Pathophysiology & Incidence
advertisement
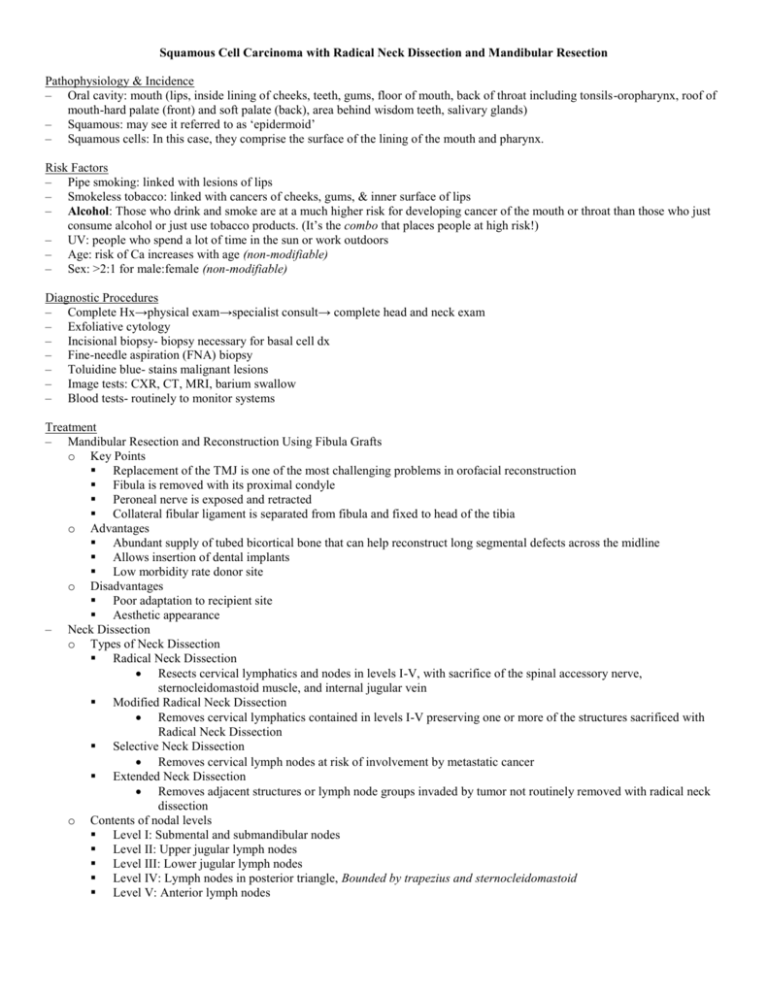
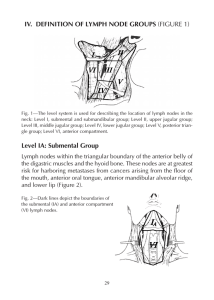
Squamous Cell Carcinoma with Radical Neck Dissection and Mandibular Resection Pathophysiology & Incidence – Oral cavity: mouth (lips, inside lining of cheeks, teeth, gums, floor of mouth, back of throat including tonsils-oropharynx, roof of mouth-hard palate (front) and soft palate (back), area behind wisdom teeth, salivary glands) – Squamous: may see it referred to as ‘epidermoid’ – Squamous cells: In this case, they comprise the surface of the lining of the mouth and pharynx. Risk Factors – Pipe smoking: linked with lesions of lips – Smokeless tobacco: linked with cancers of cheeks, gums, & inner surface of lips – Alcohol: Those who drink and smoke are at a much higher risk for developing cancer of the mouth or throat than those who just consume alcohol or just use tobacco products. (It’s the combo that places people at high risk!) – UV: people who spend a lot of time in the sun or work outdoors – Age: risk of Ca increases with age (non-modifiable) – Sex: >2:1 for male:female (non-modifiable) Diagnostic Procedures – Complete Hx→physical exam→specialist consult→ complete head and neck exam – Exfoliative cytology – Incisional biopsy- biopsy necessary for basal cell dx – Fine-needle aspiration (FNA) biopsy – Toluidine blue- stains malignant lesions – Image tests: CXR, CT, MRI, barium swallow – Blood tests- routinely to monitor systems Treatment – Mandibular Resection and Reconstruction Using Fibula Grafts o Key Points Replacement of the TMJ is one of the most challenging problems in orofacial reconstruction Fibula is removed with its proximal condyle Peroneal nerve is exposed and retracted Collateral fibular ligament is separated from fibula and fixed to head of the tibia o Advantages Abundant supply of tubed bicortical bone that can help reconstruct long segmental defects across the midline Allows insertion of dental implants Low morbidity rate donor site o Disadvantages Poor adaptation to recipient site Aesthetic appearance – Neck Dissection o Types of Neck Dissection Radical Neck Dissection Resects cervical lymphatics and nodes in levels I-V, with sacrifice of the spinal accessory nerve, sternocleidomastoid muscle, and internal jugular vein Modified Radical Neck Dissection Removes cervical lymphatics contained in levels I-V preserving one or more of the structures sacrificed with Radical Neck Dissection Selective Neck Dissection Removes cervical lymph nodes at risk of involvement by metastatic cancer Extended Neck Dissection Removes adjacent structures or lymph node groups invaded by tumor not routinely removed with radical neck dissection o Contents of nodal levels Level I: Submental and submandibular nodes Level II: Upper jugular lymph nodes Level III: Lower jugular lymph nodes Level IV: Lymph nodes in posterior triangle, Bounded by trapezius and sternocleidomastoid Level V: Anterior lymph nodes o – Complications of Neck Dissection Perioperative: Hemorrhage, Shock, Airway obstruction, Carotid sinus reflex, Pneumothorax, Air embolism, Peripheral motor nerve damage, Peripheral sensory nerve damage, Subcutaneous emphysema, Injury to cervical spine Postoperative: Delayed bleeding, Wound infection, Fistula, Chylus fistula, Necrosis