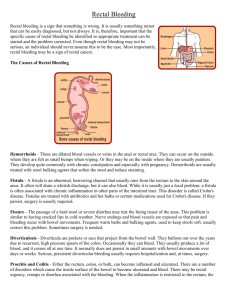
1.5 Delay in diagnosis of colorectal cancer
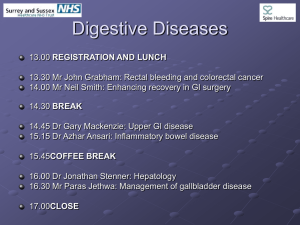
advertisement

Diagnostic Delay, Symptoms, and Stage of Colorectal Cancer: Population-based Observational Studies in Denmark. Ph.D. THESIS Marianne Korsgaard Department of Surgery L Department of Clinical Epidemiology Aarhus University Hospital Faculty of Health Sciences, University of Aarhus, 2005 1 The four studies listed below constitute the basis for this doctoral thesis. Study I: Korsgaard M, Pedersen L, Sørensen HT, Laurberg S. Diagnostic delay is associated with the stage of rectal cancer but not of colon cancer. Submitted for publication. Study II: Korsgaard M, Pedersen L, Laurberg S. Delay of Diagnosis and Treatment of Colorectal Cancer. A Danish Population-based Study. Submitted for publication. Study III: Korsgaard M, Pedersen L, Sørensen HT, Laurberg S. Symptoms, Diagnostic Delay, and Stage of Colorectal Cancer. Submitted for publication. Study IV: Korsgaard M, Pedersen L, Lous J, Sørensen HT, Laurberg S. Correlation between patients’ and general practitioners’ reported diagnostic delay in Danish patients with colorectal cancer. Submitted for publication. 2 Contents Contents ............................................................................................................................................... 3 1. Introduction .............................................................................................................................. 4 1.1 Incidence, staging, and prognosis of colorectal cancer .............................................................. 4 1.2 Risk factors for colorectal cancer............................................................................................... 9 1.3 Symptoms and diagnosis of colorectal cancer ........................................................................... 9 1.4 Colorectal cancer diagnosis: recommendations ....................................................................... 11 1.5 Delay in diagnosis of colorectal cancer ................................................................................... 13 1.6 Aims ......................................................................................................................................... 19 2. Methods.................................................................................................................................... 20 2.1 Study I. Diagnostic delay is associated with the stage of rectal cancer but not of colon cancer ........................................................................................................................................................ 21 2.2 Study II. Delay of Diagnosis and Treatment of Colorectal Cancer. A Danish Population-based Study .............................................................................................................................................. 25 2.3 Study III. Symptoms, Diagnostic Delay, and Stage of Colorectal Cancer .............................. 27 2.4 Study IV. Correlation between patients’ and general practitioners’ reported diagnostic delay in Danish patients with colorectal cancer ...................................................................................... 28 3. Results....................................................................................................................................... 29 3.1 Study I ...................................................................................................................................... 29 3.2 Study II..................................................................................................................................... 36 3.3 Study III ................................................................................................................................... 39 3.4 Study IV ................................................................................................................................... 41 4. Discussion ............................................................................................................................... 43 5. Conclusions ............................................................................................................................ 55 6. Perspectives ............................................................................................................................ 57 7. Summary.................................................................................................................................. 58 8. Danish summary .................................................................................................................. 62 9. References............................................................................................................................... 67 3 1. Introduction Colorectal cancer is one of the most common malignancies in western countries with the average five-year post-diagnosis survival of only 50 percent (1-3). For unknown reasons, Danish patients with colorectal cancer have poorer prognosis than their counterparts in other Scandinavian countries (4). Stage of the tumor at the time of treatment is the most important predictor of survival (5;6). Given the cancer biology, long diagnostic delays are typically expected to lead to tumors being diagnosed at advanced stages; for colorectal cancer, however, the evidence to this end is not clear-cut (7-24). Diagnosis of colorectal cancer from clinical symptoms alone is difficult (25;41-48) because the disease often presents with vague and unspecific symptoms identical to those of benign colorectal diseases (25-34) that are widely prevalent in general population (25;26;28-33;35-41). 1.1 Incidence, staging, and prognosis of colorectal cancer Incidence Colorectal cancer is the third most common cancer in Denmark, skin cancer excluded. In 2000, there were 2323 new cases of colon cancer (male-to-female ratio, 1.0 to 1.1), and 1027 cases of rectal cancer (male-to-female ratio, 1.0 to 0.7). The incidence of colon cancer in 2000 was 24 per 100,000 among men and 20 per 100,000 among women. For rectal cancer, the corresponding incidence values per 100,000 persons were 15 and 8 (49). The mean age of colorectal cancer patients is 70 years. In the last decade, the incidence of colon cancer has been slightly increasing, whereas the incidence of rectal cancer has been slightly decreasing (49). Staging Use of different staging classifications of colorectal cancer makes it difficult to compare data on tumor stage across cancer registries. For colorectal cancer classification, Dukes’s staging is commonly used (50) (Table I). The Danish Cancer Registry usually classifies the 4 colorectal cancers into three stages: local growth, local spreading, and distant spreading (52). The TNM Staging System (T: Tumor, N: Lymph Nodes, M: Metastases) of the International Union Against Cancer (UICC), a common and more specific system of cancer staging, is now frequently used when classifying colorectal cancer (Table II). Table I. Characteristics of Dukes’s stages and estimated five-year recurrence-free survival for patients with colon and rectal cancer. Dukes’s Characteristics Stage Estimated 5-year survival Colon cancer Rectal cancer Dukes’s A Tumor limited to the bowel-wall 70% 75% Dukes’s B Tumor invades through the bowel-wall 55% 50% Dukes’s C Tumor with spreading to regional lymph nodes 30% 25% Dukes’s D* Tumor with distant metastases or peritoneal 0% 0% carcinosis *Stage D is not part of the original Dukes’s classification, but it was added to classify disseminated colorectal cancer (51). Table II. Characteristics of the TNM staging classification, fourth edition (53). TNM Category T1 Clinical Classification/Definition Tumor limited to submucosa T2 Tumor invades muscularis propria T3 Tumor invades muscularis propria extending into subserosa or into nonperitonealized pericolic or perirectal tissue T4 Tumor directly invades other organs or structures and/or perforates visceral peritoneum N0 No regional lymph node metastasis N1 Metastases in 1-3 regional lymph nodes N2 Metastases in 4 or more regional lymph nodes M0 No distant metastases and no peritoneal carcinosis M1 Distant metastases or peritoneal carcinosis 5 An estimated 5-10 percent of Danish colon cancer patients are in Dukes’s stage A, and 30 percent are in each Dukes’s stages B, C, and D. For rectal cancer, 15 percent of the patients are estimated to have tumors in Dukes’s stage A, 30 percent in Dukes’s stage B, 30 percent in Dukes’s stage C, and 15 percent in Dukes’s stage D. Patient mortality increases with higher tumor stage. The estimates of crude recurrence-free 5-year survival rates for colon and rectal cancers are given in Table I (4). A 30-day postoperative mortality is about 25 percent for all patients, regardless of tumor stage (54). Dukes’s classification cannot be used on non-resected tumors, except when liver or lung metastases or abdominal carcinosis are radiologically verified, in which case the tumors are assigned Dukes’s stage D (51;53). The validity of Dukes’s staging depends on the number of lymph nodes examined in a specimen. During the study period, Danish guidelines recommended that at least 10 lymph nodes be examined for a valid staging (55). In addition, the validity of the Dukes’s stage D assignment depends on the quality of examination for the disseminated disease (56). Prognosis The distribution of colorectal cancer stages at the time of resection in Denmark is similar to that of other Scandinavian countries, yet relative survival in Denmark is lower than that in Sweden (which has the highest survival), Norway, or Finland (4) (Figure I). 6 Figure 1. Age-adjusted relative survival* after colon cancer in Scandinavian countries, 1990-1995. Men. Den Swe Nor Fin 1 year 3 years 5 years Age-adjusted relative survival after colon cancer in Scandinavian countries, 1990-1995. Women. Den Swe Nor Fin 1 year 3 years 5 years 7 Age-adjusted relative survival after rectum cancer in Scandinavian countries, 1990-1995. Men Den Swe Nor Fin 1 year 3 years 5 years Age-adjusted relative survival after rectum cancer in Scandinavian countries, 1990-1995. Women Den Swe Nor Fin 1 year 3 years 5 years The total survival is defined as the proportion of a cohort surviving within a given time interval. The relative survival is defined as the total survival compared with the expected survival, if the cohort had the same mortality as the general population. 