Metabolic Bone Disorders - Austin Community College
advertisement

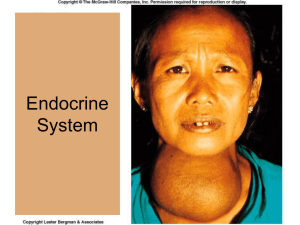
Endocrine Notes Anatomy & Physiology Review Endocrine System *Also very helpful view narrated PTT or as PODcast; also LEWIS Key points (audio/notes) A. B. C. D. E. F. G. A. Review only Endocrine system; (see text p.1201 ; Table 48-1; p. 1204 ; fig 48-8) 1. Consists of glands, specialized cells clusters and hormones-chemical transmitter secreted by glands in response to stimulation & CNS. 2. Regulates and integrates body’s metabolic activities; maintains homeostasis! Hormones & hormone function: chemical substances/messengers synthesized and secreted by a specific organs or tissue- exert action on specific cells called target cells 1. Common characteristics a. secreted in small amounts at variable but predictable rates (daily, hourly, monthly, etc) b. circulation through the blood c. Classified by chemical structure: lipid-soluble (all hormones produced by adrenal cortex, sex glands and thyroid hormones) and water-soluble (protein based) d. bind to specific cellular receptors in cell membrane or within cells e. inactivated or excreted by liver or kidneys f. alter rate of physiologic activities Hypothalamus: integrative center for endocrine and autonomic (involuntary nervous system) 1. Controls some endocrine glands by neural and hormonal pathways Negative feedback (negative feedback system) 1. Regulates endocrine system by inhibiting hormone overproduction 2. Can be simple or complex system a. Dysfunction can result from 1) Defects in gland 2) Release of trophic (hormones that control secretion of hormones by other glands) or effector hormones 3) Hormone transport 4) In target tissue such as adrenal cortex b. *Examples of negative feedback: low serum calcium have increased PTH; increased serum calcium, have decreased PTH Hormone to hormone regulation: dec. thyroid hormone (T3 & T4 > release of TRH by hypothalamus and TSH by anterior pituitary; inc. T3 and T4 levels inhibit TSH release (review thyroid and parathyroid). Hypothalamus and pituitary gland 1. Form a complex called the hypothalamic pituitary axis (HPA) 2. Integrates communication from nervous and endocrine systems 3. Examples, what hormone released under stress? Can this hormone make you fat? (p. 1276) (cortisol) (click here for more) and Stress and body fat. Endocrine disorders due to 1. Hypersecretion or hyposecretion of hormones 2. Hyporesponsiveness of hormone receptors 3. Inflammation of glands 4. Gland tumors a. Hypofunction or hyposecretion due to congenital defects, gland destruction, aging, atrophy b. Hyperfunction due to hyperplasia, tumors Components of the Endocrine System Components of the Endocrine System 1. Pituitary gland (hypophysis, master gland) a. Parts 1) anterior pituitary (adenohypophysis): composed of cells that secrete protein hormones 2) posterior pituitary (neurohypophysis): not really an organ-extension of hypothalamus: composed mostly of axons of hypothalamic neurons-extend downward as large bundle behind anterior pituitaryforms so-called pituitary stalk-appears to suspend anterior gland from hypothalamus. b. Components of Pituitary Gland 1) Anterior portion: adenohypophysis **know this!! Name & Source Functions GH (growth hormone; Somatotropin, STH) *anabolic, promotes protein synthesis> mobilizes glucose and free fatty acids; stimulates liver to produce insulin-like growth factor-1 (IGF-1) also known as somatomedin C; > stimulates growth of bones and soft tissues. ACTH (adrenocorticotrophic hormone; corticotrophin) Stimulates growth of tissues and bone; protein synthesis; stimulates growth of body (epiphyseal plates long bones in youth); promotes inc. mitosis; inc. size of cells; dec. CHO utilization in striated muscle and adipose tissue; inc. mobilization of stored fat; inc. use of fats for energy Stimulates production of hormones from adrenal cortex, esp glucocorticoids* Stimulate secretion of adrenal cortex hormones (release cortisol) Stimulates growth of ovarian follicles and spermatogenesis in males Regulates growth gonads and their reproductive activities; female, ovulation and formation of corpus luteum; male, called Interstial cell-stimulating hormone (ICSH), stimulates testes >male sex hormones FSH (follicle stimulating hormone) LH (luteinizing hormone) RNSG 2432 1 Name & Source Prolactin (PRL); LTH (Prolactin; luteotropic hormone; luteotrotropin; lactogenic hormone: mammotropic hormone; mammotropin TSH (thyroid stimulating hormone; thyrotropin; thyrotrophic hormone) Functions Promotes mammary gland growth and milk production Stimulates synthesis & release of thyroid hormones by thyroid: Stimulates uptake iodine and release of T3 & T4 (*Calcitonin from thyroid; reduces serum calcium levels by dec bone resorption & resorption of calcium in kidneys * If too much secretion of prolactin what occur? >Milk secretion!! * If too much release of LH what would occur? > enlarged reproductive organs; not enough…undeveloped reproductive organs! **Key -*Identify source of problem-Primary: organ itself; secondary: defect outside of gland itself) Posterior portion: neurohypophysis (*Listen to Kelly & Pituitary Tumor)-Stores and releases hormones produced by hypothalamus Name & Source Functions ADH; Vasopressin; Antidiuretic; Hormone Oxytocin 2. Promotes H2O retention by way of renal tubules > dec urine formation; stimulates smooth muscle of blood vessels and digestive tract Stimulates release of milk and contraction of smooth muscles in uterus; Sucking stimulates inc. secretion of oxytocin 2) Intermediate (pars intermedia) *secretes MSH (melanocytes for skin pigmentation Thyroid gland (review): produces Thyroid hormone (TH) composed of: Name & Source Functions 1.Triiodothyronine (T3); (more rapid and potent; action - shorter duration Thyroxine (T4) Calcitonin 3. Aid in growth/development; inc.basal metabolic rate (BRR) assoc with inc. 02 consumption/heat production; shorter acting; more rapid, potent than T4 As above; slower action Lowers serum calcium and serum phosphate-inhibit bone resorption; *Dec. excessive calcium by slowing calcium release by bone cells Parathyroid gland:(review) produces PTH hormone: (inc. renal excretion of phosphate, dec. excretion of CA, releases calcium from bone) Name & Source 1. Functions Regulates CA & PO4 metabolism as result of its effects on 3 target organs: Bone, Kidney, GI Parathyroid Hormone (PTH) 4. Adrenal Gland: 2 parts: cortex and medulla (p. ) a. Parts: 1) Inner medulla: source of catecholamines (*neurotransmitters); hormones when secreted by adrenal medulla-when released into circulation > epinephrine and norepinephrine- innervated by preganglionic