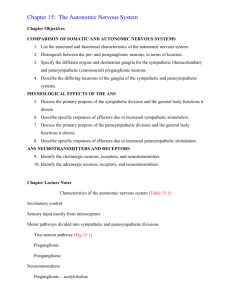
Autonomic Nervous System
advertisement

Autonomic Nervous System Autonomic nervous system (ANS) is part of the efferent division of the PNS. It is composed of visceral motor (efferent) neurons that innervate smooth muscle, cardiac muscle, glands and visceral organs. This system is involuntary; it functions below the level of consciousness. The ANS contains neurons that travel in spinal and cranial nerves. The visceral sensory neurons travel along the same pathways as the visceral motor neurons of the ANS. The visceral sensory neurons are similar to the somatic sensory neurons. I. Anatomy of the Autonomic Nervous System The efferent pathways of the ANS are composed of two neurons. The preganglionic (presynaptic) neuron has its perikaryon in the CNS. Outside of the CNS, the myelinated axon of the preganglionic neuron travels to a ganglion where this neuron synapses with the postganglionic (postsynaptic) neuron. The unmyelinated axon of the postganglionic neuron travels to the effectors. This is a two-neuron chain compared to the one neuron in the somatic nervous system, where one motor neuron travels from the CNS to the skeletal muscle innervated. The ANS is organized structurally and functionally into the sympathetic and parasympathetic divisions. A. Sympathetic or Thoracolumbar Division The perikarya of the preganglionic neurons of the sympathetic division of the ANS are located in the lateral horns of the gray matter of the spinal cord from the 1st thoracic to the 2nd lumbar segments. This division of ANS is also called the thoracolumbar division. The myelinated axons of these neurons leave the spinal cord through the ventral roots of the spinal nerves along with the somatic motor neurons. They then enter the ventral or white rami of the spinal nerves. The preganglionic neurons enter chains of interconnected ganglia. These chains are the (para) vertebral or sympathetic ganglionic chains. They are located from cervical to sacral-coccygeal region of the spinal cord on each side of the vertebral column. The preganglionc neurons are limited to spinal segments T1-L2. The spinal nerves at these segments have both white and gray rami. Postganglionic neurons in the cervical, inferior lumbar and sacral sympathetic chain ganglia are innervated by axon branches of preganglionic neurons that run up or down the sympathetic chain. The postganglionic neurons exit the sympathetic chain through the gray rami to run in the cervical, inferior lumbar and sacral spinal nerves. Thus spinal nerves T1-L2 have white rami, while all spinal nerves have gray rami. Upon entering the ganglia, the preganglionic sympathetic axons can follow one of four paths. 1. The preganglionic sympathetic axons synapse with perikarya of postganglionic neurons in the ganglion at the same level that the preganglionic neurons entered the chain. Since the postganglionic axons are unmyelinated from the ganglia to the spinal nerve the path they form is the gray rami of the spinal nerves. The axons of the postganglionic neurons then travel to the periphery in the spinal nerves. In this path, these neurons innervate smooth muscles in the blood vessels of the skin, sweat glands, the arrector pili muscles of the hair follicles and adipose tissue. 1 2. The preganglionic sympathetic axons travel up or down within the chain before they synapse with the postganglionic neurons. The ganglia in the cervical region are called the superior, middle and inferior cervical ganglia. The postganglionic neurons’ axons leaving the cervical sympathetic ganglia are in the cervical spinal nerves and in cranial nerves III (occulomotor), VII (facial), IX (glossopharyngeal) and X (vagus). The postganglionic neurons leaving these sympathetic chain ganglia above the diaphragm goes to head and thoracic organs. The postganglionic neurons leaving the sympathetic chain in the inferior lumbar and sacral-coccygeal region innervates the pelvic cavity organs. 3. The preganglionic sympathetic axons pass through the chain without synapsing. The preganglionic axons synapse with the postganglionic neurons in ganglia close to the organs they innervate, these ganglia are called prevertebral or collateral ganglia. The viscera of the abdominopelvic cavity are innervated by this kind sympathetic innervations. The preganglionic neurons’ axons form the splanchnic nerves (greater, lesser and lumbar). These preganglionic neuron’s axons pass through the sympathetic ganglionic chain to synapse with the postganglionic neurons in the celiac, superior mesenteric and inferior mesenteric ganglia. The postganglionic neurons from the celiac and superior mesenteric ganglia innervate the upper and lower digestive tract, liver, pancreas, spleen and kidney. The postganglionic neurons from the inferior mesenteric ganglion innervate the pelvic organs. 