Chalenging-Patients
advertisement
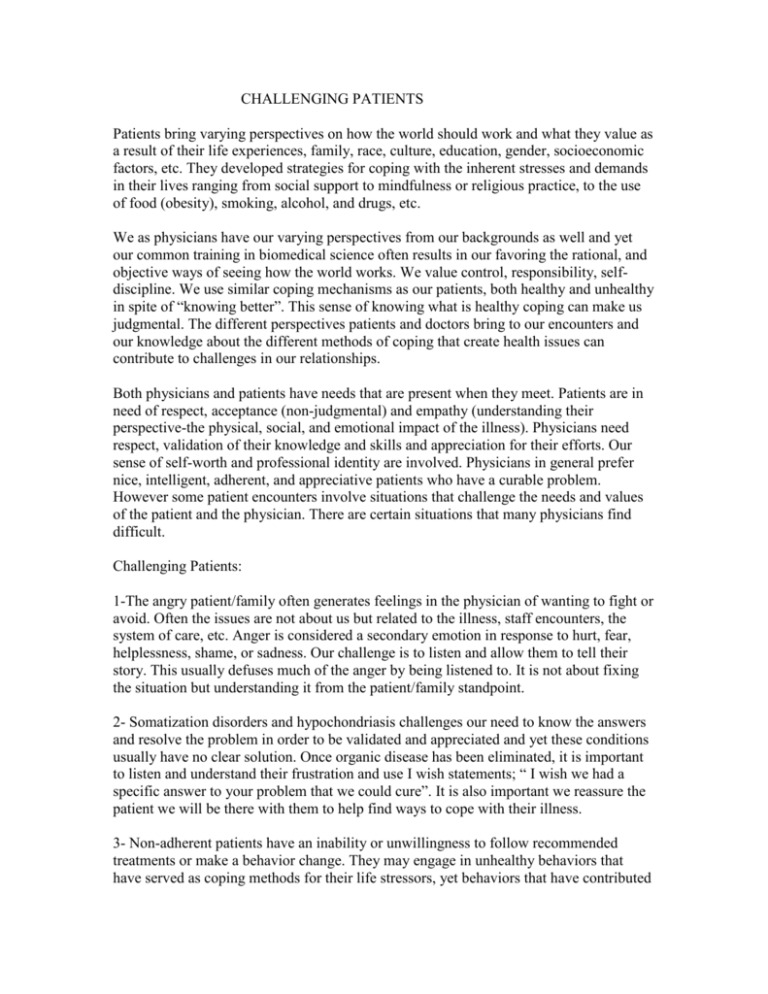
CHALLENGING PATIENTS Patients bring varying perspectives on how the world should work and what they value as a result of their life experiences, family, race, culture, education, gender, socioeconomic factors, etc. They developed strategies for coping with the inherent stresses and demands in their lives ranging from social support to mindfulness or religious practice, to the use of food (obesity), smoking, alcohol, and drugs, etc. We as physicians have our varying perspectives from our backgrounds as well and yet our common training in biomedical science often results in our favoring the rational, and objective ways of seeing how the world works. We value control, responsibility, selfdiscipline. We use similar coping mechanisms as our patients, both healthy and unhealthy in spite of “knowing better”. This sense of knowing what is healthy coping can make us judgmental. The different perspectives patients and doctors bring to our encounters and our knowledge about the different methods of coping that create health issues can contribute to challenges in our relationships. Both physicians and patients have needs that are present when they meet. Patients are in need of respect, acceptance (non-judgmental) and empathy (understanding their perspective-the physical, social, and emotional impact of the illness). Physicians need respect, validation of their knowledge and skills and appreciation for their efforts. Our sense of self-worth and professional identity are involved. Physicians in general prefer nice, intelligent, adherent, and appreciative patients who have a curable problem. However some patient encounters involve situations that challenge the needs and values of the patient and the physician. There are certain situations that many physicians find difficult. Challenging Patients: 1-The angry patient/family often generates feelings in the physician of wanting to fight or avoid. Often the issues are not about us but related to the illness, staff encounters, the system of care, etc. Anger is considered a secondary emotion in response to hurt, fear, helplessness, shame, or sadness. Our challenge is to listen and allow them to tell their story. This usually defuses much of the anger by being listened to. It is not about fixing the situation but understanding it from the patient/family standpoint. 2- Somatization disorders and hypochondriasis challenges our need to know the answers and resolve the problem in order to be validated and appreciated and yet these conditions usually have no clear solution. Once organic disease has been eliminated, it is important to listen and understand their frustration and use I wish statements; “ I wish we had a specific answer to your problem that we could cure”. It is also important we reassure the patient we will be there with them to help find ways to cope with their illness. 3- Non-adherent patients have an inability or unwillingness to follow recommended treatments or make a behavior change. They may engage in unhealthy behaviors that have served as coping methods for their life stressors, yet behaviors that have contributed to their disease. It can be easy to be judgmental here. Our challenge is to use our motivational interviewing skills and let go of attachment to our outcome. We need to realize their failure to change is not our failure. 