sympathetic fibers- extension of sympathetic nervous system. a) Outer cortex: secretes several classes steroid hormones (glucocorticoids and mineralocorticoids); few others b) Components (1) Adrenal Medulla: Hormones: catecholamines Name & Source Functions Inc. blood glucose, stimulate ACTH, glucocorticoids; inc. rate and force of cardiac contractions; constricts blood vessels in skin, mucous membranes, kidneys; dilates blood vessels in skeletal muscles, coronary and pulmonary arteries; *Acts on beta –adrenergic receptors 1. Epinephrine (75%) 2. Norepinephrine (15%) Inc. heart rate, force of contractions; constricts blood vessels throughout body; * Acts on alpha-adrenergic receptors As above 3. Dopamine (2) Adrenal Cortex (Salt, sugar and sex)*can’t live without! Hormones: corticoids*Know function=nursing problems! Name & Source 1. Mineralocorticoids: aldosterone 2. Glucocorticoids: Cortisol, cortisone *can’t live without it; *Stress makes you fat! Functions Retains Na and water to inc. blood volume and BP pressure; excretes K+* CHO metabolism-regulating glucose use in body tissue, mobilize fat, shifting energy source for muscle cells from glucose to fat; **Respond to stress *Depresses inflammatory response, inhibits immune system *Affects carbohydrate, protein and fat metabolism 3. Sex hormones 2 RNSG 2432 Androgens & Estrogens Pancreas (endocrine portion) (review) Name & Source 1. 2. 3. Functions Glucagon (alpha cells) Increases blood glucose Insulin (beta cells) Decreases blood glucose Somstostatin (delta cells) Inhibits secretion of glucagons and insulin Gonads (review only) Name & Source Functions 1. Androgens (mainly testosterone) Male sex hormone 2. Estrogen and progesterone Female sex hormone (several types of estrogens) Keys to Assessment of Endocrine Function (review) – Health assessment interview inc. medical history, family history, changes in size or functioning of organs, skin, hair; changes in thirst, appetite, weight, energy, sleep; use of medications that may affect hormones; changes in reproductive functioning, secondary sex characteristics A. Physical Assessment including: palpation of thyroid; inspection of skin, hair, nails, facial appearance; reflexes, musculoskeletal system; height, weight, vital signs; assessment for hypocalcemia B. Abnormal findings 1. Skin assessment a. Pigmentation: hyper or hypo with adrenocorticodysfunction b. Rough, dry skin, yellow cast with hypothyroidism c. Smooth, flushed skin with hyperthyroidism d. Purple striae (stretch marks) e. Skin lesions on extremities: diabetes mellitus 2. Hair and nails a. Pigmentation with hypoadrenocorticofunction b. Dry, thick, brittle nails and hair with hypothyroidism c. Thin, brittle nails, thin soft hair with hyperthyroidism d. Excessive hair growth with hyperadrenocorticofunction 3. Facial Assessment a. Abnormal growth, symmetry with excess growth hormone b. Exophthalmoses (protruding eyes) with hyperthyroidism 4. Thyroid assessment a. Enlargement of thyroid gland or goiter b. One or multiple palpable nodules 5. Motor function assessment a. Increased deep tendon reflexes with hyperthyroidism b. Decreased deep tendon reflexes with hypothyroidism 6. Sensory function assessment Peripheral neuropathy or paresthesias with diabetes, hypothyroidism, excess growth hormone 7. Musculoskeletal assessment 8. Size and proportion, insufficient or excess growth hormone 9. Hypocalcemic tetany (possible thyroid, parathyroid abnormalities) *Trousseau’s sign (carpal spasm with inflation of blood pressure cuff) *Chvostek’s sign (tap front of client’s ear in angle of jaw to elicit facial muscle contraction) **Note-refer to p. 1248-1251 tab. 48-8 for Dx studies Endocrine system- important reference *Reminder- (lev2) covered thyroid, parathyroid function (review), not a testing focus in lev4, however, student responsible for content previously covered. A. Pituitary Gland Disorders Anterior Pituitary Gland (Adenophyophysis) HYPERfunction Etiology/Pathophysiology of Hyperfunction of Anterior Pituitary Gland (Lewis p.1218 ) 1. Etiology/Pathophysiology: a. Primary- defect in gland itself which releases that particular hormone that is too much or too little as Cushings b. Secondary-defect is somewhere outside the gland c. HYPERfunction of anterior pituitary gland d. Most often cause - benign adenoma producing excess hormones 1) growth hormone (GH), Prolactin (PRL), or ACTH 2) 10% OF ALL BRAIN TUMORS RNSG 2432 3 e. B. C. Specific Conditions 1) Gigantism a) Growth hormone hypersecretion occurs prior to puberty b) Result > person become excessively tall (over 7 feet tall) 2) Acromegaly: (See p. 1256 fig 50-1) a) Growth hormone (GH) HYPERsecretion (somatotropin) occurs after puberty > bone and connective tissue continue to grow enlargement face, hands, and feet 3) Overproduction of prolactin secretion (prolactinomas) dec. reproductive & sexual function (p. 1258) 4) *Cushing’s Disease (inc ACTH due to pituitary adenoma) 2. **Know anterior pituitary hormones (refer to chart with hormones produced & Tab 48-1); includes GH,TSH, ACTH, MSH, Prolactin, & FSH & LH Clinical Manifestations/Complications HYPERfunction of Anterior Pituitary Gland 1. *Manifestations depend upon which hormone(s) is/are produced in excess a. Giantism in children 1) skeletal growth; may grow to 8 ft. tall and > 300 lbs b. Acromegaly in adults 1) usually seen in those age 40-60 years 2) enlarged feet/hands, thickening of bones, prognathism (extension of mandible that occurs when problems in shape of face bones cause teeth to be misaligned), diabetes, HTN, wt. gain, H/A, visual disturbances, diabetes mellitus, facial changes 3) *Risks enlarged tumor lead to pressure on surrounding tissue; visual disturbance, predisposed to atherosclerosis, hyperglycemia, left ventricular hypertrophy etc (p. ) Collaborative Care for HYPERfunction of Anterior Pituitary Gland 1. Diagnostic Tests: (p.1213, Tab. 48-8) a. Key; history and physical exam b. Evaluation of GH levels; GH response to oral glucose challenge *GH antagonizes action of insulin > hyperglycemia c. MRI to identify pituitary hormone; CT scan with contrast d. Opthalmologic exam and visual fields due to pressure on optic chiasm or optic nerves 2. Treatment: a. Medications: goal-dec. GH levels (initial treatment or adjunct therapy) 1) *Somatostatin analogs as octreotide (Sandostatin- reduce GH levels-also powerful vasoconstrictor) see dosage/administration *Note-use to treat Cushing disease when due to pituitary tumor- see text p. 1257 2) GH receptors antagonist-Pervisomant (Somavert) for patients who had surgery and/or radiation therapy still have hypersecretion GH 3) Dopamine agonists as cabergoline (Dostinex); also