Preoperative Physical Status Evaluation: Variability
advertisement

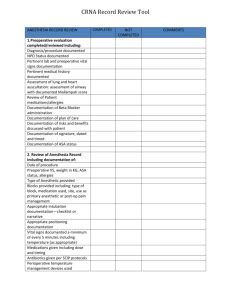
1 ABSTRACT: Introduction: The ASA PS Classification System is widely used to assess patients preoperatively. Objective: To assess inter-rater consistency of PS determination between surgical and anesthesiologist residents, to find sources of variability, to evaluate the effect of an interdepartmental re-orientation meeting, and to determine effects of discordance on patient outcome. Methods: A case series of all inpatient operations under anesthesia other than local in 2004. An interdepartmental meeting on was held towards the end of the 3rd month of the 9month duration of the study. Results: Of 1590 cases, almost all of the 62 percent discordance was where a higher PS class was assigned by the anesthesiologist-in-charge. After the conference, discordance rate decreased from 71 to 57 percent. Neither emergent/elective classification of operations nor years of practicing of the residents-in-charge showed correlation with discordance rates. Despite the disconcordance, there was no significant effect on mortality and morbidity. A gradual deterioration back towards pre-conference discordance rates suggests the need for regular orientations. Future research is recommended to determine the significance of the documented variability in terms of preoperative laboratory usage. Keywords: ASA PS, physical status, functional status, preoperative evaluation 2 Introduction: The American Society of Anesthesiologists (ASA) Physical Status (PS) Classification Scale is used by anesthesiologists and recognized by surgeons globally 1,2,3 as a most practical way to assess the preoperative PS of patients. It has at least equal prognostic significance as other preoperative classification systems.2 In 2001, when the Departments of Surgery and Anesthesiology of Hospital X decided to do away with routine cardiopulmonary, endocrine, and pediatric clearances prior to operations, they mutually agreed that aside from the selective use of preoperative screening examinations, the physical status of the patients should be routinely assessed using ASA PS classification. They would use the PS categorization to facilitate discussion, problem solving and decision making during the preoperative, postoperative, and mortality and morbidity conferences. Specifically, the PS categorization would be used to assess the preoperative risk, to identify patients who might need more attention and preoperative preparations, to facilitate analysis and understanding of complications, as well as to facilitate in quality service review. From 2001 to this writing, September, 2004, the PS categorization of all preoperative patients of the Department of Surgery was being done by both surgical and anesthesiologist residents. During the weekly Surgery-Anesthesiology Conferences, questions would be raised by both 3 consultants and residents of the two departments on the accuracy and discrepancy of the posted PS categorizations. In March 2004, because of the persistent questionings on the reliability of interpretations of PS between surgeons and anesthesiologists, it was decided to formally conduct a study. In late March, 2004 a joint Surgery-Anesthesiology Conference re-oriented all residents on the ASA PS Classification Scale with some agreements on how to deal with commonly encountered issues such as age, previously controlled medical conditions, tuberculosis, etc. It was also decided to make a study on the extent of variability. The objectives of this study were to assess inter-rater consistency of preoperative physical status determination between surgeons and anesthesiologists in a tertiary hospital in the Philippines; to find possible sources of this variability; to evaluate the effect of a Surgery-Anesthesia interdepartmental meeting on these discordance rates; and to determine if poor patient outcome was associated with a higher discordance. Methods: This is a case series of all patients who underwent inpatient operations under anesthesia other than local at Hospital X, a tertiary city government hospital in the Philippines between January 2004 and September 2004. 4 A Surgery-Anesthesia interdepartmental meeting on ASA PS classification held at the last week of March aimed to reorient the residents and improve discordance rates. Results: Of the 1680 operative records during the 9 months covered by the study, 1590 (87 percent) had documentation of PS status by both surgeons and anesthesiologists. Inter-observer PS assigned was more often than not (62 percent) different between the two physicians (anesthesiologist-in-charge, and surgeon-in-charge) most directly involved with the patient. Almost all of the discordance was where anesthesia assigned the patient to a higher PS status, 3 percent of which was by two levels. Less than one percent was assigned higher PS by the surgeon. A Surgery-Anesthesia interdepartmental meeting on ASA PS classification led to the Department of Anesthesia initiating their mandatory use of a formal preoperative evaluation form. A pre-conference discordance rate of 71% (365/515) improved to 57% (552/974). 5 Monthly variability was graphically illustrated according to elective/ emergency nature (figure 1) of the operations and according to year level of training of the involved resident (figures 2 and 3). Of the 61 mortalities and 47 morbidities reported during the duration of the study, anesthesia other than local were used on 40 postoperative mortalities and 41 perioperative morbidities. 