8 1.2 Risk factors for colorectal cancer Certain persons have an increased risk of colorectal cancer, partially caused by genetic factors. Familial adenomatous polyposis (FAP) (57), attenuated familial adenomatous polyposis (AFAP), and hereditary non-polyposis colorectal cancer (HNPCC) (58) are diagnosed in about 2-5 percent of Danish colorectal cancer patients. Additional risk factors include history of colorectal cancer or adenoma, chronic inflammatory bowel disease, and Crohn’s disease (59;60). Dietary factors are also important in determining colorectal cancer risk. Diet rich in red meat and saturated fat increases the risk, while consumption of fruits, vegetables, fiber, calcium, and folic acid may be protective. Lifestyle factors also play a role with obesity being a risk factor and physical activity, a preventive factor of colorectal cancer. 1.3 Symptoms and diagnosis of colorectal cancer The differential diagnosis of colorectal cancer may not be straightforward. The symptoms of colorectal cancer are often unspecific and indistinct. These symptoms are prevalent in the general population with most patients having benign gastrointestinal disease, and only a small fraction of them having cancer (26;27;34;43;45;46;64-67). According to an Australian study, about 20 percent of the general population experience rectal bleeding, and only 3 percent of them have colorectal cancer (26). Hemorrhoids are the most common cause of rectal bleeding. In Hong Kong, a prospective study of 337 patients over the age of 40 presenting with rectal bleeding, showed that 80 percent of the patients had hemorrhoids, but 16 percent of the patients also had polyps or colorectal cancer (65). In a Danish study, 63 percent of patients with colorectal cancer who experience rectal bleeding, also had hemorrhoids (66). Patients with colorectal cancer tend to present with more than one onset symptom, the most frequent symptoms being rectal bleeding, change of bowel habits, ileum, and abdominal pain. 9 Other symptoms of colorectal cancer include anemia, weight loss, nausea, tenesmus, constipation, increased abdominal size, mucus in stools, and palpable tumor (23;42; 43; 61-63). The problem of delayed diagnosis is exacerbated by patients’ under-reporting of the vague and unspecific gastrointestinal symptoms, unless prompted by specific questions from physicians (68;69). This under-reporting is likely caused by lack of knowledge about colorectal cancer symptoms (26;40;41;70-74). Data from most studies of abdominal symptoms among the general population are often of unknown quality, as they are primarily taken from questionnaires and interviews; in addition, some studies are not population-based and thus may be non-representative (26;27;30;36;37;39;40;66;75-78). The location of colorectal cancer cannot be determined from the symptoms alone, though some symptoms are more frequent when the cancer is located in the left side of the colon and in the rectum, while others are most frequent for right-sided colon cancer (23;27;61;63;65;67;79-81). Rectal bleeding with visible blood in stools tends to be a symptom of left-sided colorectal cancer, whereas right-sided cancer more often presents with occult blood and symptoms of anemia (7;23;29;42;61;65;67;82;83). Abdominal pain is more frequent for right-sided colon cancer than for left-sided colon cancer or the rectal cancer (23;27;61;63;67;79). In general, rectal bleeding and changes in bowel habits are the most usual symptoms of cancer of the rectum or the sigmoid colon. Symptoms of cancer located in the right side of colon are less well-defined (7;23;29;42;61;67;79;82;83). About 20 percent of colorectal cancer cases present acutely with ileum symptoms, and less frequently with acute abdomen caused by perforation (61). An acute presentation is more common for colon cancer than for rectal cancer (84-86). 10 1.4 Colorectal cancer diagnosis: recommendations Owing to the unspecific and vague nature of symptoms, there are no preferred evidence-based recommendations about examination of patients with suspected colorectal cancer (25;41;43-45;47;48). In Denmark, the Health Technology Assessment (HTA) (4) recommends that general practitioners examine patients older than 40 years with suspected colorectal cancer by abdominal palpation, rectal exploration, and by measuring blood hemoglobin. For female patients, a gynecological examination should be added to rule out gynecological disease. If there is reason to believe that the patient has colorectal cancer, referral for either sigmoidoscopy combined with a sensitive test for occult blood in the stools or colonoscopy is indicated (Figure II). This applies to patients older than 40 years old with no specific risk of colorectal cancer. For high-risk patients, colonoscopy is always indicated. 11 Figure II. Recommended clinical practice for patients with suspected colorectal cancer. Patients older than 40 years presenting with rectal bleeding or change in bowel habits > 1 month or iron deficiency or anemia (and, if indicated, with abdominal pain, loss of weight or obscure dyspepsia) Mandatory examination of all patients: general evaluation abdominal palpation rectal examination gynecological examination (for women) blood hemoglobin measure Risk factors: e.g., history of colorectal cancer or adenoma, risk of inflammatory bowel disease, endometrial cancer, or first-degree relatives with colorectal cancer, adenoma, or endometrial cancer No risk factors for colorectal cancer Monosymptomatic Non-red rectal bleeding Change in bowel habits red rectal bleeding or red rectal bleeding and > 1 month change in bowel habits Other important indications Iron deficiency anemia Anoscopy Sigmoideoscopy i.a. i.a. i.a. i.a. No more examinations Haem-sensa x 3 POS. NEG. Clinical reassessment after 3 month Gastroscopy AND Symptoms No symptoms No more examinations Colonoscopy 12 All Danish patients suspected of having colorectal cancer must be examined within two weeks after referral to a hospital (87). Attempts have been made to set up a system, to classify patients suspected of having colorectal cancer and patients with benign colorectal diseases, by clinical picture alone. The aim was to establish clinical practice guidelines that are sufficiently sensitive to detect cancers and sufficiently specific to be economic, and thus supportable with public funding. However, no final conclusion has yet been reached about feasibility of such system (4;25;39;41-48). 1.5 Delay in diagnosis of colorectal cancer In general, diagnostic delay is the time from appearance of onset symptoms of cancer until the start of treatment. The longer the diagnostic delay, the more likely are tumors to grow to advanced stages, with the rate of growth depending on type an aggressiveness of a particular tumor. It is expected therefore that, for the same type and aggressiveness of cancer, reducing diagnostic delay will help treat cancer at a less advanced stage thereby improving patient prognosis. For colorectal cancer, diagnostic delay is defined as the period from the date of the patient-reported onset symptom(s), until surgery, start of preoperative radiotherapy, or palliative treatment. Thus, the beginning of this period is difficult to ascertain, as it depends on patient recall and awareness of which symptoms pertained to colorectal cancer, while the end of the period is obtainable from medical records. The total delay period can be divided into three components. The “patient delay” is the time from the date of onset of symptoms to the first symptom-related physician visit. The “doctor delay” (or “G.P. delay”) is the time from the first visit to a general practitioner until referral for additional hospital-based evaluation for colorectal cancer. The “hospital delay” is the time from patient’s referral to the hospital until the start of treatment. “Hospital delay” can be further divided into “doctors’ delay of diagnosis”, i.e. time from referral to the hospital until the diagnosis has been made, and “treatment delay”, i.e. time from diagnosis until start of treatment (Figure III). 13 Figure III. Components of diagnostic delay. Onset of Symptoms Contact to a G.P. Referral Diagnosis Start of treatment [ Patient delay ][ G.P. delay ][ Hospital delay [Doctors’ delay of] [ diagnosis ] Delay of treatment ] A long “doctors’ delay of diagnosis” can be caused by the general practitioner or the hospital. The delay of a sigmoidoscopy or a colonoscopy substantiating the diagnosis, depends on the information provided by general practitioner in the referral letter to the hospital (61;88) and on the hospital capacity. In practice, treatment delay usually occurs in hospitals where it is caused by administrative errors or by the lack of financial or human capacities, whereby some patients diagnosed with colorectal cancer must wait for 14 days of more until the treatment can begin (67;84;89;90). It is still not clear, however, whether diagnostic delay is important for the stage and the prognosis of colorectal cancer. Most earlier studies reported no association between diagnostic delay and stage (8-18;22;24). Five studies found an association between stage with diagnostic delay for rectal cancer (7;19-21;23), and three of them found the association for colon cancer as well (20;21;23). Most of the prospective studies included between 100 and 582 colorectal cancer patients, and the majority of the studies were based on delay data obtained from medical records (11;13;14;16-18;20;22;24) (Table III). Holliday and Hardcastle compared mean delay according to Dukes’s stages in 100 colon cancer patients and 100 rectal cancer patients (12) and found no association between diagnostic delay and stage. In this study, combined analysis was performed for patients with colon and rectal cancers. Rowe-Jones and Aylett (21) and Robinson et al. (20) did find an association between diagnostic delay and stage for both colon and rectal cancer. Rowe-Jones and 14 