bromocriptine (Parlodel) inhibits prolactin release (dec. GH hormone levels in acromegaly,*also used in Parkinsonism) b. Radiation therapy: external radiation- reduce GH levels in 30-70% of patients (usually given with medications); long time for success >develop hypopituitarism with radiation >replacement therapy; c. *Sterotactic radiosurgery-for small, surgically inaccessible tumors (post-op at inc.risks for seizures) d. Surgical removal (hypophysectomy) *treatment of choice; cure if tumor smaller than 10mm; usually with **transsphenoidal hypohysectomy *through floor of nose into sella turcica-most common method (See p. Fig 50-2); goal remove only tumor causing GH secretion; procedure > immediate dec. IGF-1 levels within few weeks. (Can also use transcranial (upper part of skull) if larger tumor; smaller, endoscopic through nostril-front of sphenoid sinus) 1) Pre-op hypophysectomy: a) Anxiety r/t body changes, fear of unknown, brain involvement, chronic condition; requiring life-long care b) Sensory-perceptual alteration r/t visual field cuts, diplopia and secondary to pressure on optic nerve. c) Alteration in comfort (headache) r/t tumor growth/edema 2) Post-op (was entire pituitary removed or only tumor; what type of procedure?) – Neuro checks vital! a) Knowledge deficit: post-op teaching including pain control, ambulation, hormone replacement post-surgery. activity restrictions b) Post-op; elevation HOB 30%; activity restricted (bedrest), NO straining/ bending for 2 months, use stool softners; avoid coughing, straining, saline mouth rinses (no tooth brushing-risk of meninitis); potential*CSF leak where sella turcica was entered 4 RNSG 2432 (usually resolves within 72 hours); *Important to *test clear nasal drainage for glucose (above 30 mg.dl); notify physician; spinal taps to relieve pressure!! c) Periocular edema/ecchymosis d) *Monitor, treat for post-op complications as diabetes insipitus > hypovolemic shock; very thirsty, urinate a lot!! *Due to lack of ADH (antidiuretic hormone)> Diabetus Insipitus due to involvement of posterior pituitary!! If develops-must be replaced through hormone replacement (DDAVP-Desmopressin, synthetic ADH, give by spray or pitressin IM)!** Know this e) Risks- dec. ACTH > require cortisone replacement due to dec glucocorticoid production. Can’t live without glucocorticoids! f) Risks dec. in sex hormones >infertility due to decrease production of ova & sperm (FSH, Prolactin) g) If hypophysectomy-or damage to pituitary-need ADH, cortisol &, thyroid replacement life-long- Understand significance! 3) Stereotactic radiosurgery a) Required use of stereotactic head frame, specialized unit; use of “pins”, 24 hours obs b) Post-op risk of seizures Note- excesses of other Tropic Hormones 3. *Lead to syndrome related hormone excess from target organ as ACTH excess lead to Cushing’s disease; inc TSH cause hyperthyroidism 4. Prolactinomas (prolactin-secreting adenomas), *most commonly occurring pituitary tumor (read manifestations p.1258); treat commonly with dopamine agonists as bromocripine (Parlodel) Pituitary Gland Disorders Anterior Pituitary Gland HYPOfunction A. Etiology/Pathophysiology of Hypofunction of Anterior Pituitary Gland (Lewis p.1258) 1. Etiology (rare) may be due to disease, tumor, or destruction of gland. 2. Selective hypopituitarism-only one hormone deficient or panhypopituitarism, deficient all hormones (what signs & symptoms?); most common-involve GH & gonadotrophins 3. Due to tumor, autoimmune; pituitary infarction (Sheehan’s syndrome-*understand this), pituitary gland destruction > end-organ failure (target organ effect); can be life-threatening as with lack of ACTH > effect on adrenal gland (*understand this). B. Common Manifestation/Complications Hypofunction of the Anterior Pituitary Gland 1. Signs/symptoms dec. hormones: GH, FSH/LH, Prolactin; ACTH; TSH C. Collaborative Care for Hypofunction of the Anterior Pituitary Gland 1. Diagnostic Tests: MRI, CT Scan; Serum hormone levels as Somatomedin C,Growth hormone stimulation test, Gonadotropin levels,Water deprivation levels, Prolactin levels (See 1213-1216). Tab 48-8) 2. Treatment: a. neurosurgery: removal of tumor b. radiation: tumor size c. hormone replacement: cortisol, thyroid, sex hormones 3. Assessment of S & S of hypo or hyper:functioning hormone levels 4. Teaching-Compliance with hormone replacement therapy: counseling and referrals and support medical interventions 5. Life-long hormonal therapy! Posterior Pituitary Disorders (neurohypophysis) Posterior HYPERpituitary Disorder Syndrome of Inappropriate Antidiuretic Hormone (SIADH) A. Etiology/Pathophysiology of Syndrome of Inappropriate Antidiuretic Hormone (SIADH) (p.1259) 1. Normal physiology a. 2 hormones released by posterior pituitary when signaled by hypothalamus b. ADH-antidiuretic hormone or (vasopressin/AVP) a) Secreted by cells in hypothalamus; stored in posterior pituitary; acts on distal and collecting tubules of nephrons>more permeable to H20>dec. water volume excreted b) Secreted in response to changes in serum osmolality (concentration of particles) *Normal serum osmolality-285-295 mOsm/kg; NA 135-145mEg/L; urine sp gravity 1.010-1..30 c) Vasoconstrictive action d) *Released in response to (1) dec. blood volume (2) inc. concentration of Na+ or other substances (3) periods pain, stress RNSG 2432 5 (4) B. C. *ADH-vasoconstrictive action-regulates extracellular fluid volume through renal handling>inc. volume, inc. cardiac output, inc. arterial pressure. *Under normal conditions- no vasconstrictive effect. 2) Oxytocin (cuddle hormone) *only positive feedback hormone in body a) controls lactation/stimulates uterine contraction b) Research links oxytocin and socio-sexual behavior 2. Etiology of SIADH a. *Occurs when ADH released despite normal or low normal plasma osmolarity (see Fig 503, p 1259) >*from abnormal production or sustained secretion of ADH – too much ADH b. Various causes: (see Table 50-1, p.1259) 1) **Malignant tumors - most common cause – especially small cell lung cancer, pulmonary disease, CA duodenum/pancreas 2) CNS disorders, trauma, 3) Drug Therapy (Vincristine, nicotine, general anesthestics, tricyclic antidepressants 4) Miscellaneous conditions 3. Pathophysiology a. Excess ADH inc. permeability of distal tubule & collecting duct reabsorption of H2O into circulation extracellular fluid volume inc., plasma osmolarity dec., GFR inc., Na+ dec.