92 and 93 percent of these had PS data from both Anesthesia and Surgery. The discordance rates were 62 and 68 respectively, compared with the overall average discordance rate of 62%. Discussion: Preoperative risk assessment of patients aims to minimize postoperative complications and adverse outcomes. A complete clinical risk assessment should include not only history and physical examination but also a complete review of systems, medication history, and functional status evaluation. The general public agrees 4 with physicians that such forms an important part of preparations prior to surgery. There is however no standard scoring system or definite way of determining which signs, symptoms, or laboratory examinations hold greater weight. The ASA PS Classification System, is one of the most popular 1,2,3 system being utilized by surgeons and anesthesiologists. It gives a global assessment of risk in contrast with specific organ-system risk scales. Inter-rater agreement between surgeons and anesthesiologists, and even among 6 anesthesiologists themselves 5,6,7 however varies tremendously, as was observed in our institution. The high overall discordance rate of 62% during the period covered by this study suggests a need to improve the scoring system or the system of its application. It can be seen that ASA used open-ended criteria such as mild, some, moderate, severe, moribund, and may be a reason for the continuing discrepancy. PS Systemic disease AND Functional limitation 1 Normal 2 Mild to moderate None 3 Severe Some 4 Life-threatening ± sx Incapacitated 5 Moribund (sx last resort) 6 Brain dead donor The emergent or elective classification of the operations had no effect on the discrepancy rate. Years of practicing (3-year anesthesia training program, 5year surgery training program) also did not show a correlation with scoring. After the conference, the resulting improvement of inter-observer consistency from 29 to 43 percent (and above 50 in the immediate postconference period) suggests the need for orienting surgical and anesthesia 7 residents to the system of classification. The gradual deterioration back towards pre-conference values suggests a need to do orientation activities regularly, perhaps once or twice a year. First year surgical residents showed a tendency to forget the orientation quickly. Previous local data 8 shows ASA class II patients having a higher risk than those described in other countries. Since much of the increase/ discordance in this study was in class II patients, it is important to determine if the outcome varied. The PS discordance rates of the postoperative mortalities and perioperative morbidities were 62% and 68% respectively, showing no difference with the overall average discordance rate of 62%. Data completion remains a problem, with many charts not documenting PS classifications assigned in weekly audits. The Department of Anesthesia initiated a mandatory use of a formal preoperative evaluation form after the joint conference. Data does not show an effect on increasing concordance. Some foreign data suggest that introduction of a structured form for ASA might even lower data completion due to changes in routines and layouts.9 Patient education has limited the feasibility of a self-administered health status questionnaire reduce the need for prolonged physician evaluation time. Future research objectives include finding other possible sources of discordance; determining effects in subsequent ordering for laboratory 10 to 8 examinations and mandatory preoperative medical evaluation by internists/ cardiologists; and quantifying the impact of the differences in laboratory examinations. 9 REFERENCES: 1Aronson WL; McAuliffe MS; Miller K. Variability in the American Society of Anesthesiologists Physical Status Classification Scale. AANA J 2003; 71(4): 265-74. 2Junger A; Engel J; Quinzio L; Banzhaf A; Jost A; Hempelmann G. Risk predictors, scoring systems and prognostic models in anesthesia and intensive care. Part I: anesthesia. Anasthesiol Intensivmed Notfallmed Schmerzther 2002; 37(9): 520-7. 3Meftahuzzaman AM; Rickta D; Sarker SC; MMC, Mymensingh. Grading & scoring systems used for pre-anaesthetic evaluation of the patients. Mymensingh Med J 2002; 11(1): 44-8. 4Matthey P; Finucane BT; Finegan BA. The attitude of the general public towards preoperative assessment and risks associated with general anesthesia. Can J Anaesth 2001; 48(4): 333-9. 5Haynes SR; Lawler PG. An assessment of the consistency of ASA physical status classification allocation. Anaesthesia 1995; 50(3): 195-9. 10 6Mak PH; Campbell RC; Irwin MG. The ASA Physical Status Classification: inter- observer consistency. American Society of Anesthesiologists. Anaesth Intensive Care 2002; 30(5): 633-40. 7Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology 1978; 49(4): 239-43. 8Samar-Sy OM; Bautista AH; Leachon AC; Dans AL; Tamesis BR. Preoperative predictors of complications among Filipinos undergoing non-cardiac surgery in a tertiary general hospital. Philipp J Intern Med. 1995; 33(5):163-176. 9Marco AP; Buchman D; Lancz C. Influence of form structure on the anesthesia preoperative evaluation. J Clin Anesth 2003; 15(6): 411-7. 10Reeves SW; Tielsch JM; Katz J; Bass EB; Schein OD. A self-administered health questionnaire for the preoperative risk stratification of patients undergoing cataract surgery. Am J Ophthalmol 2003; 135(5): 599-606. 11Pollard JB; Garnerin P. Outpatient preoperative evaluation clinic can lead to a rapid shift from inpatient to outpatient surgery: a retrospective review of perioperative setting and outcome. J Clin Anesth 1999; 11(1): 39-45. 11 Figure 1 Variability of Assigned Physical Status 90% Discordance Rate 80% 70% 60% 50% Elective OR Emergency OR 40% 30% 20% 10% 0% Jan Feb Mar Apr May 2004 Jun Jul Aug Sep 12 Figure 2 Discordance by Level of Surgical Training 90% Discordance Rate 80% 70% Residency 60% first year 50% second year 40% third year fourth year 30% fifth year 20% 10% 0% Jan Feb Mar Apr May 2004 Jun Jul Aug Sep 13 Figure 3 Discordance by Level of Anesthesia Training 1 0.9 Discordance Rate 0.8 0.7 Residency 0.6 first year 0.5 second year 0.4 third year 0.3 0.2 0.1 0 Jan Feb Mar Apr May 2004 Jun Jul Aug Sep