4-“Hotbuttons”are those issues that involve our values and beliefs that we feel are important. When others fail to follow these same values and beliefs, our biases, judgments, criticisms arise. Commonly these involve patients who we judge as having lack of self-discipline, are irresponsible, slothful, or acting irrational. Are we able to accepting of our patients as doing the best they can base on their perspectives. 5- Patients in pain where physicians are concerned about drug seeking behavior is a special situation and requires boundary setting, negotiating a medication plan and careful follow-up. Guide to Success: 1-Our first step is our self-awareness of our emotions, which arise in these challenging situations. If we are feeling uncomfortable in a patient encounter, this is our clue to an emotional barrier and we need to explore it. Emotions are said to be “contagious” and anxious, angry or depressed patients will often contribute to our having similar feelings or triggering our own biases. Questions/Statements to consider: You seem upset. Help me understand. What worries you the most about this? How is this affecting your life? How do you think I can help you? 2- If we are mindful, we can create “space” around our emotions so we can choose the best option for our patient and ourselves. In this way we avoid reacting out of our frustrations, which often arises when we feel we are unable to help, or our anger over conflicting values between the patient and ourselves. 3- Avoid giving information until the emotions (patients and our own) are explored using open-ended questions. Tell me more about the “worry”, “upset”, “concern”, “stress” etc and this exploration often leads us to the meaning of the illness (emotions point to meaning). Emotions arise when our needs and values are being affected, either supported as in joy, etc. or threatened as in fear, etc. Patients are usually unable to “hear” information until their emotions are addressed in some way. As physicians we will all face many challenging patient interactions. We need to be able recognize our emotions and avoid reacting in ways that are hurtful to our patient and ourselves. We can process them later in ways that help us gain self-understanding and dissipate the emotional energy. What needs and values of my own were involved in the interaction? Talking to a colleague, friend or journaling about the experience can be ways that help our understanding. The alternative is to “stuff it”, try to deny it and the result can be “numbing”ourselves. If this choice of coping is repeated over time, it may change who we are. Many examples of this numbing behavior are apparent on the wards at Duke. Michael Mcleod, MD References: 1-Elder, Nancy, MD MSPH , Ricer, Rick, MD , Tobias, Barbara, MD How Respected Family Physicians Manage Difficult Patients. JBFM, 2006 Vol 19 no 6 pg 533-541 2-William, Steiger, MD. Managing Difficult Patients. Psychosomatics, 1967 Vol 8 no 6 pg 305-308 3-Walling, Anne, MD; Montello, Martha, PHD; Moser, Scott, MD; Menikoff, Jerrry MD; Brink, Melanie, MA. Which Patients Are Most Challenging For Second Year Medical Students. Family Medicine, 2004 Vol: 36(10) pg 710-714 4-Adams, J MD; Murry, R MD. The General Approach To The Difficult Patient. Emergency Medicine Clin North Am 1998 Vol: 16 pg 689-700. 5-Baum, NH.Twelve Tips for Dealing with Difficult Patients. Geriatrics 2002 Vol 57 pg 55-57. 6- Grove, James, MD. Taking Care of The Hateful Patient. N.E.J.M. 1978 Vol 298 (16) pg 883-887.