(dilutional hyponatremia) Clinical Manifestations/Complications Syndrome of Inappropriate Antidiuretic Hormone (SIADH) 1. Excess 2. Characterized by a. fluid retention; *weight gain b. serum hypo-osmolality; *dilutional hyponatremia & water intoxication (low serum Na)hypochloremia c. *dec. urine output/concentrated urine (*inc. urine osmolality) in presence of normal or inc. intravascular volume d. normal renal function 3. Clinical presentation a. Initially 1) Thirst 2) DOE 3) Fatigue, weakness, diarrhea; dulled sensorium, headache 4) Muscle cramps 5) Dec. UO; inc. weight gain 6) If serum Na+ dec. (usually < 120mEq/L) *Hyponatremia worsens>lethargy 7) Abdominal cramping, vomiting; muscle twitching 8) *Seizures-cerebral edema cerebral edema, lethargy, anorexia, confusion, HA, coma 4. More common in older adult Collaborative Care for Syndrome of Inappropriate Antidiuretic Hormone (SIADH) 1. Diagnosis by simultaneous measurements of urine & serum osmolality 2. Immediate goal: restore normal fluid volume & osmolality 3. Diagnostic tests *know this! a. Labs to monitor 1) Dilutional hyponatremia a) Serum Na+ < 134mEq/L b) Serum osmolality < 280mosm/kg c) Urine sp. gravity > 1.005 & urine osmolality (be inc.) d) BUN- dec. or normal e) *FYI: serum osmolality much lower than urine osmolality indicative of inappropriate excretion of concentrated urine in presence of dilute serum 4. Treatment *know this-*Fluid restriction important *p. 1260 Tab 50-2 a. Treat underlying problem- chemo (if not drugs causing the problem), radiation b. Medications stimulating release of ADH avoid/discontinue such as opoids, thiazide diuretics, tricyclic antidepressants, etc (see Table 50-1, p.) c. Drugs to treat 1) *Demeclocycline (Declomycin) (a tetracycline) & Lithium a) Lithium- inhibits renal response to ADH; 900-1200 mg po TID or QID in divided doses; max. 2400 mg po daily. b) Declomycin-produces diuresis by inhibition by inhibitng ADH induced water reabsorption (blocks effect of ADH on renal tubules-only tetraclycine that does this) d. If serum Na+ >125mEq/L (mild) 6 RNSG 2432 1) D. E. A. *Restrict PO fluids to 800-1000ml/day (correct hyponatremia)- If HF- Lasix- temporary fix – to promote diuresis (only use if serum Na greater than 125mEq/L; caution if dec. K, Mg, Ca & may need supplements for low levels) e. If serum Na+ <120mEq/L 1) IV hypertonic saline solution (3% or 5%)- adm at very slow rate, usually over 3-6 day period. (WHY???) 2) May restrict PO fluids to 500ml/day Nursing Assessment/Management of SIADH (p.1260-Tab. 50-2) 1. Subjective Data a. Health history b. Medication history 2. Objective Data a. Weight gain (without edema); due to atrial natriuretic peptide (ANP) leads to dec. BP, inc. sodium excretion, (sodium escape mechanism) b. Review lab results Pertinent Nursing Problems and Intervention for SIADH 1. Nursing Diagnosis a. Fluid volume excess b. Risk for decreased cardiac output r/t fluid volume excess c. Knowledge deficit 2. Nursing Interventions) a. Frequent vitals b. **Monitor I&O --1) Restrict fluids 2) look for dec. UO c. **Monitor labs 1) urine specific gravity inc. 2) serum Na+ decline d. **Daily weights- look for weight gain w/o edema (1 lb weight = 500 ml fluid retention) e. Monitor LOC f. Monitor heart & lung sounds g. Observe for S/S hyponatremia (KNOW THESE!!) (review) 3. *Positioning-HOB flat or no more than 10 degrees-enhance venous return to heart, inc left atrial filling pressure, reduce ADH release 4. *Protect from injury, potential for seizures 5. Rehabilitation and Home Care a. In case of Chronic SIADH 1) Teach fluid restriction 2) Instruct on chewing sugarless gum or ice chips to combat thirst 3) Educate on diuretic medications & supplements 4) Teach S&S of fluid/electrolyte imbalances Posterior Pituitary Gland Disorders-HYPOpituitary ADH Disorders Diabetes Insipidus (DI) Etiology/Pathophysiology of Diabetes Insipidus –“Too little ADH” (Lewis p.1261) 1. Normal physiology a. 2 hormones released by posterior pituitary (*refer to above) 1) ADH (vasopressin) a) Secreted by cells in hypothalamus b) Vasoconstrictive action c) Released in response to (1) dec. blood volume (2) inc. concentration of Na+ or other substances etc. 2) Oxytocin 2. Etiology a. Brain tumors b. Closed head trauma &/or other brain conditions c. Renal failure d. 50% idiopathic 3. Pathophysiology (see Table 50-3, p. 1261) *understand differences a. **Assoc with deficiency of production/secretion of ADH b. ADH insufficiency from neurogenic or nephrogenic origin -- too little ADH 1) central (neurogenic DI) – usually occurs suddenly RNSG 2432 7 a) B. C. any organic lesion of hypothalamus, infundibular stem, or posterior pituitary interferes with ADH synthesis, transport or release b) head trauma; if infection, trauma, may resolve; If surgical issue following to brain surgery for tumor-may be permanent problem 2) nephrogenic DI - inability of tubules to respond to ADH often due to drug therapy, renal damage, hereditary a) Lithium – most common cause if due to drug-also Declomycin b) Hypokalemia & hypercalcemia 3) psychogenic DIa) less common condition; can be a structural lesion or a psychological disorder leading to water intoxication*like drinking contests, exercise and excessive ingestion water without replacing electrolytes: Is it true DI? Clinical Manifestations/Complications of Diabetes Insipidus (see Figure 50-4, p.1260 *Understand patho for sign/symptoms! 1. Large amounts dilute urine-5 to 20 L/day 2. Risk for dehydration and hypernatremia 3. **Polydipsia…important to prevent dehydration! 4. **Polyuria (10-20 L in 24 hours) a. low urine specific gravity < 1.005 b. have and urine osmolality of < 100mOsm/kg. c. *serum osmolality inc as result hypernatremia due to pure water loss in kidney 5. Severe fluid volume deficit a. wt loss b. tachycardia c. constipation d. *shock (hypovolemic) Collaborative Care for Diabetes Insipidus 1. *Identification of cause- initial step 2. Complete history & physical 3. Diagnostic tests (p.1261) and Tab. 48-8 a. *Urine specific gravity dec.