Aylett did separate analyses for colon and rectal cancers. In that study, 50 percent of colon cancer patients with medical delay longer than 2 months had advanced cancer compared only 25.6 percent of patients without such delay (relative risk, 1.9). Among rectal cancer patients, 63.6 percent of those with medical delay longer than 2 months had advanced cancer compared with only 29.5 percent in the non-delayed group (relative risk, 2.2) (21). Robinson et al. (20) retrospectively studied medical records of colorectal cancer patients. The authors found than among 277 colon cancer patients, patients with advanced tumors were more likely than patients with localized tumors to have had a medical delay longer than six weeks (60 percent vs. 49 percent). The corresponding difference was somewhat greater (45 percent vs. 30 percent) for the 168 rectal cancer patients. In a prospective study of 218 rectal cancer patients and 336 colon cancer patients, Arbman et al. (7) report an association between diagnostic delay with the stage of rectal cancer, but not of colon cancer. Pahlman et al. (19) examined primarily the effectiveness of preoperative radiotherapy, but they also examined diagnostic delay in patients with rectal and rectosigmoid cancer. In 221 patients enrolled prospectively and 83 included retrospectively, they found a significant association between diagnostic delay and stage of cancer at the time of surgery. A German study (23) of 70 colorectal cancer patients reported correlation between diagnostic delay and stage for the 40 colon cancer patients as well as for the 30 rectal cancer patients. 15 Table III. Studies of the association between diagnostic delay and stage of colorectal cancer (chronologically by the first author). Association reported? Rowe-Jones 1965 UK Devlin 1973 UK Irvin 1977 UK Holiday 1979 UK McDermott UK 1981 Pescatori 1982 Italy Khubchandani 1982 USA Jolly 1982 New Zealand col rec Yes Yes Separate analysis for colon and rectal cancer? Yes No Number of patients studied Inclusion rate Prospective and/or retrospective inclusion Measure of delay used Did analysis include emergency cases? Non-adv. vs. Adv. Prosp. Retros. NR NR NR interval Yes No 0 74% No Yes interval Yes No col rec col rec 100 100 NR 0 229 Dukes’s (- D) Dukes’s (C1&C2) Dukes’s (-D) No No 169 166 NR NR No Yes interval Yes No No No 100 100 NR NR Yes No mean Yes No Dukes’s 711 0 94% 0 No Yes interval Yes No Dukes’s No No No 161 NR No Yes interval Yes No Dukes’s No No 194 NR No Yes interval Yes No Dukes’s No No 455 NR No Yes interval Yes No Dukes’s (-D) Påhlman 1984 Sweden Yes 0 270 0 76% Yes Yes interval Yes Yes B2= adv. Dukes’s B2=adv. Dukes’s Gaffner 1986 Sweden No No Yes 50 50 NR NR Yes No interval Yes No Robinson 1986 Israel Yes Yes Yes 277 168 NR NR No Yes interval Yes Yes/ No Yes No median Yes No Ratcliffe 1989 UK Dukes’s stage or TNM No No 332 84% Dukes’s A&B= Non-adv Dukes’s (-D) 16 Kyle 1991 Saudi Arabia Goodman 1993 UK Arbman 1996 Sweden Langenbach 2003 Germany Gonzalez-Hermoso 2004 Spain Bharucha 2005 UK No No No 146 94% No Yes interval Yes No Dukes’s 152 0 89% 0 No Yes interval No No Dukes’s (-D) No Yes Yes 336 218 93% 93% Yes No interval Yes No Dukes’s Yes Yes Yes 40 30 NR NR Yes median Yes No UICC No No 660 74% No Yes interval No Yes TNM No No 582 89% NR NR Interval No No Dukes’s (-D) NR=Not reported 17 The majority of studies were conducted retrospectively, while prospective studies had small number of patients. Few studies examined colon and rectal cancer patients separately and only two studies considered emergency cases. In addition, the definition of diagnostic delay varied across the studies, and no study addressed the validity of tumor staging. 18 1.6 Aims In the following observational studies, I examined the association between diagnostic delay, onset symptoms, and stage of colorectal cancer. I also examined how and whether the interval between the onset of symptoms of colorectal cancer until the start of treatment is influenced by the patients, general practitioners, or hospitals. All studies were conducted prospectively within a large cohort of Danish patients. AIM I: To examine the association between diagnostic delay and stage of colon and rectal cancer at time of surgery (study I). AIM II: To examine the interval between the onset of colorectal cancer symptoms and the start of treatment. I aimed to determine the extent to which this diagnostic delay for colon cancer patients and/or for rectal cancer patients was caused by patients, general practitioners, or hospitals. I examined the adherence to the Danish Health Authorities guidelines recommending that patients with suspected colorectal cancer be further examined within 14 days, and those with the confirmed diagnosis, be treated within 14 days of diagnosis (study II). AIM III: To examine whether symptoms are associated with diagnostic delay or with the stage of the tumor, separately for colon and rectal cancer patients (study III). AIM IV: To compare length of diagnostic delay reported by patients with that reported by general practitioners (study IV). The thesis was conducted within the large population-based Scandinavian study based on prospectively recorded data, aiming at examining prognosis, diagnostic delay and comorbidity of colorectal cancer patients in Denmark, Norway and Finland. 19 2. Methods We conducted separate analyses for colon cancer and rectal cancer patients. The analyses were carried out with SPSS software (version 10.0)and in the Excel Episheet program (URL: http://members.aol.com/krothman/modepi.htm). 20 2.1 Study I. Diagnostic delay is associated with the stage of rectal cancer but not of colon cancer Patients We aimed at including a minimum of 350 colorectal cancer patients from Aarhus County and 350 colorectal cancer patients from Ringkoebing and Ribe counties; the population of these counties is representative of the general Danish population. Hospitalized patients were registered prospectively between 1 January 2001 until 30 June 2002 in three Danish counties: Aarhus County (6 hospitals and about 630,000 inhabitants), Ringkoebing and Ribe Counties (7 hospitals and 475,000 inhabitants). Eligible patients had histologically verified primary adenocarcinoma of the colon or rectum (WHO histological classification 1989; ICD 8140, 8480, 8490, 8020 (91)). We excluded patients with inherently increased risk of colorectal cancer: those under colonoscopic surveillance due to hereditary non-polyposis colorectal cancer; patients with attenuated familial adenomatous polyposis; familial adenomatous polyposis; or with chronic inflammatory bowel disease. Nurses and surgeons from the 13 hospitals prospectively enrolled colorectal cancer patients from their departments in the study. Pathology reports from the four pathology departments serving all study hospitals were sent to the study personnel at Aarhus University Hospital. Pathology reports were used to ascertain diagnosis and tumor stage and to insure participation of all eligible colorectal cancer patients residing in study counties. Patients completed interviewer-administered questionnaires. In order to standardize the interviews, the author of this Ph.D. thesis supervised the interviewers during the inclusion period. Delay Data Patients were asked to endorse having a list of typical symptoms with the dates; duration of symptoms; dates of seeing a physician for those symptoms; type and date of therapy received; and dates of follow-up examinations of colon or rectum. For patients who were unable to 21 remember exact dates, but remembered the month, or the season, the corresponding median date was used. For symptoms lasting longer than four years without change that were deemed benign on earlier examinations, the date of physician visit leading to the cancer diagnosis was considered the date of that symptom’s appearance. In addition, patients were asked whether general practitioner performed a rectal examination. Most patients were interviewed before undergoing surgery to avoid potential recall bias resulting from patients’ knowledge about tumor’s stage. In case that was not possible (e.g., for acutely operated patients), we aimed to conduct interviews before a histology report was issued. The author of this thesis contacted interviewers to resolve any discrepancies in the questionnaires. Pathology and Surgery Data In Denmark, for all patients operated for colorectal cancer, a Colorectal Cancer Report (CRC report) is filed that includes macroscopic and microscopic description of the specimen. For this study, responsible surgeons reported the following data on tumors: neoplasm location; whether surgery was emergency or elective; patients’ other treatments; intra- and post-operative complications; re-operations; in-hospital postoperative deaths; Dukes’s classification; TNM classification; the number of lymph nodes in the specimen; and number of lymph nodes with metastases. Two independent pathologists who were not blinded to the diagnoses validated dukes’s stage in a random sample of tumors through histological review. The macroscopic findings from the pathology reports were filled into a data review report. Hematoxylin-eosin-stained sections and occasionally specially stained sections were reviewed afterwards. Correlation between microscopic findings in the primary CRC report and the data review report was scored on a 4-point scale: complete agreement; minor disagreement (not relevant to postoperative adjuvant treatment); 22 medium disagreement (primarily in TNM classification and not relevant to postoperative adjuvant treatment); and major disagreement (in Dukes’s stage relevant to postoperative adjuvant treatment). Every electively operated colorectal cancer patient had a preoperative ultrasonic examination of the liver, and a chest radiograph. The author of the thesis validated dukes’s stage D at time of surgery for all registered patients by reviewing medical records (after the patients had left the hospital), resulting in correction of 3.5% of staging information. The corrections stemmed most often from additional information about lung or liver metastases, or carcinosis found in the medical record. The corrections were done before analyzing the data. The boundary between colon and rectum is not well defined. Some studies place rectum boundary as far as 20 or 25 cm from anus (10;19). We defined a cancer as a rectum cancer if its most distal part was localized 0-15 cm from the anus. Statistical Analysis Diagnostic delay was defined as the period from the date of the first symptom of colorectal cancer until surgery, start of preoperative radiotherapy, or palliative treatment. Diagnostic delay was classified as short delay (up to 60 days) – the reference category; median delay (61-150 days); and long delay (>150 days). In selecting 150 days as the cutoff between the two latter groups, we considered comparability of group sizes and the fact that median delay value was included in the median delay group. Dukes’s stage was dichotomized into non-advanced cancers (Dukes’s stages A and B) and advanced cancers (Dukes’s stages C and D). We analyzed the data first by obtaining contingency tables for the main study variables and calculating relative risk (prevalence rate ratio) of having advanced stage of the cancer according to the three diagnostic delay categories. We obtained relative risk estimates stratified by age, gender, and type of surgery (elective, emergency). In addition, we examined an alternative 23 classification of diagnostic delay using categories of 90 days (short delay), 91-180 days (median delay), and >180 days (long delay)*. * Results of this additional analysis were not included in Study 1, but are discussed in the PhD thesis. 