SUPPLEMENTARY MATERIAL
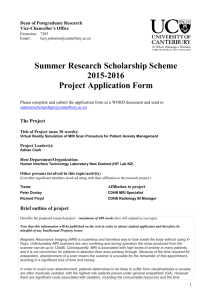
advertisement

SUPPLEMENTARY MATERIAL Case 1. A 60-years-old woman presented at age 57 complaining of increased severity and frequency of headaches. She had been suffering from headache for many years, but in the past 2 years they had become daily, continuous, with a clear orthostatic component. An MRI obtained at another institution was interpreted as demonstrating a malformation of posterior fossa structures. On admission to our Institute (May 2005), additional complaints were profound weakness, difficulty swallowing liquids, dizziness, hearing distortion and neck pain. Neurological examination demonstrated psychomotor slowing, frontal signs, dysphagia for liquids, ataxia. MRI showed diencephalo-mesencephalic swelling with brain sagging; descent of the iter to the aqueduct below the incisural line was 20 mm; descent of cerebellar tonsils below Chamberlain’s line: 15 mm. No subdural haematomas were found. Thin dural enhancement over the convexities and along the clivus was present. Pituitary gland enlargement, consistent with hyperemia, was present. MRI of the spine showed numerous dilated perineural cysts along the spinal roots, no CSF extradural collections, and mild engorgement of the spinal venous plexuses. Diagnosis of SIH was made and an epidural blood patch was performed. Improvement ensued in less than 72 hours: headache and slowing of speech disappeared, ataxia and dysphagia greatly improved. Brain MRI abnormalities were reduced at 2-month control and further improvement was observed at 8 months. Case 2. A 56-year-old woman had been complaining of continuous headache exacerbated by orthostatism, dizziness, and pain along the spine for 10 months. An MRI had allegedly demonstrated a posterior fossa malformation. She was admitted to our Institute because nausea and vomiting aggravated her clinical condition; headache was no longer relieved by horizontal decubitus. On admission, she was drowsy, slow in speech and mentation, and appeared profoundly weak. MRI showed diencephalo-mesencephalic swelling with brain sagging; descent of the iter to the aqueduct: 22 mm; descent of cerebellar tonsils below Chamberlain’s line: 5 mm. No subdural 1 collections. On postcontrast study, no dural enhancement was present except, thin, along the clivus. Large dural venous sinuses and enlarged pituitary gland were also seen. On spinal examination, engorged peridural venous plexuses, no extradural CSF collections and an irregularly dilated dural sleeve at T1-T2 on the left side were found. The patient underwent surgical ligature and covering of the left T1 root with excellent clinical result and return to normal conditions for 3 months. Brain MRI obtained 2 months after operation, however, did not show substantial changes. One month after recurrence of clinical deterioration, the patient had a lumbar blood patch, followed by immediate clinical improvement which lasted 4 months. After this period, gradual recurrence of clinical symptoms occurred and 6 months later the patient was submitted to another blood patch (May 2006), whose beneficial effects are still present after 6 months, in spite of no significant improvement of the brain sagging and swelling on MRI. Case 3. A 60-year-old woman had been suffering from headaches for years. At the end of 2004, the headaches changed pattern, becoming nearly continuous and more severe, with a distinct orthostatic pattern: elevation of the head caused headache in less than 15 minutes. Profound weakness, episodes of urinary incontinence, dizziness and double vision were additional complaints. A few months later, she was submitted to MRI and diagnosed to have SIH. On admission to our Institute in November 2005, the patient was profoundly weak and emotionally unstable. Urinary incontinence was present. Neurological examination showed frontal signs, left 6th nerve palsy, ataxia, positive Romberg sign. MRI showed diencephalo-mesencephalic swelling with brain sagging; descent of the iter to the aqueduct: 22 mm; descent of cerebellar tonsils below Chamberlain’s line: 5 mm. No subdural collections and no obvious venous engorgement were present. Minimal dural enhancement was found on postcontrast examination. On spinal MRI, periradicular cysts at nearly all levels with a Christmas tree-like aspect were demonstrated. Epidural blood patch led to a complete clinical recovery for 5 months. Worsening with headache, weakness 2 and incontinence was again relieved by repeated blood patch. Improvement was maintained at last follow-up, 2 months after the second blood patch. Case 4. A 42-year-old man had onset of posterior pulsating headache that rapidly became clearly orthostatic in December 2005. His neurological examination was normal when, 3 months later, he had an MRI that showed very thin subdural collections and diencephalo-mesencephalic swelling with brain sagging; descent of the iter to the aqueduct: 19 mm; no descent of cerebellar tonsils below Chamberlain’s line. Dural enhancement over the convexities and along the clivus were present. Spinal MRI showed dilatation of venous plexuses and a thin anterior extradural CSF collection from C6 to T3. No suspected points of CSF leakage were found. The patient, who has been treated with bed rest, hydration and steroids with good clinical improvement, is currently in follow-up. Case 5. This 63-year-old woman had onset of orthostatic headache in 2001, 5 years prior to admission at our Institute, shortly after a mild head trauma. She became depressed, then developed mild disequilibrium, hearing changes and periods of somnolence and was submitted to a series of examinations receiving different diagnoses. MRI examinations demonstrated posterior fossa abnormalities with a midbrain deformity, which were interpreted as a possible midbrain tumour, and subsequently a brainstem malformation, and a Chiari 1 malformation. In 2003, on admission to another hospital, she was found depressed, with remarkable slowing in cognitive and motor performances, and ataxic. On MRI, a severe brain sagging at the tentorial incisura was described, with very thin third ventricle, elongation of the anteroposterior diameter of the midbrain with posterior dislocation of the tectum and obliteration of the anterior mesencephalic and pontine cisterns. The tonsils were at the level of the foramen magnum. The findings were still considered indicative of a malformative aspect of the brainstem. In 2004, a minimal dural enhancement was noted and diagnosis of SIH was suggested. Extensive search for a CSF leakage, including 3 radioisotope myelocisternogram, was negative. The patient improved after bed rest and hydration and nothing else was done. The patient slowly developed parkinsonian features treated with levodopa with some improvement. She also complained of urinary urgency with occasional incontinence. In July 2006, the patient was again admitted to another hospital because of reappearance of orthostatic headache, mild ataxia, dysarthria, and tremor in the right hand. Diagnosis of malformation was again considered. The patient had some subjective and objective improvement without treatment except for bed rest and was discharged home. In October 2006 she presented at our Institute with the same clinical picture; MRI demonstrated severe brain sagging with deep BS. Descent of the iter to the aqueduct below the incisural line was 19 mm. The cerebellar tonsils were not herniated. No subdural effusions were present but large sulci and subarachnoid spaces along the convexities could be seen. Further examinations to search for the dural leakage have been proposed in order to proceed with adequate treatment, but so far the patient has postponed additional investigations and treatment. 4