-less than 1.005; serum NA above 145mEq/L; serum osmolality above 295; urine osmolality less than 300. b. Dehydration test- *need baseline prior to testing 1) 2 units of Vasopressin(ADH) mixed in saline adm over 2 hrs then check urine osmolality levels; if rise 9% or greater in urine osmolality-confirms = central DI, if none nephrogenic DI c. Water deprivation-confirms diagnosis of central DI 1) First: a) baseline weight, pulse & BP; labs- urine, plasma osmolalities, sp. gravity 2) Then withhold all fluids for 8 to 16 hours; *cannot let them drink 3) *Potential risk fluid volume deficit-*hypovolemic shock (done in hospital setting) 4) During test, patient assessed hourly for BP, weight, urine osmolality; test continues until urine osmolalities stabilize (hourly increase less than 30 mOsm/kg in 3 consecutive hours or body weight declines by 3% or orthostatic hypotension develops. p. 1297) d. What is expected urine sp. gravity; serum Na & serum osmolality without treatment? (p. 1261) 4. Medical Mangement/Treatment a. Identify first etiology, H & P; Treat underlying problem b. Central- Administer IV hypotonic fluids (saline or D5W) titrate to replace lost fluids 1) Inc. oral fluids 2) *Replace ADH hormone (Desmopressin acetate) (DDAVP) *know this)- give IV, nasally, orally 3) 4) 8 RNSG 2432 Pitressin (Vasopressin) sc, nasal spray Chlorpropamide (Diabenese) –useful for partial central DI c. D. E. A. Nephrogenic-above not-use dietary measures, low sodium, thiazide diuretics, indomethacin *know why effective) p. 1261 Nursing Assessment Specific for Diabetes Insipidus 1. Subjective Data a. Medical history b. Medication history 2. Objective Data a. Head to toe assessment b. Monitor labs Pertinent Nursing Problems and Intervention for Diabetes Insipidus 1. Nursing Diagnosis a. Risk for injury (hypovolemic shock) b. Knowledge deficit c. High risk for ineffective coping 2. Nursing Interventions a. Identification of etiology, H & P b. Tx of underlying problem c. **DDAVP (desomopressin acetate) (nasal spray); Pitressin s.c. IM, nasal spray *know how, why this med works, implications! d. Assess for F & E imbalances e. High risk for sleep disturbances f. Increase po/IV fluids 3. Rehabilitation and Home Care a. Daily weights – report changes b. Medication education – s/s of side effects Arenal Cortex Disorders HYPERfunction Cushing Syndrome/Disease Etiology/Pathophysiology of Cushing Syndrome/Disease *great resource Adrenal Cortex- “think”- Salt, Sugar, Sex 1. Normal physiology a. 3 main adrenal cortex steroid hormones (i.e. corticosteroids) 1) Glucocorticoid (Sugar) a) Regulate metabolism b) Increase blood glucose levels c) Critical in physiological stress response (1) Primary glucocorticoid = Cortisol (many actions) (2) Cortisol-*metabolism of CHO (carbohydrates)- regulation blood glucose- inc thru glucogenesis, dec. during fasting (3) Cortisol- control of fat metabolism –stimulates fatty acid metabolism from adipose tissue (4) Cortisol-control of protein synthesis in liver; protein breakdown in tissues; role in sodium/water balance & fight/flight response (5) Cortisol- inflammatory response (dec inflammatory response); bad if increased cortisol and trying to heal (6) Exogenous forms Corticosteroids used: *predniSONE, *cortisone, *dexamethasone (Decadron), *hydrocortisone (Cortef), *methylPREDNISolone (Solu-Medrol)- Caution in administration; note some IV, others po form 2) Mineralcorticoid (Salt)*Fluid and electrolyte balance/extracellular fluid volume What stimulates aldosterone secretion? –remember renin-angiotensin-aldosterone system What inhibits aldosterone secretion?-Atrial Naturetic Peptide (ANP);hypokalemia a) Regulate sodium (sodium/water retention) & potassium balance RNSG 2432 9 b) 3) 4) Hydrogen ion excretion (1) Primary mineralcorticoid = Aldosterone (2) *If Na level low-aldosterone level inc.;if *K+ high, aldosterone level inc. (understand this); what effect if aldosterone too low, what effect on K+? Androgen(Sex)*Also estrogen a) Contribute to growth & development in both genders b) Contribute to sexual activity in adult women c) Androgen-hormones which inc. male characteristics; release of testosterone Review a) Release of Glucocorticoids-controlled by hypothalamic-pituitary-adrenal axis (review physiology- remember anterior pituitary produces –ACTH- stimulates adrenal cortex to secrete corticosteroids/cortisol) p. b) ACTH- Circulating levels of cortisol Dec. levels cause inc. of ACTH Inc. levels cause dec. of ACTH What kind of feedback mechanism is this? (negative) *ACTH levels affected by: individual biorhythms: ACTH levels highest 2 hrs before and just after awakening (usually 5 am-7am; then gradually dec. rest of day- STRESS inc. cortisol production and secretion. Usually produce 20 mg day (most in am); can inc. up to 500 mg day if needed!! B. Function Adrenal Cortex Hormones Cushing Syndrome vs Cushings Disease 2. General information r/t Cushing Syndrome (see p. 1276, 1277 Tab. 50-13, 14) a. Spectrum of abnormalities caused by excess corticosteroids b. Particularly glucocorticoids = Cortisol (Hypercortisolism) c. More common in females ages 30-50 years old 3. Etiology/Pathophysiology (see Tab. 50-13) a. Cushing’s Disease – ( disease if Pituitary cause leads to excessive ACTH production) 1) Pituitary cause 2) Endogenous Cushing Syndrome 3) Primary origin of problem – secreting pituitary adenoma (tumor) 4) Overproduction/secretion of adrenocorticotropic hormone (ACTH) 5) Inc. ACTH = inc. Cortisol-accounts for 85% of endogenous Cushing Syndrome b. Cushing’s Syndrome –‘syndrome’ – group of signs & symptoms due to too much corticosteroid; problem comes from source other than pituitary cause/tumor 1) Adrenal cause a) Excessive production of cortisolnegative feedback to pituitary suppresses pituitary ACTH production b) Results in atrophy of uninvolved adrenal cortex (*Adrenal tumor inc cortisol dec ACTH adrenal cortex atrophy) *Need to understand “why”! 2) Ectopic cause due to ACTH-secreting tumors a) Small-cell lung cancers, random and episodic ACTH Production b) Tumor=inc ACTH=inc cortisol 3) Iatrogenic (medically induced Cushings) admin of exogenous corticosteroids cause – as prednisone; steroid use inc. cortisol dec. ACTH adrenal cortex atrophy Clinical Manifestations/Complications of Cushing Syndrome/Disease 1. (See Table 50-14 & Fig 50-11, 12 p.1277) *Symptoms due to inc secretion of cortisol/or excess exogenous (derived or originating externally) corticosteroids as prednisone); 4 X more common in females, usually occurs at 20-40 yrs age. 2. Signs and symptoms **related to adrenal cortex functions i.e. effect functions of adrenal cortex “sugar, sex, and salt”: a. Mineralcorticoid excess – (aldosterone) (see p.307-Fig. 17-9,10*understand process). *Sodium & water retention (no edema) 1) Hypertension-secondary to fluid retention etc. b. Androgen excess (testosterone)- acne, virilization in women, feminization in men, etc c. Glucocorticoid excess (cortisol)*pronounced changes-physical appearance etc*key 1) Mood changes, phychic stimulation, euphoria, irritability, etc. 2) Cortisol induced insulin resistance hyperglycemia 3) Electrolyte abnormalities a) Hypernatremia, hypokalemia (mineralocorticoid effect) 10 RNSG 2432 4) C. Protein wasting (inc. protein metabolism) a) muscle wasting weakness b) Loss of protein matrix osteoporosis pathological fractures c) Loss of collagen weak, thin skin, bruises easily, abdominal striae d) Delayed wound healing; *Changes in fat metabolism 5) Dec. immune response (anti-inflammatory response of steroids)-more prone to