24 2.2 Study II. Delay of Diagnosis and Treatment of Colorectal Cancer. A Danish Population-based Study Patients Same as in Study 1. Delay Data Denmark has a tax-funded health care that covers 100 percent of hospital care costs. Over 95 percent of Danes are registered with a family general practitioner (G.P.), who is paid by the county according to the number of patients registered annually. For routine complaints, patients are expected to contact their family general practitioner or, in case of emergencies outside business hours, to contact a general practitioner on call. General practitioners examine the patient and refer them to hospitals if indicated. We defined total diagnostic delay as the period from the date of onset symptom(s) of colorectal cancer until treatment (surgery, start of preoperative radiotherapy for rectal cancer if indicated (47), start of palliative treatment in case of disseminated cancer, or inoperability, old age, or patient’s refusal to undergo major surgery). Total delay was subdivided into the following periods (Figure III): Patient delay: the interval from symptom(s) onset until physician (primarily, a G.P.) visit about the symptom(s); G.P. delay: the interval from first physician visit until referral to the hospital; Hospital delay: the interval from hospital referral until start of treatment. The hospital delay was further divided into “doctors’ delay of diagnosis” defined as the time from the hospital referral by G.P. until the diagnosis; “delay of treatment” defined as the interval between diagnosis and start of treatment. 25 Data on symptoms and G.P. visits were obtained from patient interviews (as in Study 1). Data on hospital treatment were available form medical records. Recommendations for colorectal cancer patients Starting in 1998, Danish Government recommends that patients with suspected colorectal cancer undergo diagnostic procedures within 14 days of hospital referral and, if colorectal cancer is diagnosed, treated within the 14 days following the diagnosis (87). The Danish Colorectal Cancer Group recommended decision tree for examining and diagnosing patients with suspected colorectal cancer (4;47) are shown in Figure II. Statistical Analysis We did separate analyses for colon cancer and rectal cancer patients. We tabulated and examined distributions of the main study variables: age, gender, type of surgery (elective or emergency), and delay periods. We calculated the 25th percentile, the median, the 75th percentile, and the 95th percentile delay for all patients stratified according to age and gender. We calculated the proportion of patients for whom the recommendations of the Danish Government (87) were met. 26 2.3 Study III. Symptoms, Diagnostic Delay, and Stage of Colorectal Cancer Patients Same as in Study 1. Symptoms Data Interviewers asked patients to endorse having had each of the following symptoms and to give the date of their onset: rectal bleeding, constipation, diarrhea, change in bowel habits, abdominal pain, ileus, weight loss, tiredness, anemia, decreased appetite, nausea, palpable tumor, increased size of the abdomen, tenesmus, mucus in stools, icterus, or others. The patients were then asked if any of the symptoms reoccurred, and, if so, on what date. Symptoms experienced no later than one week after the onset symptom(s) were also classified as onset symptoms. Pathology and Surgery Data Same as in Study 1. Statistical Analysis The analyses were made for colon cancer patients and rectal cancer patients, separately. We tabulated main study variables and calculated the frequency of each onset symptom and of the most frequently occurring onset symptoms combinations. We calculated the median diagnostic delay for each onset symptom. We analyzed the association between onset symptoms/symptom complexes and diagnostic delay by obtaining contingency tables of the numbers and frequencies of patients with the different onset symptoms/symptom complexes in the three delay groups defined for Study I (short delay; 0-60 days, median delay; 61-150 days, and long delay; >150 days). We calculated the association between the most frequent onset symptoms and symptom complexes and stage of tumor using the definition of advanced cancer from Study I with stage dichotomized into non-advanced (Dukes’s and B) and advanced (Dukes’s C and D). 27 2.4 Study IV. Correlation between patients’ and general practitioners’ reported diagnostic delay in Danish patients with colorectal cancer Patients Same as in Study 1. General Practitioners Ninety percent of the patients included in studies I-III consulted their family general practitioner regarding symptoms related to colorectal cancer. The remaining 10 percent of the patients either consulted a general practitioner on call or went directly to an emergency department. To examine the quality of interview data and correlation between patient- and physician-provided information, we drew a 20-percent random sample of the patients who had consulted their family general practitioners. We surveyed these general practitioners by a mail-in questionnaire consisting of four questions taken from the original patient interview. The physicians were asked to answer questions about study patients’ presenting symptoms; their reported onset dates; date of patient visit; and type of follow-up prescribed. This survey was conducted in parallel with enrolling the patients for studies I-III. Questionnaires on randomly selected 150 patients were sent 132 general practitioners, as 18 of them saw more than one study patient. Physicians not responding within 14 days were contacted by telephone with a reminder. Statistical Analysis We cross-tabulated duration of delay (categorized variable) according to physicians’ and patients’ reports. We estimated the correlation between the patient-reported delay and the G.P.reported delay, by conducting Spearman’s Rank Correlation test and calculating Spearman’s correlation coefficient. We then constructed an Altman’s plot (93) in which the difference (in days) between patient- and physician-reported delay is plotted against patient-related diagnostic delay. Such plot shows the relation of the magnitude of discrepancy between the two reports with the length of patient-reported delay. We also calculated the Spearman’s correlation coefficient for this relation. 28 3. Results 3.1 Study I Descriptive data During the enrollment period, we registered 951 patients in the three counties (598 had colon cancer and 353 had rectal cancer). We excluded 147 (15.5%) patients: 74 (7.8%) had dementia or were otherwise unable to participate; 61 (6.4%) died before an interview could be conducted, and 5 patients (0.5%) did not speak Danish. Two excluded patients (0.2%) were under colonoscopic surveillance due to hereditary non-polyposis colorectal cancer and 5 excluded patients (0.5%) had chronic inflammatory bowel disease. Additionally, 61 patients (6.4%) refused to participate leaving 743 patients (78.1%). County-specific participation rate was 383/486 (80%) in Aarhus County and 360/465 (77%) in Ringkoebing and Ribe counties. The participation rates were 459/598 (77%) among colon cancer patients and 284/353 (80%) among rectal cancer patients. Three colon cancer patients and seven rectal cancer patients were interviewed but had neither surgery, nor radiologically-verified liver or lung metastases and therefore could not be assigned a Dukes’s stage. These patients were excluded from the analyses of studies I and II, but were included in the analyses of studies III and IV. Patients could become unblinded to their tumor stage at the time of the interview if they had had preoperative ultrasonic examination of liver or chest radiography revealing metastases (Dukes’s stage D). Furthermore, 24 rectal cancer patients were staged preoperatively and thus could have been aware of their TNM stage. We validated Dukes’s staging in 102 (11%) of all registered patients: 86 participants (53 colon cancer patients, 33 rectal cancer patients); 10 excluded patients (7 colon cancer patients, 3 rectal cancer patients); and 6 refusers (3 colon cancer patients, 3 rectal cancer patients). 