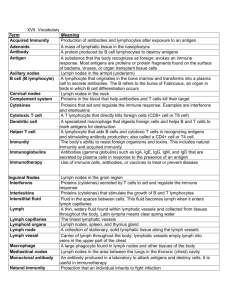
Chapter 16: LYMPHATIC SYSTEM and IMMUNITY
advertisement

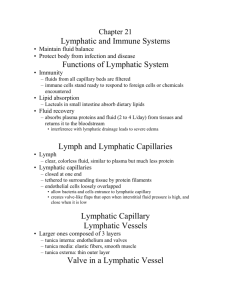
Chapter 16: LYMPHATIC SYSTEM and IMMUNITY Defined as all the cells, tissues and organs responsible for: 1) Returning fluid to the blood from body tissues a) Maintains normal blood volume and prevents tissue swelling 2) the defense of the body from infection and disease a) lymphocytes respond to pathogens, abnormal body cells, and foreign proteins 3) the distribution of hormones, fats, and waste products from their tissues of origin to the general circulation a) larger substances that are unable to enter capillaries, enter lymph vessels that drain into venous circulation Components 1) Lymph – mostly extracellular fluid; resembles plasma with lower protein concentration 2) Lymphatic vessels a) Capillaries – comprised of simple squamous epithelium (but more permeable) a) Originate as “blind pockets” and are large in diameter (as compared to blood capillaries) have thin walls and look flatter in sectional view b) Present in almost every tissue and organ except in areas that lack a blood supply as well as bone marrow and CNS c) Capillaries drain into larger vessels that lead toward the trunk d) Bulge at valves to create a beaded appearance valves – prevent back flow and direct it toward the thoracic cavity b) Major lymph collecting vessels a) Superficial (skin and membranes) and Deep (muscles and organs) vessels eventually converge to form two large collecting ducts Named for their location (mammary, femoral, etc) (1) Thoracic duct (left lymphatic duct) ~16 inches long (a) anterior to the level of vertebrae L2 up to the level of the left clavicle (b) receives lymph from left side of head, neck and thorax and entire body inferior to the diaphragm (i) Cisterna chyli – a receiving pouch at the inferior end of this duct (c) empties into left subclavian vein (2) Right lymphatic duct (short duct) (a) Lies below the right clavicle (b) receives lymph from delivering lymph from the right side of the body superior to the diaphragm c) Lymph is moved through the vessels in the same manner as blood through veins a) Rhythmic contractions, valves, skeletal muscle contractions, and the respiratory pump keep lymph flowing back towards the heart b) The more lymph, the more contractions and pressure to return Lymphedema (Box 16-1) Edema is tissue swelling due to excess fluid in the tissue. Blockage of lymphatic tissue due to infection (filarial worms) will prevent fluid drainage from tissue. Limbs will become grossly distended, a condition known as elephantiasis. Other blockages can come from loss of lymphatic tissue, malignant growths that block vessels, or other infections. Edema may increase the chance of infection because filtering is diminished and protective measures are diluted. 3) Lymphoid tissue a) Lymph nodes (kidney shaped) – locations (cervical, axillary, mesenteric, inguinal) a) Range in diameter from 1-25mm b) Collagen fibers surround and extend into the node (trabeculae) which is dominated by immune cells c) Blood vessels and nerves attach at the hilus (indentation) (1) afferent vessels – carry lymph to lymph node (2) efferent vessels – carry lymph to venus circulation out the hilus d) 99% of the lymph that passes through the node is cleared of its antigens (outer cortex to medulla) e) Designed as an early warning system (infection presents antigens) b) Spleen a) Contains the largest collection of lymphoid tissue in the body b) takes it shape by the organs that are around it (5-7” long. 2-3” wide) c) contains pulp red (RBC’s) vs white pulp (lymphoid nodules) d) Main functions: (1) Removes abnormal blood cells and other components by filtration and phagocytosis. Initiates an immune response (T-cells and B-cells) (2) storage of iron from recycled RBCs (3) Produces RBCs before birth (4) Blood reservoir which can be used during hemorrhage Surgical removal of the spleen (splenectomy) when damaged is well tolerated. The capsule around the spleen is too thin to repair. There are plenty other lymphatic tissues to do the job. c) Thymus a) located in the mediastinum (pink and grainy) posterior to the sternum b) grows through puberty then diminishes in size and becomes fibrous (involution) c) divided into lobules where each has an outer cortex and central medulla d) T cells mature in the cortex then migrate to the medulla to be released e) releases hormones collectively known as thymosins d) Tonsils a) large nodules in the walls of the pharynx b) R & L palatine tonsils located on the soft palate (referred to as “tonsils”) c) Pharyngeal tonsil (adenoids) located on the roof of the pharynx d) Lingual tonsils - pair at the base of the tongue (1) Not noticeable unless swollen Tonsillitis (Box 16-3): bacterial infection of the tonsils in the throat Breathing and swallowing become difficult Once an abscess forms, surgery is required to drain the fluid Removal of tonsils (tonsillectomy) to prevent reoccurring infection e) Other tissues that are dominated by lymphocytes a) MALT (mucosa-associated lymphoid