infection; *infection-common cause of death a) hematology- dec. WBC, lymphocytes, eosinophils 6) Clinical presentation a) Truncal obesity b) Moon face c) Purplish red striae (usually usually depressed below the skin surface on abdomen, breast, or buttocks (see Fig 50-12) d) hursutism in women; menstrual disorders in women e) hypertension; unexplained hypokalemia Collaborative Care for Cushing Syndrome/Disease (p.1278 Tab. 50-15) 1. Goal: identify underlying cause & normalize hormone secretion 2. Diagnostic tests (click here for more information) (think adrenal cortex function & relationship to pituitary & ACTH) a. Labs p. 1276 and Tab. 48-8 1) **24 hour urine collection for free cortisol *most indicative a) *50-100mcg/day = Cushing Syndrome-*significant finding b) *If borderline results high dose dexamethasone suppression test performed (1) If ACTH not suppressed with cortisol > adrenal tumor (2) If very high levels of cortisol needed to suppress ACTH >adrenal cortex hyperplasia 2) Plasma cortisol levels for diurnal variations –(primary glucocorticoid) – 3) May be elevated in mornings, low in afternoon & evenings *important 4) *Plasma ACTH levels – may be low, normal, or elevated – depends on underlying cause a) Normal/high – indicates ACTH-dependent Cushing’s Disease b) Low/undetectable – indicates adrenal/exogenous etiology 5) 17-Ketosteroids (urinary measurement of adrenocorticoid and gonadodal function and ) (p. 6) Basic Metabolic Panel a) inc. sodium & glucose, dec. potassium & calcium (WHY?) 7) CBC b. CT scan/MRI/Petrosal sinus sampling 1) Of pituitary & adrenal glands c. Petrosal sinus sampling-not always required, may be best way to distinguish pituitary from ectopic causes of Cushing’s syndrome. Samples blood drawn from petrosal sinuses—veins that drain pituitary—insert tiny tubes through a vein in upper thigh or groin region d. Treatment- If caused by: 1) Pituitary adenoma a) Hypophysectomy (removal of pituitary gland) (1) removal of pituitary gland through transphenoidal (through nostril) route or craniotomy (see previous notes-pituitary & p. fig. 50-2) (2) radiation of pituitary if pt. not good surgical candidate 2) Adrenal tumors a) Adrenalectomy - removal of adrenal gland-laparoscopic removal preferred unless malignancy suspected then “open” (1) if both glands removed, client requires *lifelong hormone replacement (2) *Risk for Addisonian Crisis & hypovolemic shock…Know why! (3) *Read carefully re pre-post care surgery on adrenal glands-risks etc p. 1279 understand implications/care 3) Ectopic ACTH secreting tumor a) removal of source of ACTH secreting tumors or treat primary neoplasm 4) *Radiation to tumors-if surgery not optimal; or to follow surgery 3. Drug Therapy (see p 1278.;Tab 50-15) 1) Ketoconazole (Nizoral); aminoglutethimide (Cytadren) *main meds; *Somatostatis analog octeotide suppresses ACTH secretion in some cases-used mostly to suppress GH (*read text- know/understand effect each drug) 4. *If due to long-term Steroid Therapy RNSG 2432 11 long term steroid therapy for “another condition” >potential problems; careful follow-upmaintain at lowest level of steroids for adequate treatment; effort to minimize untoward effects 2) Always taper off steroids!!!!* Know why?? (Not appropriate-ifused as replacement therapy) D. Nursing Assessment Specific for Cushing Syndrome 1. Subjective Data a. Past health history 1) Tumors or neoplasms, GI bleeding, frequent infections b. Current medications 1) Use of corticosteroids 2) Functional health patterns 2. Objective Data (Table 50-16) a. Weight gain – truncal obesity b. Integument c. CV d. Musculoskeletal e. Reproductive f. Monitor labs E. Pertinent Nursing Problems and Intervention for Cushing Syndrome 1. Nursing Diagnosis (understand pathophysiology & problems with each) a. Fluid volume excess – HTN, edema b. Risk for infection – immune suppressed, hyperglycemia, poor wound healing, etc. c. Disturbed body image – physical manifestations of syndrome d. Impaired skin integrity – altered skin fragility e. Imbalanced nutrition – increased appetite, high caloric intake, inactivity; *teach to follow diet high in protein 2. Nursing Interventions (p.1279) a. Proper collection of 24 hour urine specimen b. Pre/Post surgical patients (see p.1279) 1) ICU admission – post craniotomy 2) Education on possible life- long hormone replacement therapy 3) Education on not abruptly stopping hormone replacement 4) Medical follow up a MUST c. Emotional support d. Monitor vitals, daily weights, glucose, labs e. Monitor for possible infection f. Rehabilitation and Home Care g. Home health consult h. Wear medical alert bracelets i. Avoid exposure to extreme temps & infections Adrenal Cortex Disorders HYPOfunction (Adrenocortical Insufficiency) Addison’s Disease (primary and secondary) *Note defined as primary if adrenal cortex is “cause” (all 3 hormones involved); secondary if lack of pituitary ACTH secretion (rare involvement of mineralocorticoids) B. Etiology/Pathophysiology of Addison’s Disease* (adrenal cortex source of problem) (p.1280) a. Normal physiology (remember function)- 3 main adrenal cortex steroid hormones (i.e. corticosteroids) 1) Glucocorticoid a) Regulate metabolism b) Increase blood glucose levels c) Critical in the physiological stress response (1) Primary glucocorticoid = Cortisol 2) Mineralcorticoid a) Regulate sodium & potassium balance b) Hydrogen ion excretion (1) Primary mineralcorticoid = Aldosterone 3) Androgen= Testosterone a) Contribute to growth & development in both genders b) Contribute to sexual activity in adult women b. If lack of adrenal cortex function- What hormones do you have too little of?? (cortisol, aldosterone, testosterone * Deficiency of “salt, sex,& sugar”- hormones) 1) 12 RNSG 2432 2. C. Etiology 1) *Primary Addison’s disease a) Originates in adrenal glands b) Chronic deficiency of glucocorticoid, mineralcorticoid, & androgen hormones; Adrenal tissue destroyed by antibodies against patient’s own adrenal cortex; 80% of cases;*Most common cause- 90% tissue destroyed;“susceptibility” gene 2) Idiopathic (unknown cause) 3) Other: malignancy, TB, fungal infections (fatal if not treated), AIDS, metastic cancer 4) Adrenal insufficiency- most often in adults less than 60- if due to autoimmune cause – most common in white females 5) *Secondary adrenocortical insufficiency a) Cause disorder outside adrenal gland as pituitary tumor with corticotrophin activity b) Aldosterone (mineralocorticoid) secretion may be unaffected 6) Iatrogenic (therapy induced) Addison’s disease a) Untoward effect of anticoagulant therapy, trauma -client has bilateral adrenal hemorrhage b) Abrupt withdrawal from long-term, high-dose