29 Tables IV shows the distribution of Dukes’s stages of ‘all registered patients’, ‘included patients’, ‘excluded patients’, and ‘patients who refused to participate’. Patients with tumors at Dukes’s stage D were more likely to refuse or be excluded. Table IV. Frequency (%) of Dukes’s stages in each patient group and in all registered patients. Colon cancer patient group All registered Included No consent Excluded N=598 N=459 N=39 N=100 Dukes’s A 72 (12%) 63 (14%) 2 (5%) 7 (7%) Dukes’s B 209 (35%) 161 (35%) 16 (41%) 32 (32%) Dukes’s C 173 (29%) 137 (30%) 9 (23%) 27 (27%) Dukes’s D 133 (22%) 95 (20%) 7 (18%) 31 (31%) 11 (2%) 3 (1%) 5 (13%) 3 (3%) Duke’s stage Unclassified Rectal cancer patient group All registered Included No consent Excluded N=353 N=284 N=22 N=47 Dukes’s A 70 (20%) 60 (21%) 4 (18%) 6 (13%) Dukes’s B 101 (29%) 85 (30%) 6 (27%) 10 (21%) Dukes’s C 94 (27%) 86 (30%) 3 (14%) 5 (11%) Dukes’s D 68 (19%) 46 (16%) 3 (14%) 19 (40%) Unclassified 20 (6%) 7 (3%) 6 (27%) 7 (15%) Duke’s stage 30 Delay Table V shows that colon cancer patients were somewhat more likely than rectal cancer patients to have a short diagnostic delay. Among colon cancer patients, more men than women had a short delay. Men were more likely than women to have a long delay for rectal cancer. Table V. Distribution of total diagnostic delay among Danish colorectal patients. Delay category Type of cancer Short Median Long Colon cancer patients (N=456) 184 (40%) 114 (25%) 158 (35%) Rectal cancer patients (N=277) 90 (32%) 91 (33%) 96 (35%) Delay and Dukes’s stage Rectal cancer patients with short delay were more likely than rectal patients with medium and long delay to have non-advanced cancer (study I, table 1), whereas there was no substantial association between stage and delay among the colon cancer patients (study I, table 2). Colon cancer patients with either median delay or long delay did not have increased risk of advanced cancer (Dukes’s stage C or D) compared with those in the short delay group (respective relative risks (RR) (95% confidence intervals (CI)): 1.0 (0.8-1.3) and 1.1 (0.9-1.4)) (study I, table 3). Among rectal cancer patients, delay and stage were associated: RR (95%% CI) was 1.9 (1.1-3.1) for median delay and 2.1 (CI 1.3-3.4), for short delay, each compared with the short delay group. The association was strongest for old rectal cancer patients (age >70 years old). Relative risk for old patients with a median delay was 2.7 (95% CI, 1.0-7.1) and for patients with a long delay 2.7 (95% CI 1.1-7.1). Relative risk for long vs. short delay was higher for women with rectal cancer (2.5 (95% CI, 1.1-5.6)) than for men with rectal cancer (1.9 (95% CI 1.0-3.5)) (study I, table 3). 31 Using different cutoffs for delay categories – 90 days for short delay, 91-180 days for median delay, and >180 days for long delay – the relative risks for having an advanced cancer in median or long delay groups were similar to those with the original categories for colon cancer patients providing no evidence of an association between delay and stage. For rectal cancer patients, relative risk estimates were somewhat smaller than with the original categories, but these differences did not affect the interpretation.(Tables VI, VII). Table VI. Distribution of total diagnostic delay among Danish colorectal patients according to the “new" cutoffs of delay categories. Delay category Short (90 days) Median (91-180 days) Long (>180 days) Colon cancer patients (N=456) 184 (40%) 114 (25%) 158 (35%) Rectal cancer patients (N=277) 90 (32%) 91 (33%) 96 (35%) Type of cancer Table VII. Relative risk (95% CI) of having an advanced cancer at time of surgery. Delay periods Colon cancer Rectal cancer 0-90 days 1.0 1.0 91-180 days 0.9 (0.7-1.1) 1.7 (1.2-2.4) >180 days 0.9 (0.8-1.2) 1.6 (1.1-2.2) 32 The median numbers of examined lymph nodes in the specimens for all registered patients and for included patients according to Dukes’s stages are shown in tables VIII and IX. Table VIII. Median number* of examined lymph nodes in the different Dukes’s stages for all registered colon cancer patients and for included colon cancer patients for whom the number of examined lymph nodes in the specimen was known. Dukes’s A Dukes’s B Dukes’s C Dukes’s D All registered patients 6 (56) 8 (190) 9 (157) 8 (93) Included patients 5 (46) 8 (146) 9 (127) 9 (70) * In parentheses is the number of patients in the different Dukes’s stages for whom the number of examined lymph nodes in the specimen was known. Table IX. Median number of examined lymph nodes in the different Dukes’s stages for all registered rectal cancer patients and for included rectal cancer patients for whom the number of examined lymph nodes in the specimen was known. Dukes’s A Dukes’s B Dukes’s C Dukes’s D All registered patients 6 (57*) 8 (90) 9 (85) 10 (48) Included patients 7 (47) 8 (75) 9 (79) 9 (40) *Footnote as in previous table. Below the lymph node data are shown stratified by delay category (table X and XI). The numbers (N) of patients in each group were small. 33 Table X. Colon cancer patients. Median number of examined lymph nodes in the different Dukes’s stages for the three delay groups. Dukes’s A Dukes’s B Dukes’s C Dukes’s D Short delay 7 (12*) 8 (35) 9 (32) 7 (21) Median delay 6 (19) 8 (48) 9 (42) 9 (26) Long delay 3 (16) 9 (63) 9 (53) 9 (23) *Footnote as in previous table Table XI. Rectal cancer patients. Median number of examined lymph nodes in the different Dukes’s stages for the three delay groups Dukes’s A Dukes’s B Dukes’s C Dukes’s D Short delay 5 (10*) 8 (20) 6 (7) 10 (5) Median delay 9 (21) 8 (31) 12 (34) 8 (15) Long delay 6 (16) 10 (24) 9 (38) 10 (20) *Footnote as in previous table 34 The reviewed specimens were from all pathology departments participating in the project, and there were no substantial differences between the frequencies of reviewed specimens from the four pathology departments (table XII). Table XII. Numbers of specimens reviewed by each of the four participating pathology departments. Pathology Localization department of the cancer Esbjerg Colon Rectum Holstebro Colon Rectum Randers Colon Rectum Aarhus Colon Rectum Total Colon Rectum Included No consent Excluded Total 10 8 13 8 16 7 14 10 53 33 0 0 1 0 0 1 2 2 3 3 2 1 4 0 1 0 0 2 7 3 12 9 18 8 17 8 16 14 63 39 Colon and rectum combined 21 26 25 30 102 For 3/102 reviewed specimens, the Dukes’s stage was reclassified. In two of them, the reviewing pathologist found lymph nodes with metastases not found in the primary pathological examination; i.e. the patients were upstaged from Dukes’s B into Dukes’s C. One of these 2 patients was a rectal cancer patient included in the analyses and with a total diagnostic delay of 80 days. The patient changed from non-advanced stage into advanced stage, but that did not influence our results. The other patient had been excluded in the beginning of the study. In the third reclassified specimen, the reviewing pathologist found no evidence of tumor perforation of the muscularis propria thereby downstaging the lymph-node-negative patient from Dukes’s B to Dukes’s A. 35 3.2 Study II Study II, table 2 shows the 25th percentile, the median, the 75th percentile, and the 95th percentile of delays for colon cancer patients and rectal cancer patients included in the analysis. These were also stratified by age and gender. No substantial differences were seen except for patient delay. Therefore, the 25th percentile, the median, the 75th percentile, and the 95th percentile are only shown for patient delay (study II, table 3). Patient delay Colon cancer patients The median patient delay was 18 days, but variability was large: 25% of the patients had a patient delay of more than 3 months (study II, table 3). Female colon cancer patients had a longer patient delay than male patients, (study II, table 3). Patient delay was longer for patients aged 70 years than for patients aged >70 years (study II, table 3). Rectal cancer patients Median patient delay was 44 days, and 25% of patients had a patient delay of more than 115 days (study II, table 2). Less than half of the rectal cancer patients had a patient delay 30 days, and less than a third had a patient delay 7 days (study II, table 4). Men had longer patient delay than women. Patient delay was longer for patients 70 years than for patients >70 years (study II, table 4). General practitioner delay Colon cancer patients Median G.P. delay was short, but the range was wide and 25% of the patients had a G.P. delay of 59 days or more (study II, table 2). Less than half of the colon cancer patients were referred to a hospital specialist at first visit (study II, table 4), and the median number of visits to their family general practitioner was 2. Less than 10 percent of patients consulted a general practitioner on call, or went directly to the hospital. 36 Rectal cancer patients The median G.P. delay was short; 25% of the patients had a G.P. delay of 53 days or more (study II, table 2). Less than half of the patients were referred to the hospital at first visit (study II, table 4). Less than 5% of the rectal cancer patients never visited their family general practitioner but went to a general practitioner on call or directly to the hospital. Doctors’ delay of diagnosis Colon cancer patients The median doctors’ delay of diagnosis was 16 days (study II, table 2), which is not in accordance with current recommendations that diagnosis be made within 14 days of referral. Slightly more than one third of the patients had a delay of diagnosis of 14 days or less (study II, table 4). The patient’s family general practitioner was the first contact for the majority of the colon cancer patients, and over a half of them did not receive a rectal examination (data not shown). Rectal cancer patients The median doctors’ delay of diagnosis was 12 days (study II, table 2), but for 40% of the rectal cancer patients the fast track recommendations of a maximum of 14 days was not followed (study II, table 4). About one third of the rectal cancer patients who had contacted their family general practitioner first did not receive a rectal examination (data not shown). Delay of treatment Colon cancer patients The median delay of treatment was 9 days (study II, table 2); the 14-days postdiagnosis treatment recommendation was met for about three quarters of the patients (study II, table 4). For planned surgeries only, 65% of patients were operated within 14 days of diagnosis (data not shown). Rectal cancer patients The median delay of treatment was 15 days (study II, table 2) reflecting the fact that almost half of the patients received treatment according to the guidelines (study II, table 4). 