file - European Urology
advertisement

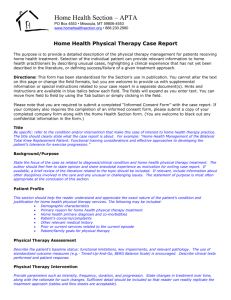
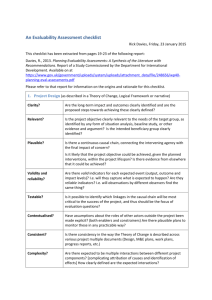
Supplement – Methods: Patient-reported outcomes Pain was evaluated using the Brief Pain Inventory-Short Form (BPI-SF) questionnaire [1] via paper forms at clinic visits at baseline, at day 1 of each treatment cycle, and at the end of treatment. The BPI-SF is measured on a scale of 0–10; lower scores represent lower levels of pain intensity or less interference of pain with daily living activities. The following pain measures were derived from the BPI-SF questionnaire: Mean pain progression was defined as an increase of ≥30% from baseline in the average of BPI-SF pain intensity item scores (Items 3, 4, 5, and 6) at two consecutive evaluations ≥4 weeks apart without a decrease in World Health Organization (WHO) analgesic usage score. Worst pain progression was defined as an increase of ≥30% from baseline in the BPI-SF worst pain intensity item score (Item 3) at two consecutive evaluations ≥4 weeks apart without a decrease in WHO analgesic usage score. Pain interference progression was defined as an increase at any visit in the baseline BPISF pain interference score of one half the baseline standard deviation of BPI-SF. Health-related quality of life (HRQoL) was evaluated using the Functional Assessment of Cancer Therapy-Prostate (FACT-P) questionnaire [2, 3] via paper forms at clinic visits at baseline, day 1 of cycles 3, 5, 7, and 10, and every third cycle thereafter, and at the end of treatment. The FACTP is measured on a scale of 0–156, with higher scores indicating better functional status. The functional status degradation was measured using the following composite scores: FACT-P total scale: decrease of 10 points from baseline. FACT-General (FACT-G) scale and trial outcome index: decrease of 9 points from baseline. Prostate Cancer Subscale, physical well-being, functional well-being, social/family wellbeing, emotional well-being: decrease of 3 points from baseline. The thresholds for pain and functional status were predefined based on existing evidence of score changes that are clinically meaningful to patients [2, 4-6]. For the analyses of time to mean pain intensity progression and worst pain intensity progression, patients who had not experienced pain progression at the time of analysis were censored on the last date they were known not to have progressed. Patients without on-study or baseline assessments were censored at the date of randomisation. Kaplan-Meier product limit methods were used to estimate the time to pain progression and HRQoL degradation distributions. Inferences for these time-to-event end points were assessed using a log-rank test stratified by Eastern Cooperative Oncology Group performance status (0 or 1). The hazard ratio and its 95% confidence interval were estimated from a stratified Cox proportional hazard model assuming a proportional hazard between the abiraterone and prednisone groups. References 1. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 1994:23;129-38. 2. Cella D, Nichol MB, Eton D, Nelson JB, Mulani P. Estimating clinically meaningful changes for the Functional Assessment of Cancer Therapy--Prostate: results from a clinical trial of patients with metastatic hormone-refractory prostate cancer. Value Health 2009:12;124-9. 3. Victorson DE, Beaumont JL, Rosenbloom SK, Shevrin D, Cella D. Efficient assessment of the most important symptoms in advanced prostate cancer: the NCCN/FACT-P Symptom Index. Psychooncology 2011:20;977-83. 4. Farrar JT, Young JP, Jr., LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001:94;14958. 5. Sloan JA, Cella D, Hays RD. Clinical significance of patient-reported questionnaire data: another step toward consensus. J Clin Epidemiol 2005:58;1217-9. 6. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 2008:9;105-21. Supplemental Fig. 1 – Patient disposition (CONSORT). ITT = intent-to-treat. As of 26 September 2012. *Unequivocal clinical progression is 1 or more of the following: pain requiring opiates, chemotherapy, palliative radiation therapy, decline in ECOG PS, surgical intervention. Supplemental Fig. 2 – Percent incidence of adverse events by duration of exposure and by grade. Supplemental Fig. 3 – Cumulative incidence of adverse events (all grades) from time of first incidence of adverse events.