4. Preganglionic sympathetic neurons that innervate the adrenal medulla travel directly to the gland. There are no postganglionic sympathetic neurons innervating the adrenal medulla. The adrenal medulla is a modified sympathetic ganglion. The adrenal medulla cells are specialized postganglionic neurons secreting norepinephrine (NE) and epinephrine (E) directly into the blood. This is the only exception to the two-neuron chain in the ANS. 80% of the adrenal medulla secretion is E and 20% is NE. Autonomic Plexuses – are a series of nerve networks. Definition of a plexus is a network of nerves or vessels. In the thoracic, abdominal and pelvic cavities each plexus is a tangled network of sympathetic neurons, parasympathetic neurons, somatic and autonomic sensory neurons and somatic motor neurons. The plexuses named for the arteries along which they are distributed. These are the cardiac, pulmonary, celiac, superior mesenteric, inferior mesenteric, hypogastric and renal plexuses. B. Parasympathetic or Crainosacral Division The perikarya of the preganglionic neurons of the parasympathetic division are located in the brain stem and in the lateral horns of the gray matter of the sacral segments of the spinal cord. The parasympathetic preganglionic neurons, whose perikarya lie in the brain stem, travel in cranial nerves III, VII, IX and X. They synapse with the postganglionic neurons in the terminal ganglia close to structures they innervate. These neurons travel to the viscera of the head, thorax and abdomen. The parasympathetic preganglionic neurons, whose perikarya lie in the sacral region of the spinal cord, travel in the ventral roots of the sacral spinal nerves to form the pelvic splanchnic nerves. These neurons pass to terminal ganglia close to the structures they innervate to synapse with the postganglionic neurons. The postganglionic neurons then travel to the viscera of the pelvic cavity. 2 C. Anatomical Differences Between the Divisions The sympathetic and parasympathetic divisions differ in location of the perikarya of the preganglionic neurons. They also differ in lengths of their axons. In the sympathetic division the preganglionic axons are relative short and the postganglionic axons are long. The pre- and post-ganglionic axons are highly branched. This leads to wide divergence of the impulse to the visceral organs and mass activation. In the parasympathetic division, the preganglionic axons are long. The postganglionic axons are short and not as branched. Compared to the impulses in the sympathetic division, the impulses of the parasympathetic division has a more precise and focused effect. II. Functions of the Autonomic Nervous System Most visceral organs have dual innervations with the two divisions having opposite effects, one excitatory, the other inhibitory. This is possible as there are two types of neurotransmitters released at the ends of the neurons. Also for these neurotransmitters there are different types of receptors on the cells of the visceral organs. In addition, some organs have either sympathetic or parasympathetic innervations. A. ANS Neurotransmitters and Neurons 1. Cholinergic neurons - release at their ends acetylcholine. a. Parasympathetic pre- and post-ganglionic neurons. b. Sympathetic preganglionic neurons. c. A few sympathetic postganglionic neurons. d. Somatic efferent (motor) neurons to the skeletal muscle. 2. Adrenergic neurons - release at their ends norepinephrine (NE) or noradrenalin and epinephrine (E) or adrenalin. Most sympathetic postganglionic neurons secrete these neurotransmitters. Norepinephrine and epinephrine are also secreted by the adrenal medulla and have the same physiologic effect as these substances secreted by the postganglionic sympathetic neurons. 3. Effects of Parasympathetic and Sympathetic Stimulation a. Parasympathetic Stimulation The effects of parasympathetic stimulation are brief as the acetylcholine is short acting as it is inactivated by the enzyme, acetylcholine esterase (ACHE). b. Sympathetic Stimulation The effects of sympathetic stimulation is longer lasting and more widespread for three reasons: 1. Greater divergence of sympathetic pre- and post- ganglionic axons, 2. NE, E last longer than ACH but will be inactivated by enzyme, monoamine oxidase (MAO). 3. NE, E is secreted by the adrenal medulla and is distributed by way of the blood. B. Cholinergic and Adrenergic Receptors Receptors are structures on the cells in the organs of the body that can attach to the neurotransmitters. There are two types of cholinergic and adrenergic receptors and several subtypes of adrenergic receptors. 