37 Hospital delay Colon cancer patients Median hospital delay was 28 days (study II, table 2). If the emergency surgery cases were excluded from the analyses, the median hospital delay was 32 days. Rectal cancer patients Median hospital delay was 29 days (study II, table 2). Total delay Colon cancer patients Median total delay for colon cancer patients was 116 days (study II, table 2). Rectal cancer patients Median total delay for rectal cancer patients was 135 days (study II, table 2). 38 3.3 Study III Symptoms Vague and non-specific symptoms such as tiredness, weight loss, nausea, decreased appetite, and increased size of abdomen, were the most frequent onset symptoms for colon cancer patients. Those symptoms were also more commonly onset symptoms of colon cancer than of rectal cancer (study III, table 1). Rectal bleeding was the most frequent onset symptom of rectal cancer. Monosymptomatic rectal bleeding was the onset symptom for 18 percent of the rectal cancer patients. Fifty-four percent of the rectal cancer patients reported rectal bleeding as one of their onset symptoms. By comparison, only 26 percent of colon cancer patients presented rectal bleeding as one of their onset symptoms. Another frequent symptom of rectal cancer was change in bowel habits, which was reported by 20 percent of rectal cancer patients (study III, table 1). Symptoms and delay Study II, table 2 shows the association between onset symptom/symptom-complexes and diagnostic delay. For colon cancer patients, change in bowel habits, monosymptomatic abdominal pain, and vague symptoms as the onset symptom/symptom-complexes were associated with delay of longer than 150 days. For rectal cancer patients, monosymptomatic rectal bleeding as the onset symptom was associated with delay of 60 days or less. Symptoms and stage The vague unspecific symptoms were most frequent onset symptoms of colon cancer (study III, table 1), and they were associated with advanced cancer stage. (study III, table 3). Similarly to monosymptomatic rectal bleeding, rectal bleeding combined with other symptoms was a more frequent onset symptom among patients with non-advanced cancer than among patients with advanced cancer. This was true for both colon cancer patients and rectal cancer patients (study III, table 3). 39 Risk of advanced cancer was lower if onset symptoms were well defined than if they were vague and unspecific. Relative risk (95% CI) of advanced colon cancer for monosymptomatic rectal bleeding was 0.6, (CI: 0.5-1.0) and for rectal cancer, RR (95% CI) was 0.6 (0.4-0.9). Relative risk (95% CI) of having advanced cancer among patients with non-monosymptomatic rectal bleeding for those with diagnostic delay over 60 days was 0.7 (0.6-0.8) for both colon and rectal cancer patients (study III, table 4). 40 3.4 Study IV Correlation Of the 150 questionnaires sent to general practitioners, 149 (99.3%) were returned. Two returned questionnaires were not filled out (in one case, the G.P. retired, and in the other, patient ended up being seen by a G.P. on call). In 31 of the returned questionnaires, some of the dates were missing, most often, the date symptom(s) began. If only the month or the season and no exact date were given, we chose the median date of the month or the season. One hundred and sixteen questionnaires (77.3%) were complete and available for correlation analyses; 48 of them pertained to rectal cancer patients and 68, to colon cancer patients. The distribution of delay categories according to patient interviews and G.P. surveys is shown in Table XIII. Table XIII. Number (%) of patients in each delay group according to patients’ and G.P. questionnaires. Delay group Short delay All registered patients Colon cancer patients Rectal cancer patients N=116 N=68 N=48 Patient GP Patient GP Patient GP 23 28 16 22 7 6 (19.8) (24.1) (23.5) (32.4) (14.6) (12.5) Median delay 44 (37.9) 52 (44.8) 24 (35.3) 27 (39.7) 20 (41.7) 25 (52.1) Long delay 49 (42.2) 36 (31.0) 28 (41.2) 19 (27.9) 21 (43.8) 17 (35.4) Spearman’s Rank Correlation Test Spearman’s correlation coefficients are shown in Study IV, table 2. The coefficient for the correlation between the diagnostic delay reported by the patients and the general practitioners, varied from 0.27-0.60. The correlation was better for short delays ( 60 days) reported by the patients, than for median and long delay (> 60 days) reported by the patients (study III, table 2). 41 Altman’s plot According to the Altman’s plot, discrepancies between patient- and G.P.-reported delays were smaller for shorter delays than for longer delays. (figure IV). The Spearman’s correlation coefficient for the correlation showed in Altman’s plot was 0.42 (p<0.0001). Figure IV. Altman’s plot. Differences in the diagnostic delay (days) reported by the patients and the general practitioners are plotted against patient-reported delay. 42 4. Discussion Main conclusions Using population-based prospective design, we found that diagnostic delay was associated with the risk of having an advanced rectal cancer at time of treatment. However, the association for colon cancer was null. Diagnostic delay for rectal cancer tended to be longer than for rectal cancer in all delay categories, except doctors’ delay of diagnosis. G.P.-reported delay had short median value, but a wide range. Our data suggest that within-hospital adherence to current guidelines of diagnosis and treatment of patients with (suspected) colorectal cancer are not entirely met. A large proportion of patients referred to hospitals experience longer than 14-day wait until diagnostic procedures, and not all patients are treated within 14 days of establishment of diagnosis. G.P. does not always perform rectal examination on patients presenting with potential colorectal cancer symptoms. Nonspecific symptoms (tiredness, weight loss, nausea, decreased appetite and increased size of abdomen) were frequent symptoms of the onset of colon cancer, and having those vague symptoms was associated with a long diagnostic delay. Furthermore, the non-specific onset symptoms were associated with advanced cancer stage. Rectal bleeding was the most frequent onset symptom of rectal cancer. Monosymptomatic rectal bleeding was associated with short diagnostic delay for rectal cancer. For both colon cancer patients and rectal cancer patients, rectal bleeding was associated with nonadvanced tumor stage. The correlation between patient- and G.P.-reported diagnostic delay was moderate and discrepancies tended to become larger with longer delays. Methodological strengths and limitations To our knowledge, this is the largest study of diagnostic delay among colorectal patients conducted to date. The main strengths of our study are its large size, prospective design, 43 population-based setting within the uniformly organized tax-funded health care system, complete follow-up, and independent data collection on symptoms and delay (nurses’ interviews) on stage of the cancer (from surgical pathology reports). The limitations include the infeasibility of obtaining symptom onset data prospectively, increasing thereby the risk of recall bias among patients, in particular given vague and non-specific nature of the onset symptoms for colorectal cancer. We attempted to reduce the recall bias by conducting interviews before patients knew stage of tumor, which, however, was not always possible logistically. The vague and unspecific nature of the symptoms could have caused cancer-unrelated symptoms to be classified as onset symptoms and vice versa. Blinding both patient and interviewer to cancer stage achieve that any misclassification is non-differential, which, in turn, induces a downward bias of a positive relation. However, some patients may not have been blind to their tumor stage, which could cause differential misclassification of delay. There were 24 rectal cancer patients who received preoperative radiotherapy (1 Dukes’s A, 3 Dukes’s B, 11 Dukes’s C and 9 Dukes’s D) and for whom pathological staging of the specimens was downstaged due to the long preoperative radiotherapy treatment. These patients could have known their preoperative tumor stage, and judged their delays longer than they actually were (none of these patients were in the group of short delay). In addition, the interviewers could have known the preoperative stage for these patients. Similarly to other studies, we found that vague onset symptoms are typical for colon cancer often making it difficult to pinpoint its clinical onset. In contrast, rectal cancer tends to have well-defined symptoms, most notably, rectal bleeding (7;23;29;42;82;83). Thus misclassification of onset symptom date is more likely to occur among colon than among rectal cancer patients, which could partially explain that association between diagnostic delay and stage of cancer was seen so strongly for rectal cancer patients, but not for colon cancer patients (study I). 44 Biological differences may also explain the findings with some colon cancers being aggressive and quickly growing, as suggested by some studies (11;12;15). This is supported by observations that colon cancer patients often present as emergencies and are found to have advanced cancers, despite a short diagnostic delay. In study IV, correlation between patient- and G.P.