femoral epicondyle. Locate groove between biceps femoris and vastus lateralis. Insertion point is located 7cm proximal from lateral femoral condyle within the groove of the biceps femoris and vastus lateralis muscles. Mark structures with pen. Insert needle perpendicular to skin in horizontal plane, with initial current of 0.8mA at 7cm mark. Advance until desired contact with femur. If no bony contact made with femur, re-insert needle 5-10mm anterior to mark. Upon bony contact with femur, redirect needle at 30 degrees posterior angle until nerve stimulation. Stimulation of tibial nerve results in plantar flexion and inversion. Stimulation of common peroneal results in dorsiflexion and eversion. When the nerve is not localized on the first angled needle pass, the needle is withdrawn back to the skin and re-directed anteriorly or posteriorly at a 5-10 degree change in angle. If no further response, withdraw needle and re-insert 5mm more posteriorly. When appropriate stimulation is identified, aspirate to ensure nonintravascular placement, then inject 30-40cc’s of local anesthetic. ASSESSMENT OF BLOCK EFFICACY: Ask pt. to move toes and ankle: motor. Lightly pinch foot and leg to assess analgesia: sensory to pain. If pt. responds, may have missed saphenous nerve. Convert to general. SPECIFIC COMPLICATIONS: Nerve damage from direct injection of LA into nerve. S/S include severe pain on attempted injection or marked resistance to injection. Intraneural injection less likely if using short beveled needle. Paresthesia is the “electric shock-like” feeling felt as the nerve is touched by the needle. Do not advance needle further as nerve damage is likely to occur. Intravascular injection. Monitor for systemic toxicities including confusion, metallic taste, tinnitus or seizures. Remember saphenous nerve usually also needs blocked. STUDY QUESTIONS: 1. What kind of surgical procedures is this block used for? 2. Why would a current intensity of less than 0.2mA be a concern? 3. Stimulation of the tibial nerve elicits what response? 4. Stimulation of the common peroneal nerve elicts what response? 5. What nerve might require a separate block if the antero-medial leg and foot are not sufficiently blocked? ANSWERS: 1. foot and ankle surgery, achilles tendon surgery, sural nerve biopsy, or short saphenous vein stripping 2. intraneuronal placement of needle 3. plantar flexion and inversion 4. dorsiflexion and eversion 5. saphenous nerve block Barash, P., Cullen, B., Stoelting, R. (2001).Clinical Anesthesia. Lippincott Williams & Wilkins. Morgan, E., Mikhail, M., Murray, M. (2002). Clinical Anesthesiology. (3rd ed.) Lange Medical Books. www.nysora.com Hadzic A, Vloka JD. A comparison of the posterior versus lateral approaches to the block of the sciatic nerve in the popliteal fossa. Anesthesiology 1998;88:1480-6 Vloka JD, Hadzic A, April E, Thys DM. The division of the sciatic nerve in the popliteal fossa: anatomical implications for popliteal nerve blockade. Anesthesia & Analgesia 2001;92:215-7