Chen, Melissa
advertisement

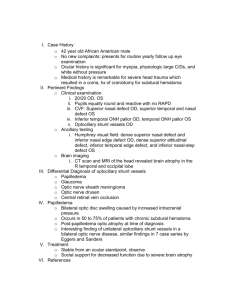
Melissa Chen melissachenod@gmail.com VA Boston – Jamaica Plains Abstract: An unusual case of a 41 year old male presents with bilateral asymmetrical optociliary shunt vessels accompanied by bilateral disc pallor and moderate cupping. The possible underlying causes for this condition will be investigated. I. Case History: a. Patient demographics b. Chief complaint c. 41 year old Caucasian male KR presented to the Optometry clinic as a new patient consult secondary to moderate cupping and atypical vessels OU. Patient is otherwise asymptomatic. Ocular, medical history Ocular history: Refractive error (CMA); history of non-specified ocular trauma OS at age 6 without sequelae. Medical history: 1. Crohn’s Disease (Dx 1992) s/p colostomy with ileostomy (2003); 2. Obesity; 3. hyperlipidemia; d. 4. GERD (Gastroesophygeal Reflux Disease) 5. Diabetes mellitus (diagnosed during work up with Hba1c at 7.0 on 8/21/08 to7.6 on 1/21/2009). Medications Omeprazole 20 mg Drainable pouch (for ileostomy status) History of taking systemic prednisone for 10 years for Crohn’s disease. II. Pertinent findings: a. Clinical/Physical BVA: 20/20 OD, 20/20-2 to 20/30 OS (fluctuation) Confrontations: FULL OU Pupils: ERRL questionable left APD Versions: FULL OU Amsler: OD normal; OS focal area of scotoma inferior to fixation dot Red Cap: 100% OD, 75% OS Ishihara: 6/6 OD, 0/6 OS Slit Lamp Exam: within normal limits OU Tonometry: 17mmHg OD, 20 mmHg OS (Goldmann) Gonioscopy: open to ciliary body 360 with minimal pigment OU Exophthalmometry: OD 17mm OS 16mm base of 110 Pachymetry: 575OD, 583 OS Dilated Fundus Exam: Optic Nerve Head: OD 0.6V/0.65H, distinct borders, optociliary shunt vessels nasally and possibly temporally; Grade 1 pallor OS 0.65H/V with inferior temporal thinning, distinct borders, numerous optociliary shunt vessels superior nasally and most of temporal rim; Grade 2 pallor Vessels: A/V crossing changes OU Macula: Clear OU Periphery: unremarkable OD, vitreoretinal tuft inferior temporally OS b. Laboratory studies CBC w/diff – essentially within normal limits, slightly elevated WBC of 12.5 (range 4.511.0) ESR – 19 (range 0-15) – High side of normal but patient has history of Crohn’s disease CRP – 7.64 (range 0-7.43) – Slightly elevated but patient has history of Crohn’s disease FTA and RPR – non-reactive c. Hb-A1c – 7.0 Lyme Ab – negative T4, TSH, T3 – all within normal limits Radiology studies d. MRI of orbit and brain (with and without contrast) with thin slices through the chiasm and orbit– normal findings, did not show any evidence of mass or other orbital or intracranial lesions. Others Fundus photography taken HRT (8/18/08): OD – wnl OS – nasal, temporal, and inferior/nasal thinning HVF 24-2: OD – questionable early superior nasal step OS – paracentral defects (absolute scotoma inferonasal from fixation) with scattered defects and enlarged blindspot. Fluorescein Angiography(FA) – Optociliary shunt OS>OD with no evidence of leakage. Retina otherwise is unremarkable and shows no clear cut evidence of prior incidence of CRVO. III. Differential diagnosis k. Primary/leading Patient presents with bilateral asymmetrical optociliary shunt vessels. The differential diagnosis of the underlying etiology includes: 1. Optic nerve sheath meningioma: Ruled out by negative MRI of brain and orbit. 2. Intracranial mass Ruled out by negative MRI of brain and orbit. 3. Glaucoma (Refer to discussion) 4. Diabetes Mellitus (Refer to discussion) 5. Congenital Optociliary Shunt Vessels (Refer to discussion) 6. History of Papilledema o 7. History of bilateral central retinal vein occlusions o 8. Clinical exam did not show characteristics of resolved papilledema such as disc elevation, drusen-like crystalline deposits, or severely impaired vision. Our patient shows disc pallor with moderate cupping rather than disc pallor with mild residual elevation (common in resolved papilledema). The chance of a bilateral CRVO is unlikely in a young male and the FA was not conclusive. There is a localized area of a few mildly tortuous vessels superior nasal to the fovea OD which is insufficient to support a previous episode of CRVO. Optic disc drusen o 9. Clinical Exam did not show any evidence of disc drusen OU. Idiopathic Intracranial Hypertension o Patient is mildly obese but denies postural headaches and no prior history of headaches 10. Thyroid Optic Neuropathy o T3, T4 and TSH lab work was all within normal limits and MRI did not show enlarged extraocular muscles. 