3 1. Cholinergic Receptors There are two types of cholinergic receptors that bind ACH. These receptors are named for the drug that binds to them and mimics the neurotransmitter’s activity. ACH binds to both types of receptors, but the response of the receptor on the cells to ACH is different. a. Nicotinic receptors - when nicotine binds to these receptors it produces the same effect on the cells as ACH. These receptors are on the: 1. Skeletal muscle at the nerve-muscle junction; 2. Sympathetic and parasympathetic postganglionic neurons; and 3. Cells of the adrenal medulla. The binding of ACH to nicotinic receptors is mainly excitatory on the cells of the target organs (effectors). . b. Muscarinic receptors - when muscarine binds to these receptors it produces the same effect on the cells as ACH, but opposite in effect compared to the nicotinic receptors. These receptors are on the: 1. Smooth muscle cells and glands innervated by parasympathetic postganglionic neurons; 2. Cardiac muscle cells innervated by parasympathetic postganglionic neurons; and 3. Most sweat glands innervated by cholinergic sympathetic postganglionic neurons. The binding of ACH to muscarinic receptors is either inhibitory or excitatory depending on the effect of the ACH on the cells of the target organs (effectors). For example, Inhibitory Effects - ACH binding to muscarinic receptors of cardiac muscle decreases heart rate and the force of atrial contraction. ACH binding to receptors on the smooth muscle in the sphincters in the G.I. tract relaxes the sphincters. On the other hand, Excitatory Effects - ACH binding to the receptors on the smooth muscle in the wall of the G.I. tract increases muscle activity. ACH binding to the circular smooth muscles of the iris of the eye cause constriction of the iris. ACH binding to the receptors on the cells of the sweat glands increases sweat gland activity. 2. Adrenergic Receptors There are two major types of adrenergic receptors for NE or E with subtypes. The two major types of adrenergic receptors are -and -receptors. These receptors are found on the cells in the visceral organs innervated by sympathetic postganglionic neurons. 1-receptors are excitatory. 2receptors are inhibitory. Some 1-receptors are excitatory, 2-receptors are inhibitory. NE binding to the 2-receptors on the smooth muscle cells of the blood vessels in skeletal muscle inhibits smooth muscle contraction in these blood vessels and leads to vasodilation of the blood vessels during exercise. NE binding to 2-receptors also causes vasodilation on the smooth muscle of heart blood vessels. NE stimulates -receptors more vigorously than -receptors. E stimulates both receptors equally. Depending on the organ, the cells of the target organ have either type or both types of receptors. Each organ will have one type of receptor more abundant. The receptors are distinguished by the specific response elicited by NE or E and by their selective binding of drugs that activate or block the action of the receptor. 4 For example, NE binding specifically to 1-receptors of cardiac muscle cells increases heart rate and force of contraction. NE binding specifically to 2-receptors on smooth muscle cells of the intestine reduces contractility. C. Effects of Drugs - Taking Advantage of Receptor Selectivity Many drugs either activate (agonist) or block (antagonist) or -adrenergic receptors and cholinergic receptors. In drug therapy these drugs are important in controlling the organ’s activities. However, the drugs should act without interfering with other activities of the organ or other organs. The type of receptor on which the drug acts allows a specific drug to be used to excite or inhibit the activities of the target organ. Examples: In the SNS, α1-receptors on smooth muscle cells of the blood vessels causes contraction of the smooth muscle and vasoconstriction. As an example of an agonist, phenylephrine an ingredient in cold and sinus medications is an adrenergic agonist at α1-receptors causing vasoconstriction of blood vessels in the nasal mucosa, reduces mucus production thus relieving nasal congestion. A side effect of phenylephrine is to increase blood pressure. β1-receptors on cardiac muscle cells bind to NE or E to increase rate and force of heart contraction. To block these receptors for these neurotransmitters a -blocker drug Metoprolol (Lopressor) is given. The Lopressor blocks the β1-receptors from picking up NE or E and so lowers heart rate and force and decreases blood pressure without interfering with other sympathetic effects. Its antihypertensive action blocks sympathetic impulses to the heart, but does not block sympathetic