corticosteroid therapy c) Bilateral adrenalectomy, chemotherapy Clinical Manifestations/Complications of Addison’s Disease 1. *Manifestations usually not apparent until 90% of adrenal cortex destroyed a. Slow onset of symptoms b. Primary symptoms 1) Weakness, fatigue, weight loss & anorexia (know why) c. Fluid and electrolyte imbalances- dec- BP; hyponatremia, hyperkalemia (*inc. Na loss chiefly through urine, sweat, but also through; inc. retention K+), > low circulating blood volume- due to lack of mineralocorticoids > Orthostatic hypotension –(*Know why!!), syncope, > hypovolemic shock d. Dizziness, confusion, cardiac dysrhythmias e. Hypoglycemia(nausea, vomiting, weakness, lethargy, diarrhea) from CHO metabolic function of cortisol f. Also dec. adrogen function; hair loss, dec. sexual function; mental disturbances; salt craving; g. Hyperpigmentation (click here)– small black freckles –know why due to inc. ACTH levels (bronzed appearance in Caucasians); (*Dec. plasma cortisol reduces feedback inhibition of pituitary ACTH, plasma ACTH rises & inc. secretion of melanocyte stimulating hormone (MSH) occurs* - Primary Addison’s disease *Primary Addison’s…common findings: Poor coordination, Dry skin and mucous membranes,Sparse auxiliary and pubic hair in women, Skin- typically deep bronze especially increases of hands and on knuckles, elbows and knees; skin shows darkening of scars, areas of vitaligoo Abnormal coloration due to dec. secretion of cortisol- glucorticoid causes pituitary gland to secrete excessive amounts of melanocyte-stimulating hormone (MSH) and corticotrophin. (as above) *Note: Secondary Addison’s adrenal hypofunction does not cause hyperpigmentation- corticotrophin and MSH levels are low. 2. Complications a. **Addisonian(Adrenal) Crisis (p.1281) -sudden electrolyte imbalance; hypoglycemia 1) *Sudden dec. or absence of adrenal cortex hormones (glucocorticoids- cortisol, mineralocorticoids-mainly aldosterone, and androgens-testosterone, estrogen) >*Lifethreatening response > circulatory collapse (hypotension, tachycardia, hyponatremia, hyperkalemia, hypoglycemia, fever, weakness & confusion (know/ understand this!) 2) Causes a) Inc. stress without inc. in dose of cortisol b) Triggered by stress- i.e. trauma, infection, hemorrhage, psychological stress c) Clients undiagnosed & exposed to stress d) Sudden withdrawal of corticosteroid hormone replacement therapy without tapering 3) *Major symptoms-as above (Know why?) fever dehydration (due to dec. NA, inc K) dec. serum sodium; inc. potassium dec. glucose- HYPOglycemia confusion, headache; pallor, inc HR, RR weakness, abdominal pain, diarrhea RNSG 2432 13 D. E. EKG changes –(remember elevated K+, dehydration; -low voltage, tall peaked T waves) HYPOvolemic shock, coma severe hypotension, circulatory collapse renal shut down, DEATH! 4) **Addisonian’s(Adrenal) Crisis *Treatment a) **Rapid IV replacement of fluids (*D5NS); high dose hydrocortisone replacement therapy until signs/symptoms disappear; prevent shock; Monitor for fluid overload b) Check VS, urine output and electrolytes frequently c) Monitor EKGd) Adm. Hydrocortisone (Solu-cortef) 100 mg IV bolus every 6 hrs. e) Hydrocortisone diluted with dextrose in NS given IV until condition stabilizes; May need up to 300 mg/day hydrocortisone and 3/5 L of IV NS in acute stage (may require 4-6 hours! ) f) Treat hyperkalemia (Bicarbonate, insulin, beta agonists as epinephrine to promote shift K blood to into cells; binding resins as Kayexlate to promote excretion of K+ from GI tract) g) Also try to decrease anxiety and stress h) May require vasopressors such as Dopamine or Epinephrine; avoid additional stress Collaborative Care for Addison’s Disease 1. Disease often advanced stage by time of diagnosis due to slow onset symptoms 2. Treatment focused on management of underlying cause 3. Diagnostic tests (See also Dx test for Cushing’s syndrome & p. 1281 tab 5017; and Tab. 48-8) a. Labs 1) *Plasma (serum) cortisol levels – dec. levels 2) Serum electrolytes – a) Hyperkalemia, hypocholoremia, hyponatremia, hypoglycemia 3) CBC – anemia 4) Elevated BUN 5) *Urine free cortisol – decreased 6) Plasma ACTH – elevated (if cause is adrenal dysfunction) 7) ACTH stimulation test - failure of cortisol levels to rise 8) Urinary 17 –Ketosteroids (measures androgen metabolites urine- evaluates adrenalcorticoid and gonadal function) p.. b. CT scan/MRI 1) Identify adrenal tumors or calcifications c. EKG 1) Low voltage & peaked T waves (what causes this?) 4. Interventions-*Drug Therapy (know this) a. See Tables 50-18,19, 20, p.1282-1283) b. Give hormones at times to reflect normal circadian rhythm c. Hormone replacement therapy (mainstay treatment)*Life long 1) Hydrocortisone (most commonly used drug)*review information on corticosteroid therapy p. 1283 Tab 50-21) a) has both glucocorticoid & mineralcorticoid properties b) inc. dose in times of stress c) *Note give in divided doses, 2/3 in am (20-25 mg); 1/3 in afternoon(10-12 mg) d) *May need to inc. dosages in times of stress-inc. need for cortisol! 2) Flurocortisone (Florinef) a) Mineralcorticoid replacement; daily, give in am 5. Diet changes a. Inc. salt in diet 1) 5-8grams/day (1 tsp salt = 2 grams Na) 2) Do not fast or omit meals & eat between meals 3) High carbohydrate & protein 6. Wear Medic alert bracelet 7. Carry kit of 100 mg hydrocortisone IM (emergencies); Teach family to administer IM injections a. Avoid infections/stress b. Avoid cold temperatures Pertinent Nursing Problems and Intervention for Addison’s Disease 1. Nursing Diagnosis a. Deficient fluid volume b. Risk for ineffective therapeutic regimen 14 RNSG 2432 2. B. C. Nursing Interventions a. Monitor vital signs, b. Monitor for signs of fluid volume deficit & electrolyte imbalance c. Monitor labs d. Daily weights e. Diligent corticosteroid administration f. Protect against exposure to infection g. Assistance with daily hygiene h. Education 1) Continue medication regimen (provide education on medications) 2) S&S of insufficient hormone levels 3) *Special care during times of stress/reduce stress (*need to increase dosage) Adrenal Cortex Disorders HYPERfunction (also known as Conn’s Syndrome) Hyperaldosteronism Etiology/Pathophysiology of Hyperaldosteronism (Lewis p.1284) 1. Normal physiology (review):3 main adrenal cortex steroid hormones (i.e. corticosteroids);Glucocorticoid; *Mineralcorticoid (aldosterone); Androgen 2. Etiology a. Excessive *aldosterone secretion (mainly mineralcorticoids) Aldosterone > regulates, Na, K+, Hydrogen b. Primary hyperaldosteronism (PA) 1) Caused by small adrenocortical adenoma (most common cause) 2) Occasionally multiple lesions; associated