of flap tissue, Rupture of carotid artery, Fluid and electrolyte imbalance, Increased ICP, Parotid gland complications, Pulmonary complications, Clavicular fracture Radiation Therapy o > 6000 cGy is recommended o Indications o Lips are the most common metastatic site – Chemotherapy o Adaptation of common chemotherapy o Lower concentrations o Common drugs o Use with laser treatment Management of Shoulder Dysfunction after Neck Dissection Spinal accessory nerve palsy leads to dysfunction of the trapezius which can be a painful and disabling condition. The shoulder droops as the scapula is displaced laterally and rotated downward. Patients present with an asymmetric neckline, a drooping shoulder, winging of the scapula, and weakness of active elevation. – Surgical Options o Levator scapulae, rhomboid major and rhomobid minor transfer (Bigliani et al) Following radical neck dissection and spinal accessory nerve resection, these intact and innervated muscles may be repositioned to function where the trapezius cannot o Cable grafting of great auricular nerve (Weisberger et al) This procedure “reconstructs” the spinal accessory nerve (sacrificed in radical neck dissection) with the great auricular nerve – Exercise (Herring et al, Saunders et al, Laska et al) o Pendulum exercises o Wall climbing o wall slides o Wand exercises o Shoulder sling o cervical and scapular PNF o Isokinetic dynamometry o NMES o shoulder abd/flex o Resisted shoulder elevation o McConnell taping o shoulder shrugs o Scapular retraction o Shoulder AAROM o lower trap Laska T, Hannig K. Physical therapy for spinal accessory nerve injury complicated by adhesive capsulitis. Phys Ther. 2001;81:936-944. Additional PT interventions – Massage o Scar management: cross-friction/deep friction: slow, firm manner 5-10 min. 3-6x/day. o Edema/Lymphedema: to decongest lymphatics; ↑’s lymph contractility, circulation, & ↓’s fibrotic tissue, duration & frequency will vary for each case o Over radiation site: Early- caution 2° ↓’d skin integrity; not recommended; later: tx of subcutaneous fibrosis, edema, adhesions. – Hyperbaric oxygen – Postural exercises – Cervical ROM Psycho-social Issues – Guilt, blame oneself: Pts with oral cancers often feel they have brought it on themselves due to their lifestyle choices (smoking, chewing tobacco, drinking, etc) – Fear, confusion, helplessness: Fear of the unknown, confusion as to what to do or why this happened to them, not in control – Anxiety, fatigue, depression: Vicious cycle – Embarrassed, nervous, ashamed: Dramatic change in appearance (new advances in plastic surgery lessen this affect); feeling attractive to one’s spouse; Will people be afraid of the way I look? – Worry about job/cost: If the pt has a job, can they keep it; what will happen if they can’t; insurance coverage?; financial burden – Even with no recurrences, people who have had cancer learn to live with uncertainty. – Studies show that for a person newly diagnoses with cancer, quality of life decreases for the first few months, but within one year, patients feel reasonably well and happy. – It is becoming more common for doctors to recommend their pts seek support or therapy. o Better outcomes are associated with higher levels of support Group meetings Family support Faith Counseling/therapy