impulses to the smooth muscle of the intestine. In the PNS, constriction of the pupil of the eye is due to the circular smooth muscle of the iris contraction caused by ACH attaching to the muscarinic receptors. To dilate the pupils, atropine prevents the ACH from exerting its effect on the pupillary smooth muscles of the iris. Atropine is an anticholinergic drug that blocks the muscarinic receptors for ACH. To reverse atropine’s effect philocarpine and physostigmine are antiACHE drugs that inhibit the enzyme from breaking down ACH, thus causing pupillary constriction. III. Parasympathetic and Sympathetic Responses Many organs of the body have dual innervations. The two divisions have opposite responses which contributes to precise control of the organ’s activity and homeostasis of the body. A. Parasympathetic System In general, PNS regulates activities that conserve and restore body energy during times of rest and recovery. The parasympathetic system is an energy conservation-restorative system. It allows for food digestion and absorption to supply energy to the body cells. It allows for defecation, urination, decrease heart rate, diameter of the bronchi, diameter of the pupils, etc. The PNS reduces body function that supports physical activity. 5 B. Sympathetic System – Stress Response In general, SNS prepares the body for emergency situations. The hypothalamus activates the SNS to immediately mobilize the body‘s resources for physical activity. The sympathetic system involves the expenditure of energy. During physical or emotional stress the SNS prepares the body for “fight or flight” responses – increased heart rate and blood pressure, dilation of the bronchi, increased rate and depth of breathing, etc. The SNS constricts blood vessels to nonessential organs at this time. The activities of the nonessential organs are inhibited. However, the SNS dilates blood vessels to the skeletal muscles, cardiac muscle, to the liver and adipose tissue to release nutrients into the blood. The brain becomes more alert and skeletal muscles become active. IV. Autonomic Reflexes The autonomic reflexes regulate and control visceral organs of the body. These reflexes regulate blood pressure, heart rate, force of heart contraction, diameter of the blood vessels, motility and muscle tone of the GI tract, opening and closing of the sphincters of the digestive and urinary systems, constriction and dilation of the iris of the eye. The autonomic reflexes are below the level of consciousness. Components of an autonomic reflex 1. Receptors are interoceptors, which monitor conditions of the internal environment of the body. They respond to stimuli to trigger nerve impulses. The interoceptors are located in the blood vessels, visceral organs, skeletal muscles and in the nervous system. 2. Sensory Neuron – conducts nerve impulses from the interoceptors to the CNS. 3. Integrating Center (CNS) – For most autonomic reflexes the integrating centers are located in the hypothalamus and brain stem. Autonomic reflexes for urination and defecation have their integrating centers in the sacral region of the spinal cord. 4. Motor Neurons – Nerve impulses from the integrating centers in the CNS move along a two (2) neuron path to the effectors. The preganglionic neuron (myelinated) conducts the nerve impulses from the CNS to an autonomic ganglion. The postganglionic neuron (unmyelinated) conducts the nerve impulses from the autonomic ganglion to the effectors. 5. Effectors – smooth muscle, cardiac muscle and glands V. Control of the ANS by Higher Centers The CNS connects to the ANS and has control over it. Autonomic centers in the brain stem (medulla oblongata) and spinal cord are influenced by the hypothalamus. The hypothalamus is the major regulator of ANS activities. The hypothalamus receives sensory input from emotions, smell, taste, temperature and changes in concentration of substances in the blood. The hypothalamus output is then received by autonomic centers in the brain stem and spinal cord to control cardiovascular activity, salivation, swallowing, vomiting, urination, defecation, etc. The posterior and lateral parts of the hypothalamus control the sympathetic division, while the anterior and medial parts of the hypothalamus control the parasympathetic division. Control of the ANS by the cerebral cortex occurs during emotional stress through the limbic system. During extreme anxiety, either conscious or subconscious, the cerebral cortex through the limbic system stimulates the hypothalamus either affecting the sympathetic or parasympathetic areas of the hypothalamus. One can obtain some voluntary control of the ANS by biofeedback or by yoga. 6 7 Sympathetic Pathways 8 9