with bilateral adrenal hyperplasia c. Occurs in both genders around age 30-50 years, 1% of population d. Secondary hyperaldosteronism 1) Occurs in response to nonadrenal cause of elevated aldosterone levels a) i.e. renal artery stenosis, rennin-secreting tumors, CKD (chronic kidney disease) 3. Pathophysiology a. Characterized by hypertension w/hypokalemic alkalosis b. Inc. aldosterone secretion Na & H20 retention inc. blood volume HTN, headache, dec. K (hypokalemia) muscle weakness, cardiac dysrhythmias, metabolic alkalosis, rarely peripheral edema; also elevated urinary K+. inc. plasma aldosterone and Na levels with low plasma rennin levels (*Understand this concept!) Clinical Manifestations/Complications of Hyperaldosteronism 1. Sodium retention hypernatremia HTN, headache a. Edema does not usually occur d/t inc. in rate of Na excretion 2. Potassium wasting hypokalemia muscle weakness, fatigue, dysrhythmias, & glucose Intolerance 3. Hydrogen ion wasting metabolic alkalosis tetany Collaborative Care for Hyperaldosteronism 1. Suspected in all patients with HTN & hypokalemia who are not on diuretics 2. Goal: treat underlying cause 3. Diagnostic tests a. Labs 1) Primary hyperaldosteronism a) Elevated Plasma aldosterone b) Elevated Na c) Dec. K d) Dec. Plasma Renin activity e) Plasma 18-hydroxycorticosterone – measure after overnight bed rest - >50nh/dL indicates adenoma f) 24 hour urine collection – elevated urine K (excess K excreted) b. CT scan/MRI- adrenal gland – identify adenoma 4. Drug Therapy a. *Potassium sparing diuretics/other meds – re: tx HTN & hypokalemia 1) spironoaldactone (Aldactone) & *eplerenone (Ispra)-*new class of drug; amiloride (Midarmor); aminoglutethimiade (Cytadren) (*Review how these drugs work!) 2) Oral potassium supplements 3) Note: beware of causing Hyperkalemia 4) Dexamethasone - re: decrease hyperplasia 5) Calcium channel blockers – re: decrease BP RNSG 2432 15 5. D. E. A. B. Diet changes a. Low Na 6. Surgical a. Preferred method of treatment for primary hyperaldosteronism b. Removal of adenoma (adrenalectomy) Nursing Assessment Specific for Hyperaldosteronism 1. Subjective Data a. Medical history b. Use of diuretics 2. Objective Data a. Blood pressure b. Lab values Pertinent Nursing Problems and Intervention for Hyperaldosteronism 1. Nursing Diagnosis a. Fluid volume excess 2. Nursing Interventions a. Monitor blood pressures b. Administer medications to correct electrolyte imbalances & HTN c. Monitor cardiovascular status d. Pre/Post Op monitoring (Partial or total adrenalectomy) **Would you need to replace cortisol levels before or after surgery?? Pre-op stabilize hormonally; correct electrolyte imbalance; cortisol evening prior to surgery, AM of surgery and during surgery. 1) *Post-op: ICU; BP, fluid and electrolyte mgt; IV cortisol preparation 1 st 24 hours; IM cortisol 2nd post-op day then oral steroids 3rd day; have inc. susceptibility to infection, poor wound healing. Unilateral adrenalectomy steroids eventually weaned. (same as above) _________________________________________________________________ Adrenal Medulla Disorders HYPERfunction of Adrenal Medula Pheochromocytoma Etiology/Pathophysiology of Pheochromocytoma (p.1284) 1. Definition a. *Tumor of adrenal medulla 1) Adrenal medulla produces catecholamines a) i.e. epinephrine & norepinepherine (hormones that regulate heart rate & blood pressure) b) *over secretion of catecholamines (epinephrine, norepinephrine) 2. Incidence a. Rare disorder b. Affects both genders equally c. Can occur at any age – most commonly in young, middle-aged adults 3. Etiology/Pathophysiology a. Most cases – tumor 1) Benign;encapsulated 2) Unilateral;occasionally bilateral tumors found 3) Solitary 4. Secretion of excessive catecholamines severe hypertension if left untreated diabetes mellitus, cardiomyopathy, & death Clinical Manifestations/Complications of Pheochromocytoma 1. *Paroxysmal severe hypertension (episodic with epinephrine, norepinephrine released sporadically-systolic: 220 – 300; diastolic 150 – 175) with tachycardia-* Hallmark signs 2. Can be life-threatening; stressor induced 16 RNSG 2432 3. C. Deep breathing; pounding heart; headache; moist cool hands & feet; visual disturbances all due to HTN 4. Attacks may be provoked by medications a. Antihypertensives, opioid’s, contrast media, tricyclic antidepressants 5. Attacks may last minute to hours 6. If untreated > Diabetes Mellitus due to decreased insulin secretion from catecholamines which can induce insulin resistance; cardiomyopathy; death Collaborative Care for Pheochromocytoma 1. Diagnosis often missed --- less than 0.1% cause of all HTN cases 2. Goal: management of uncontrolled HTN) 3. Diagnostic tests a. Labs 1) *Urine fractionated catecholamines, creatinine & metanephrines a) Usually done by 24hour urine collection b) Most reliable and simplest test c) *Values elevated in 95% of cases 2) *24 hour urine-Vanillymandelic acid (VMA-metabolite of epinephrine) --- can have false positives Tab. 48-8) 3) *Plasma catecholamines – elevated a) Preferred to measure during acute attack b. CT scan/MRI 1) Adrenal medulla - evaluate for tumors c. Biopsy 1) Adrenal biopsy – definitive diagnostic test 4. Surgery a. *Adrenalectomy to remove tumor –primary treatment b. Focus =management of dangerously high BP; post adrenalectomy= adrenal crisis and need for long term steroids!! 1) Pre-op: (get BP down-dec. other symptoms of catecholamine excess) a) Sympathetic blocking agents (Adrenergic blocking agents) (1) Ex: Minipress (prazosin), Hytrin (terazosin), Cardura (doxazosin) (2) BP change- client may experience orthostatic hypotension b) Beta blocking agents (1) Ex: Inderal (2) Dec. BP, HR, force of contraction; calcium channel blocking agents also used. 2) General management a) Diet (1) high in vitamin, mineral, calorie, no caffeine b) Sedatives; *Monitor BP c) Eliminate attacks (1) If attack- complete bedrest and HOB 45 degrees 3) Surgery- laparoscopic adrenalectomy (1st choice) or open abdominal incision; a) complete removal of tumor cures hypertension in 10-30% of cases b) *During surgery -May require REGITINE AND NIPRIDE TO PREVENT HYPERTENSIVE CRISIS (How do these drugs work-potent vasodilators) 4) Post-opa) BP may be elevated initially, CAN BOTTOM OUT b) May require volume expanders, vasopressors c) Hourly I and O; Observe for hemorrhage 5) *See cautions re adrenalectomy (typically only tumor is removed); if entire adrenal gland removed; Addison’s crisis risk and long term steroids. a) If not a candidate for surgery- Use Demser (drug which inhibits catecholamine synthesis) b) *Avoid opiates, histamines, reglan, anti-depressants (stimulate SNS) RNSG 2432 17