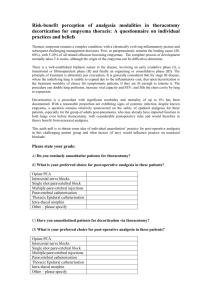
THORACIC PARAVERTEBRAL BLOCK
advertisement

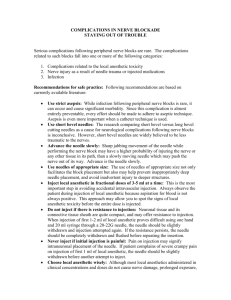
THORACIC PARAVERTEBRAL BLOCK THORACIC paravertebral block (TPVB) is the technique of injecting local anesthetic adjacent to the thoracic vertebra close to where the spinal nerves emerge from the intervertebral foramina. This results in ipsilateral somatic and sympathetic nerve blockade in multiple contiguous thoracic dermatomes above and below the site of injection. Indications: TPBV offers several technical and clinical advantages and is indicated for anesthesia and analgesia when the afferent pain input is predominantly unilateral from the chest and/or abdomen. Bilateral TPVB has also been used perioperatively during thoracic, major abdominal vascular, and breast surgeries. Common indications are: POSTOPERATIVE ANALGESIA: Thoracic surgery Breast surgery Cholecystectomy Renal and ureteric surgery Herniorrhaphy Appendectomy Video-assisted thoracoscopic surgery SURGICAL ANESTHESIA: Breast surgery Herniorrhaphy Chest wound exploration MISCELLANEOUS Fractured ribs Therapeutic control of hyperhydrosis Liver capsule pain after blunt trauma Acute postherpetic neuralgia Technical advantages:: Simple and easy to learn Safer and easier than thoracic epidural Palpation of rib not necessary and scapula does not interfere with block Safe to perform in sedated and ventilated patients Catheter placement under direct vision during thoracic surgery is safe and accurate Chest drain loss of local anesthetic is four times lower than that of interpleural block Clinical advantages: Single injection produces multidermatomal ipsilateral somatic and sympathetic nerve block Maintains hemodynamic stability Reduces opioid requirements Low incidence of complications Preserves bladder sensation Preserves lower limb motor power Promotes early mobilization Anatomy: The TPVS is a wedge-shaped space that lies on either side of the vertebral column. Its anatomic features are as follows: BOUNDARIES: Anterior/lateral: Parietal pleura Posterior: Superior costo-transverse ligament Medial: Postero-lateral aspect of the vertebral body, intervertebral disc and the intervertebral foramen COMMUNICATIONS: Intercostal space laterally Epidural space medially Paravertebral space on the other side via the prevertebral and epidural space. CONTENTS: TPVS contains fatty tissue, within which lies the intercostal (spinal) nerve, the dorsal ramus, the intercostal vessels, the rami communicantes, and, anteriorly, the sympathetic chain. The spinal nerves in the TPVS are devoid of a fascial sheath, which makes them exceptionally susceptible to local anesthetic. Technique: Patient position: Sitting, lateral, or prone. The sitting position allows easy identification of landmarks, and the patients are often more comfortable. Equipment: 10 cm, 18-22 g. short bevel spinal or epidural needle. Needle Insertion Point: 2.5 cm lateral to the tip of spinous process. Saggital section through the thoracic paravertebral space showing a needle that has been advanced above the transverse process. Procedure: Insert needle (attached to tubing or syringe) perpendicular to the skin to contact transverse process at 2-4 cm depth. Then walk off the superior or inferior aspect of the transverse process, until ‘pop’/loss of resistance to saline or air. Loss of resistance is subjective and indefinite. The needle may be advanced a fixed distance (1-2 cm) without eliciting loss of resistance – very effective and low risk of complications. Limit insertion to < 2 cm past the transverse process. It is imperative to locate the transverse process before advancing the needle any further to prevent inadvertent deep insertion and possible pleural puncture. Difficulty is common during catheter insertion, and may require manipulation of needle. Very easy passage may indicate interpleural placement. Medial redirection not recommended because of risk of neuraxial injection. Local Anesthetic: 3-4 ml/ level for multiple level block, 15-20 ml for single level, and infusion @ 0.1 ml/kg/h. Appropriate drugs: bupivacaine 0.25-0.5%, ropivacaine 0.250.5%, or lidocaine 1%; with epinephrine (2.5 μg/ml). Mechanism and Spread of Anesthesia: 15 ml bupivacaine 0.5% in TPVs produces unilateral somatic block over 5 (range: 1-9) dermatomes, and sympathetic block over 8 (range 6-10) dermatomes. Possible areas of spread: May remain localized May spread to contiguous levels above and below Intercostal space laterally Epidural space, mostly unilateral and insignificant, in up to 70% Single 15-20 ml injection as effective as multiple 3-4 ml/site. Increasing volume may predispose to bilateral anesthesia If a wide block (≥ 5 dermatomes) is desired, preferable to do multiple injections, or 2 injections several dermatomes apart Pharmacokinetics: In adults, the commonly used bolus dose of 20 ml 0.5% bupivacaine results in a mean (SEM) maximum concentration of 1.45 (0.32) μg/ml in a median time of 25 min (range, 10-60 min. Progressive accumulation of bupivacaine can occur during continuous thoracic paravertebral infusion without clinical signs of toxicity, although bupivacaine levels have often exceeded the threshold for central nervous system toxicity (2-4.5 μg/ml). This may account for the few reported cases of postoperative confusion that resolved after temporary cessation of the infusion. Lidocaine, with a shorter elimination half-life and lower cardiotoxicity than bupivacaine, may be an attractive alternative. Contraindications: Infection at the site of needle insertion, Empyema Allergy to local anesthetic drugs, and Tumor occupying the TPVS. Relative Contraindications: Coagulopathy Kyphoscoliosis (chest deformity may predispose to pleural or thecal puncture) Patient with previous thhoracotomy: TPVB may be obliterated by scar tissue and adhesion of lung to chest wall Complications: Failure rate 6-10%, comparable to other regional techniques. Inadvertent pleural puncture. May or may not produce pneumothorax. Clues to pleural puncture: ‘Pop’ sensation Irritating cough Sharp pain in chest or shoulder Air not aspirated unless lung punctured. Air may enter through the block needle. Hypotension is uncommon, even after bilateral blocks. Dural puncture-related complications such as intrathecal injection, spinal anesthesia, and postural headache appear to be exclusive to the medial approach to the TPVS and are probably related to the closer proximity of the needle to the dural cuff and intervertebral foramen. Transient Horner’s syndrome, ipsilateral or bilateral, caused by spread of anesthetic to stellate ganglion, or preganglionic high thoracic fibres. Ipsilateral arm sensory changes (spread to T1 component of brachial plexus) Pulmonary hemorrhage (1 report with block following previous thoracic surgery) Reference: Karmakar, M. Thoracic Paravertebral Block. Anesthesiology, 2001; 95:771-780