-reported delay was moderate, with the greatest correlation observed with short delay, indicating that the validity of long delay values may be worse than that of short delay values. We have no golden standard of the true information of diagnostic delay, as there were likely imperfections with the patients’ data reporting as well as the general practitioners’ data reporting. We have no foundation to conclude whether the patients’ information or the general practitioners’ information provides a better estimate of onset symptom date. It is possible that data obtained by interviews in our study were more reliable than information reported by physician (based on patient complaints at the time of the visit). General population is not usually aware of colorectal cancer symptoms (40;41;70-74) and thus patients may not have reported particular symptoms unless specifically asked by physician. In our interviews, however, we systematically asked patients about each potential symptom of colorectal cancer. Patients might have better remembered long-lasting symptoms when prompted by an interviewer, which they may not have necessarily reported to physician. While reducing recall bias, this would not reduce misclassification since some long lasting symptoms are signs of benign disease prevalent in general population (25;26;28-33;35-40). The Altman plot may reflect this misclassification by showing a tendency of patients reporting a longer diagnostic delays (by remembering earlier symptoms when probed by interviewers) than do the general practitioners (who base their report on patient information at the time of the visit). In general, if the original answer was imprecise in the main study (study I) and in the correlation study (study IV), because only the month or the season was remembered, using the median date approximation for both patients and G.P.s also reduces the difference between the 45 diagnostic delay reported by the patients and the general practitioners. This causes better correlation for imprecise answers. We expect that the patients reported the same symptoms and date of onset of symptoms to their family general practitioners and to our interviewer, reducing the difference between the diagnostic delay reported by the patients and the general practitioners - information bias difficult or impossible to validate. Response rate among general practitioners was high. Missing were usually dates of onset of the symptoms as those were unknown to the general practitioner. There is no reason to believe that this caused selection bias, as the family general practitioners were unlikely to be aware of patients’ cancer stage, since the questionnaires were sent to the general practitioners in parallel to patient enrollment (study I). Discussion of delay A relation between diagnostic delay and stage may be an artifact the choice of boundaries for delay categories. Previous studies have examined the association between diagnostic delay and stage using values different from ours (table III) and may have used different analysis. To test the conjecture of interval-dependence of the results, we examined the association between diagnostic delay and stage using two different definitions of delay categories. We found that results did not change materially and interpretation remained the same for both colon cancer patients (no association) and rectal cancer patients (clear association). Previous studies (table III) reporting no association between diagnostic delay and stage (8-18;22;24) were often either small (8-17) or retrospective (8;11;13-18), and many of them did not analyze rectal cancer patients and colon cancer patients separately (8;9;12;15-17;22;24). None of these reported an association between diagnostic delay and stage. We believe it important to examine colon and rectal cancer separately to avoid masking of potential association between diagnostic delay and stage. As we and others have shown, frequency and nature of symptoms are different for the two cancers (7;23;29;42;82;83). The shorter median delay for colon cancer patients 46 compared with rectal cancer patients may be explained by the fact that colon cancer patients often (in about 20 percent of cases) present as emergencies (7;8;11;15). Discussion of stage Dukes’s stage was dichotomized into non-advanced cancers including Dukes’s A and B, and advanced cancers including Dukes’s C and D. We chose Dukes’s staging because it is the staging system most often used in previous studies examining the association between diagnostic delay and stage of colorectal cancer (7-21;24). (One study from 2004, examining the association between diagnostic delay and stage of the cancer at time of treatment (22), used the TNM classification, but divided the stages into four groups matching Dukes’s classification). The TNM classification – especially the new 6th edition (94) – is undoubtedly more reliable in predicting survival than Dukes’s classification (95). If patients with Dukes’s B and C were further classified into subgroups according to the T category (TNM staging), and to the number of lymph nodes with metastases*, a decreasing 5-year survival could be shown for patients in Dukes’s BII (TNM stage IIb) and patients in Dukes’s CI (TNM stage IIIa) (95). This may be due to the fact that adjuvant chemotherapy is offered to patients in Dukes’s stage C, but not to patients in Dukes’s stage B. Therefore the classification of stages as non-advanced and advanced, according to Dukes’s classification, might be imprecise, as it does not classify patients diagnosed as T4N0M0 with a poorer 5-year survival (95)as advanced stage. These patients would be classified as Dukes’s stage B. However, in our data, only 21 of the colon cancer patients and only 2 of the rectal cancer patients were classified as Dukes’s stage B, T4N0M0. These patients were, according to our classification of stage, classified as non-advanced. For rectal cancer, the two patients with Dukes’s stage B, T4N0M0, had diagnostic delays of 48 days (short delay), and 170 days (long delay). Assigning them into advanced stage did not affect the results. Dukes’s stage D at time of surgery was validated for all registered colorectal cancer patients by reviewing medical records (after the patients had left the hospital), resulting in 47 correction of 3.5% of stage information. The corrections usually stemmed from additional information about lung or liver metastases, or carcinosis found in the medical record. These corrections were performed before analyzing the data. The validation of a random sample of the specimens done by two independent pathologists were done after finishing the analyses, and served as a validation of the staging. In this thesis, 11% of the material was reviewed. The Dukes’s stage was reclassified in three of 102 cases (3%). None of the scarce previous studies of inter-observer variation on this issue (96-100) was conclusive. If the number of retrieved lymph nodes for patients in Dukes’s stage A and B is low, the risk of misclassification is high. An earlier study showed that if fewer than eight lymph nodes without metastases are identified in the specimen the statistical confidence of stage N0 is low (101;102). The confidence of correct staging, and thereby the prognosis of the 5-year survival, being dependent on the number of lymph nodes identified in the specimen (103), studies have suggested a minimum number of examined lymph nodes in the specimen for acceptable confidence of correct staging (101;102;104). Recommended number of lymph nodes varies across studies owing to differences in patient populations. In recent studies, 12 lymph nodes are suggested by Compton et al. (104), 13 lymph nodes are suggested by Swanson et al. (102), 17 lymph nodes are suggested by Mukai et al. (105) and 18 lymph nodes are suggested by Goldstein (101). The recommended number of lymph nodes identified in the specimen has been increasing during the last years (106). During the inclusion period of our study, Danish Society for Pathological Anatomy and Clinical Cytology recommended that at least 10 lymph nodes be identified (55). For participants of our project, the median number of lymph nodes in the specimen was fewer than 10. This indicates a risk of misclassification of the stage, but as the median number of lymph nodes in the specimen of the patients in the short delay groups were not substantially lower than the median number of lymph nodes in the specimen of the patients in the median and * Two subgroups for Dukes’s B, similar to TNM stage II (fourth and fifth edition), IIa and IIb, and three subgroups for 48 long delay groups, the misclassification is likely to be non-differential. The number of patients in the different delay groups with a known number of lymph nodes is very low in some cases. This increases the doubts about number of lymph nodes in the specimen serving as a predictor of the confidence of the stage. As expected, the number of rectal cancer patients with an advanced stage and a short delay, for whom the number of lymph nodes in the specimen was known, is low. This decreases the confidence of a correct stage for this group, but as metastases were seen in one or more lymph nodes; i.e., at least Dukes’s C if the stage is advanced, the risk of misclassification decreases. The misclassification stems from missed lymph nodes containing metastases. The median number of lymph nodes in the specimen of Dukes’s stage A is very low. Some adenocarcinomas within polyps were classified into Dukes’s stage A, with number of lymph nodes classified as “unknown” if the patient was deemed curatively resected by the endoscopic polypectomy. All patients treated by TEM (transanal endoscopic microsurgery) were Dukes’s stage A. Staging of patients with adenocarcinoma within polyps or patients treated by TEM cannot be done according to Dukes’s stage, as no resection is done. Lymph nodes with metastases are very seldom for these patients; in our study, it was known for a single patient. Patient delay and demographics We found that patient delay was the longest component of the total diagnostic delay (study II). Rectal cancer patients had longer median patient delay than did colon cancer patients, which is similar to previous studies (7;12;23;107). This is not expected, as symptoms of rectal cancer are often better defined, though still nonspecific, than symptoms of colon cancer (study III) (12;21;23;42;51;82). Rectal bleeding is a well defined symptom and, as our study III confirmed, is the most frequent onset symptom of rectal cancer (17;23;67). However, patients often do not seek care for rectal bleeding (26;40;41;108). Similarly, patients tend not to seek care for frequent symptoms of colon cancer (23;67): abdominal pain, constipation, or diarrhea (25;28;29;41). Length Dukes’s C, similar to TNM stage III (fourth and fifth edition) IIIa, IIIb, and IIIc. 49 of patient delay depends not only on patients’ experience of the symptoms, but also on the patients’ knowledge of the significance of symptoms (12;26;29;41;83;108;109). Previous studies have shown that the general population’s knowledge of colorectal cancer symptoms is often limited (40;41;7074), explaining the long duration of patient delay. There are gender differences in knowledge about colorectal cancer symptoms. Men tend to be less knowledgeable than women (70;71), explaining longer delays observed in men (study II). Paradoxically, women