Providing Comfort During Labor & Birth
advertisement
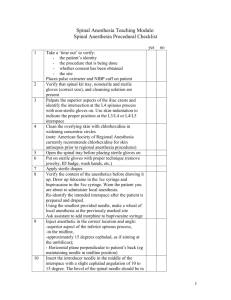
Providing Comfort During Labor & Birth Providing Comfort Concerns about the discomfort and pain involved in labor and birth dominate the thoughts of childbirth. Use neutral terms-contraction instead of pain Pharmacologic agents pose risks for both mother (hypotension) and fetus (bradycardia). Experience of Pain During Childbirth Etiology of Pain: During contractions, blood vessels constrict, reducing the blood supply to uterine and cervical cells, resulting in anoxia to muscle fibers. Anoxia causes pain. Stretching of cervix and perineum Pressure of fetal presenting part on tissues, organs. Physiology of Pain: Basic protective mechanism that alerts a person that something is happening. Perception of Pain: Pain is perceived differently Body produces endorphins (naturally opiate like substances) Factors Influencing Pain Perception: Fetal position, fear, anxiety, worry, expectation of pain, body image, and selfefficacy. Pain Relief Measures Empowering women and their partners with information so they can decide how to best relieve pain during labor. Support From a Coach Emotional involvement of husband May need someone else to coach Alternative Therapies For Pain Relief Based on gate control theory concept that distraction can be effective in preventing the brain from processing pain sensations coming into the cortex. Alternative Therapies For Pain Relief Relaxation Focusing and Imagery Breathing Techniques Herbal Preparations-raspberry leaves, fennel, life root. Blue cohosh toxic. Aromatherapy and Essential Oils-Lavender and Jasmine Heat and Cold Applications Bathing or Hydrotherapy Therapeutic Touch and Massage Yoga Reflexology-pressure to hands, feet, and ears. Crystal or Gemstone Therapy-specific positioning to be effective. Hypnosis Biofeedback Transcutaneous Electrical Nerve Stimulation-TENS T10-L1 Acupressure and Acupuncture Intracutaneous Nerve Stimulation-injection of sterile water or saline along borders of sacrum. Pharmacologic Pain Relief Analgesia-reduces or decreases awareness of pain. Anesthesia-causes partial or complete loss of sensation. Ask about allergies to medications. Virtually all medications cross the placenta. No aspirin for pain. Goals: Relax the woman and relieve her discomfort, yet have minimal systemic effects on her uterine contractions, her pushing effort, or the fetus. Medications with a molecular weight > 1000 cross the placenta poorly those with a molecular weight < 600 cross very readily. Narcotic Analgesics Potent analgesic effects-causes fetal CNS depression. Intrathecal Narcotics: Injection into the spinal cord. (Morphine) Catheter is introduced into the subarachnoid space of the spinal cord. Takes effect in 15 to 30 min. and lasts 4 to 7 hours. May need pudental block in late labor. Additional Drugs: Tranquilizers (vistaril, phenergan) Regional Anesthesia: Injection of a local anesthetic to block specific nerve pathways. (Marcaine, Nesacaine) Block sodium and potassium transport in the nerve membrane. Allow the woman to be completely awake and aware of what is happening. May or may not be aware of contractions. Helps prevent postpartal hemorrhage. Epidural Anesthesia (Peridural Blocks): Anesthetic agent placed just inside the ligamentum flavum in the epidural space. Level L4-5, L3-4 or L1-2 Blocks spinal nerve roots in the space and sympathetic nerve fibers with them. Blocks pain for labor and birth. CSF is not entered with epidural. No HA. Spinal headache due to leakage of CSF or instillation of air into CSF. Concerns: Hypotension Keep on side afterwards Tends to prolong second stage of labor. Technique for Administration: Lumbar epidural anesthesia done at 5 to 6 cm dilated. Pt. lies on side or sits upright. Clean lumbar area with antiseptic solution. Local anesthetic injected into skin at L3-4 3 to 5” needle is passed into epidural space. Catheter is passed through needle into space and needle is withdrawn and catheter is taped into place. Test with a local anesthetic solution through cathether, wait 5 min. check legs for flushing, and warmness, evidence that it is in place. Produces anesthesia up to level of the umbilicus in 10 to 15 min, lasts 40 min to 2 hours. Monitor VS temp will increase. Bladder will fill without woman knowing so void q 2 hours. I&O PCEA Combined Spinal Epidural Technique Anesthesiologist administers-inserts epidural needle then a fine spinal needle into CSF. A narcotic agonist (fentanyl) is added to CSF and needle is withdrawn. Immediate pain relief Spinal (Subarachnoid) Anesthesia: Used less frequently today. Local anesthetic agent (Marcaine or Naropin) is injected using lumbar puncture technique into subarachnoid space (CSF) L3-4 interspace. Rises to T10. IV of LR solution for hydration. Spinal headache due to leakage of CSF or instillation of air into CSF. Have woman lie flat and give analgesic. Medication for Pain Relief During Birth Natural pressure anesthesia. Local Anesthetics Local infiltration: Injection of anesthetic into superficial nerves of the perineum (Lidocaine). Along borders of vulva. Lasts 1 hour Pudendal Nerve Block: Injection of local anesthetic near the right and left pudendal nerves at the level of the ischial spine. Injection made through vagina Relives pain in 2 to 10 min., lasts for 1 hour General Anesthesia Never preferred due to dangers of hypoxia and inhalation of vomitus. Pentothal plus 6 other drugs available. Endotracheal tube. Infant may need resuscitation. Comfort During Labor Reduce Anxiety With Explanations of Labor Process: Clear understanding of what to expect. Do not know or may not remember. Provide Comfort Measures: Reposition or walk Ice chips, wet cloth Change pads frequently Clean gown, shower Pharmacologic pain relief