11. Optic nerve arachnoid cyst o IV. Was not evident on the MRI Diagnosis and discussion m. Elaborate on the condition/Expound on unique features Optociliary shunt vessels are venous collaterals that are formed between the retinal veins and the peripapillary choroidal vein in the prelaminar portion of the optic nerve. This vessel formation is a non-specific indication of an underlying compression of the central retinal vein within the optic nerve. For this specific case, there are a number of possible etiologies and some of them were ruled out above. As a result, the top differentials include: glaucoma, diabetes mellitus, or congenital optociliary shunt vessels. Glaucoma with chronic elevated IOP can cause optociliary shunt vessel formation. Our patient does have a history of 10 year duration of taking systemic prednisone for Crohn’s disease and he did not receive any eye care during this 10 year period. It remains a possibility that he may have developed steroid induced elevated IOP with subsequent development of optociliary shunts and glaucomatous optic neuropathy (with cupping and pallor). Pt has had colostomy with ileostomy in 2003 with discontinuation of prednisone. Upon examination in our clinic on 8/2008, patient’s IOP may have been stabilized but the glaucomatous damage as well as the optociliary shunt vessels remains evidenced. Furthermore, in an article called “Optociliary Shunt Vessels in Diabetes Mellitus,” by JJ LEE, three cases were discussed where diabetes was the cause of optociliary shunt formation. The proposed theory is that diabetes causes small vessel disease and venous stasis, which causes the venous circulation to become compromised (Lee). In this case, KP was not diagnosed with diabetes until blood work up was ordered to rule out causes for optociliary shunt formation. As a result, diabetes as the etiology of KP’s optociliary shunt vessel formation cannot be rule out. Lastly, congenital optociliary shunt vessels should also be considered as a possible cause for KP’s condition. In the “Clincial Studies on the Occurrence and the Pathogenesis of Optociliary Veins” article by Yoshimasa Masuyama, they presented a case where the patient had the congenital form. In the article, they discussed how congenital shunt vessels are rare and how they appear less tortuous and lighter in color in comparison to the acquired type (Masuyama). In this specific case, KP had an APD which decreases the likeliness of the congenital form but since there were no previous fundus photos for KP, a definite answer could not be made. n. V. Expound on unique features Bilateral Optociliary Shunt Vessels Negative orbital and intracranial MRI Relatively normal retina Treatment, management o. Treatment and response to treatment Close monitoring for any changes or progression: repeat HVF, periodic MRI for comparison, repeat photos, HRT, OCT. IOP control for glaucoma p. Work closely with the primary care provider to control diabetes, weight, and lipid levels. Bibliography, literature review encouraged Abbasian J, Lee AG, Longmuir R, Rouleau J. “Rapid Regression of Retinochoroidal Venous Collaterals Following Optic Nerve Sheath Fenestration in Idiopathic Intracranial Hypertension.” Semin Opthalmol. 2007 Jan-Mar;22(1):35-7. Boschetti NV, Smith JL, Osher RH, Gass JD, Norton EW. “Flourescein Angiography of Optociliary Shunt Vessels.” J Clin Neuroophthalmol. 1981 Mar;1(1):9-30. Eggers HM, Sanders MD. “Acquired Optociliary Shunt Vessels in Papilloedema.” Br J Ophthalmol. 1980 Apr;64(4):267-71. Lee JJ, Yap EY. “Optociliary Shunt Vessels in Diabetes Mellitus.” Singapore Med J. 2004 Apr;45(4):166-9. Masuyama Y, Kodama Y, Matsuura Y, Sawada A, Harada K, Tsuchiya T. “Clinical Studies on the Occurrence and the Pathogenesis of Optociliary Veins.” J Clin Neuroophthalmol. 1990 Mar;10(1):1-8. Saeed P, Rootman J, Nugent RA, White VA, Mackenzie IR, Koornneef L. “Optic Nerve Sheath Meningioma.” Ophthalmology. 2003 Oct;110(10):2019-30. VI. Conclusion q. Clinical pearls, take away points if indicated This unusual case of bilateral optociliary shunts highlights the diagnostic challenges in uncovering the underlying etiology. This case also emphasizes the importance of methodological investigation, close monitoring for progression, and appropriate management.