tissue) (a) clusters of lymphoid nodules linked to the digestive system (b) Peyer’s patches exist within the mucous membrane of GI tract b) Appendix (7-10 cm long) (1) Slender tube of lymphatic tissue attached to the cecum of the large intestine Appendicitis: breakdown of the epithelial lining of the appendix which creates inflammation. The organ becomes distended and may rupture Toxins and bacteria are released into the peritoneal cavity Disorders of the Lymphatic Tissue Lymphangitis is the inflammation of a lymphatic vessel which creates red streaks along the skin in the area of the infection. Shows the spread of bacteria in the lymphatic system. If lymph system isn’t able to stop the infection, it will get into the bloodstream and cause septicemia (blood poisoning) Lymphocytes that have become cancerous that exist in lymph tissue are called lymphomas 40% of these cases are considered Hodgkin’s Disease, the rest are grouped as nonHodgkin’s lymphoma a) cause unknown, but linked to infections and in more common in males than females b) again early diagnosis and treatment is the key to successful prognosis, but unfortunately most are not detected early because it mimics more traditional “every day” diseases Epstein-Barr virus (EBV) causes a chronic infection that is known as Mononucleosis (Increases monocyte production) Transmitted orally (kissing disease) Virus invades the lungs, bone marrow, and lymphoid tissue causing fever, sore throat, enlarged spleen, and other lymphadenopathies (disease of lymph nodes) Can only treat symptoms; no defense against the virus; cautionary to damaging the spleen Nonspecific vs Specific Defenses Immune response or immunity the ability to resist infection and disease through the activation of specific defenses Why do infections occur? (portal of entry, virulence of an organism, dose of pathogens, and an individual’s predisposition) Nonspecific Defenses 1) Physical Barriers a) the skin provides the first outer defense against antigens/pathogens from entering the body b) epithelial tissue with hair, mucous, sebaceous and sweat glands (pH and enzymes) 2) Phagocytes (white blood cells) a) Police and clean up cellular debris in response to an invasion usually before lymphocytes detect their presence b) Microphages a) Neutrophils and eosinophils that circulate in the blood b) Leave the blood and enter peripheral tissue subjected to injury or infection c) Macrophages a) Large phagocytic cells that are fixed or move freely b) Fixed macrophages: are permanent residents of specific tissues and organs, incapable of movement, scattered within the connective tissue of organs c) Free macrophages: travel throughout the body and migrate to damaged or infected tissue 3) Immunological Surveillance a) Monitoring of normal tissues by NK cells b) NK cells recognize abnormal cells by detecting the antigens on it’s surface c) Immunological escape a) When cancer cells lack or cover antigens, or destroy NK cells that detect them 4) Inflammation: localized tissue response to injury a) most cells release chemicals into the local environment (histamine increase blood flow and capillary permeability) a) increase blood flow, increase temperature, increase enzyme activity b) clotting factors begin to form a clot around the general area c) neutrophils in the area move to the damaged area releasing chemicals that attract other neurophils and macrophages d) macrophages engulf pathogens and continue to attract other macrophages e) some cytokines released by the mast cells start to stimulate local sensory neurons to elicit pain f) this general response allows for specific defenses to be activated 5) Fever: a) maintenance of a body temperature greater than 99 degrees Fahrenheit b) pyrogen- proteins that reset the thermostat in the hypothatlmus c) interleukin –1: increase 1 degree Celsius in body temperature increase metabolism 10% 6) Interferons (“interferes” with multiplication and spread of the virus) a) Small proteins released by activated lymphocytes and macrophages (cytokines) b) Binds to surface receptors on cell and releases antiviral proteins (don’t destroy but interfere with replication) c) Stimulate activities of macrophages and NK cells d) Named with a Greek letter to indicate different categories Lymphocytes – 20-30% of the circulating white blood cells a) T-cells (thymus dependant cells) 80% of lymphocytes a) Cytoxic T cells- directly attacks foreign cells or body cells infected by viruses (cellular immunity) Responsible for rejection of skin grafts and transplants b) Helper T cells- stimulate the activation and function of both T cells (secrete interleukins) and plasma B cells (secrete antibodies) c) Suppressor T cells- inhibit the activation and function of both T cells and B cells d) Memory T cells – stay in reserve for subsequent attacks b) B cells (bone marrow derived) – 10-15% of lymphocytes a) Responsible for the production and secretion of antibodies (immunoglobulins)soluble proteins (read Box 17-1) b) Immunoglobulins bind to specific chemical targets called antigens (pathogens) (foreign material) c) NK cells (Natural Killer) – 5-10% of lymphocytes a) large granular lymphocytes that “police” body tissues b) attack foreign cells, infected cells, and cancer cells within normal tissue d) Lymphocytes circulate through the body at different rates and exist in the body at different rates a) Most have long life spans (20+ years) Lymphopoiesis a) lymphocyte production involving bone marrow, thymus, and peripheral lymphoid tissue b) two distinct populations of lymphoid tissue are produced in the bone marrow a) B-cells mature in the bone marrow. NK cells develop in the bone marrow enter the bloodstream and mature in the blood stream. b) the other group of cells migrates to the thymus (1) there they are isolated from general circulation (blood-thymus barrier) and divide producing the different types of T-cells (2) after they have developed they reenter the blood stream and take on specific roles. All lymphocytes have the ability to divide by mitosis. An important concept for the immune response. Specific Defenses (immunity) Inborn immunity - immunity we have at birth. No relationship to previous exposure passed along within genetic lines (species immunity or individual immunity) Acquired Immunity (active) - immunity to a specific antigen after you have been exposed Naturally active – contact with a specific disease Passive immunity – transfer of antibodies from an other source (placenta/mother’s milk or induced) Artificially acquired (vaccination or immunization) 1. live, dead, or attenuated vaccines 2. toxoids Boosters (table 17-2) Research Examples of Bacterial and Viral Vaccines Cell Mediated Immunity 1) Activated T-cells mount a direct attack on foreign or infected cells 2) Completed by cytoxic T cells, memory T cells, Helper T cells a) Antigen Presentation occurs when an antigen-glycoprotein combination capable of activating T cells appears on a cell membrane (ie. Virus infected cell) Antibody-mediated immunity (Humoral immunity) 1) Activated B cells differentiate into Plasma cells which secrete a specific antibody that attacks specific antigens a) activated by a specific antigen presentation or interleukins secreted by helper T cells b) divide numerous times to create plasma cells or Memory B cells Cells that are not activated after cell division; stay in reserve Primary and Secondary Responses 1) Primary response – Helper T cell activation which stimulates B cells which result in antibody production (lag time between activation and sufficient production) 2) Secondary Response – upon second exposure to the same antigen, b cells immediately begin synthesizing antibodies in massive quantities Immune Disorders With advancing age, the immune system becomes less effective. Vaccines are strongly recommended Physical examination includes observing or palpating for Lymphadenopathies, percussion of the spleen, observation of skin disorder linked to certain infections, and experiencing weakness and fatigue. Disorders of the immune system may result from an inadequate or suppressed immune response, an excessive immune response, or an inappropriate mechanism of the immune response. 1) AIDS (late stage HIV disease) a) Retrovirus (Box 17-3) that injects RNA into healthy cell (typically Helper T cells) which ultimately decreases the cell population b) Without T cells, the body’s immune defense against other pathogens is greatly reduced c) Current chemotherapies are extending the lifespan of individuals by supporting immune defenses along with maintaining healthy lifestyles 2) Immunosuppressant drugs (radiation and some chemotherapy) destroy stem cells and lymphocytes leading to complete suppression of immunity a) Bone marrow transplants, if not rejected, begin creating new RBCs and WBCs within two weeks b) Graft rejections are reduced by matching lymphocytes and administering immunosuppressant drugs 3) Allergies – excessive immune responses a) Certain antigens create an excessive T cell response that in turn produces plasma antibody production that attacks normal cells as well as the antigen b) Allergens are antigens that trigger allergic reactions c) The most common type of allergy is immediate hypersensitivity (allergic rhinitis – hay fever) a) Starts first with sensitization (1) The first exposure doesn’t create the symptoms, but antibody production occurs which attach to basophils and mast cells so that a second exposure will create a massive inflammation in the surrounding tissue. (a) Lethal if the reaction happen systemically Anaphylaxis – a circulating allergen affects mast cells throughout the body 1) The response can occur in a few minutes 2) Swelling and edema in the dermis and respiratory constriction occurs with possible vasodilation which will decrease venous return and lower blood pressure (faint) a) Anaphylactic shock b) Anihistamines required, in some cases epinephrine and corticosteroids are required as well Stress and the immune response (Box 17-2) o Depression of the inflammatory response o Reduction in the number and activity of phagocytes in peripheral tissue o Inhibition if interleukin secretion