with colon cancer had a substantially longer patient delay than men. Partial explanation may be in gender-specific frequencies of symptoms. In our study, more women then men presented with vague symptoms that could signal onset of both colon and rectal cancer (28% of the women vs.19% of the men for colon cancer, 4% of the women vs. 2% of the men for rectal cancer). Study III showed that patients with very vague onset symptoms of CRC, more often had a long diagnostic delay. Another remarkable finding (study II) was that older patients (>70 years) had a shorter patient delay than the younger patients (70 years). Old patients may be generally more likely than younger patients to visit physicians for chronic conditions, which provides more opportunities for physicians to learn about potential colorectal cancer symptoms. However, previous studies found that patients do not always tell their family general practitioner about other symptoms at routine check-up visits (68;69). In our population of interviewed colorectal cancer patients, the distribution of men and women in the two age groups was different. For colon cancer patients the proportion of men was higher among young patients (men/women: 55% vs. 45%), whereas the proportion of women was higher among the old patients (men/women: 47% vs. 53%). It is strange that old colon cancer patients had a shorter patient delay than young colon cancer patients if the proportion of women (more often presenting with the very vague symptoms associated with a long delay) in the old age group was higher than the proportion of men. 50 General practitioner delay (study II) The median G.P. delay was short in this study seemingly indicating that this part of the diagnostic delay needs no improvement. At the same time, it cannot be discounted that 25 percent of the colon cancer patients had a G.P. delay of 59 days or more, and 25 percent of the rectal cancer patients had a G.P. delay of 53 days or more. The G.P. delay is affected by patient behavior, as patients not referred for further examination at first visit, may not see the G.P. for a long time, increasing the delay. If the patient waits a long time before seeking care again, delay for continuous symptoms will be classified as G.P. delay. Colorectal cancer is difficult to diagnose from symptoms alone, and the nonspecificity of CRC symptoms unquestionably leads to diagnostic delay. Studies have attempted to promote guidelines for examination of patients with gastrointestinal symptoms distinguishing between those high and low risk of CRC, but have still come to no final conclusion (25;41-48). However, it has been shown that strict compliance with the guidelines improves CRC detection rate (90;110). As earlier studies, we found that rectal examination was not routinely performed before referral to the hospital (23;67;81;84;111;112). It is an easy, inexpensive, and informative examination and, according to the guidelines of the Danish Colorectal Cancer Group (47) (figure II), it should be performed during the mandatory examinations of patients with gastrointestinal symptoms. In study II, we found that one third of the rectal cancer patients were not examined by rectal examination, although approximately two thirds of all rectal cancers can be diagnosed by rectal examination. Less than half of the rectal cancer patients were referred for follow-up at a hospital at the first G.P. visit. At the same time, our study was based solely on the patients’ account of examinations. The patients – particularly the elderly – may not remember exactly whether examinations were done by their family general practitioner or at the hospital. Therefore, the frequency of patients who received a rectal examination at the general practitioner might not be correct. The rectal 51 examination reported as having been done by a G.P. could actually be performed at the hospital. Thus, the number of rectal exams performed at G.P. office could be misclassified. Discussion of doctors’ delay of diagnosis (study II) We did not have access to the text of referrals, which could be important in assessing whether general practitioner or hospital was responsible for delay of diagnosis. Wheeler et al. (61) found (and Read-Jones confirmed (88)) diagnostic delay reduced if CRC was mentioned on the referral because guidelines require booking endoscopic examination within 14 days for suspected CRC, whereas if a cancer is not suspected, it is acceptable to wait longer. The better the patient is examined according to the guidelines before referral to the hospital, the better defined and informative the referral can be. Doctors’ delay of diagnosis may be caused by lack of hospital resources for examinations of referred patients, leading to prolonged waiting period for endoscopies. We confirmed a Swedish study (84) finding a longer delay of diagnosis for colon cancer patients than for rectal cancer patients. In the Swedish study, it was due to a long waiting period for colonoscopy or barium enemas. Rectal cancer can be diagnosed by sigmoidoscopy, which has a shorter waiting period than colonoscopy. Further, a patient with symptoms indicating the need for colonoscopy first referred for sigmoidoscopy must, after the clean sigmoidoscopy, wait for colonoscopy in order for a right-sided colon cancer to be diagnosed. In our study 48 (11%) of the colon cancer patients were diagnosed by sigmoidoscopy, and 265 (58%) of the colon cancer patients were diagnosed by colonoscopy. We do not know how many of the patients were initially referred for a sigmoidoscopy, and had to wait for a colonoscopy. Missed diagnosis of CRC at first examination is another reason for delay of diagnosis, especially if the first examination is a barium enema (10;12;21). Since most hospitals in our study only examined patients by endoscopy (66 (14%) colon cancer patients were diagnosed by barium enemas), this problem is hardly the most important, but diagnosis can still be missed at endoscopy, which could delay diagnosis considerably (23;113;114). 52 Mistakes in booking systems and missed letters to the patients can be causes of delay of diagnosis at the fault of the hospitals. Finally, patients might themselves postpone diagnostic work-up (67;84). Discussion of delay of treatment Delay of treatment is caused by the hospitals and should be avoided as much as possible. Rarely is delay of treatment caused by patients’ comorbidity indicating treatment for another disease before surgery is possible. Patients hospitalized in non-surgery departments, in whom colorectal cancer is diagnosed by chance during examinations for other diseases, will experience longer delays of treatment, as they will typically be first treated for the disease which caused the hospitalization (54). Usually delay of treatment is a function of lack of resources – financial or manpower – if colorectal cancer patients must wait for the start of treatment for more than 14 days after diagnosis (67;84;89;90). The 24 included rectal cancer patients who received preoperative radiotherapy had a substantially longer median delay of treatment than all included rectal cancer patients (35 days vs. 15 days), indicating that preoperative radiotherapy may also cause unacceptably long delay of treatment. Discussion of total delay Total delay was longer for rectal cancer patients than for colon cancer patients, and so were all components of total delay, except for the doctors’ delay of diagnosis, which can partly be explained by the frequent emergency surgery of colon cancers (doctors’ delay of diagnosis is virtually absent), and partly by the fact that a rectal cancer can be diagnosed by sigmoidoscopy and never indicates waiting for a colonoscopy afterwards. Problems with symptoms and recommendations For most patients with changes in bowel habits as CRC onset symptom, it is unrealistic to expect a short (<60 days) total delay, as according to the guidelines, endoscopy is not 53 indicated until the changes in bowel habits have lasted for at least 30 days, (4;47). However, a short delay can be expected for patients with rectal bleeding as onset symptom, since it is well defined, (albeit non-specific). Even if rectal bleeding has low positive predictive value for colorectal cancer, (26;27;34;43;45;46;64-67), screening all patients with this symptom may improve survival by allowing cancer diagnosis at early stage – the most important prognostic factor (5;6). 54 5. Conclusions We found a strong association between diagnostic delay and stage of the cancer at time of operation for rectal cancer, but not for colon cancer. This finding is important as it opens possibility for improvement of survival of rectal cancer patients by diagnosing tumors while they are in Dukes’s stages A or B. Our findings suggest that all components of diagnostic delay need improvement with patient delay being particularly long. Population should be educated about symptoms of CRC and prompt care seeking. Patient delay was longer for rectal cancer than for colon cancer. Given our findings of strong association between diagnostic delay and stage for rectal cancer, it is particularly important to reduce patient delay in rectal cancer cases. More than 50 percent of the rectal cancer patients presented rectal bleeding as onset symptom. It may be warranted to fast-track patients with this well defined symptom for further diagnostic workup. General practitioners must thoroughly examine every patient suspected of CRC according to the guidelines and mention the suspicion of CRC on the hospital referral. The hospitals, in turn, should provide timely endoscopy and mobilize resources to start CRC treatment within 14 days of diagnosis. Colon cancer tended to present with unspecific and vague symptoms, while rectal cancer was more likely to present with better defined symptoms, such as rectal bleeding – monosymptomatic or as a part of symptom constellation – which was also the most frequently reported symptom. Our study provided additional evidence for inverse association between presence of rectal bleeding and CRC stage (22;27;31;115), suggesting that rectal bleeding is an early symptom, once more underscoring the importance of patient education. We found that correlation between patient- and general-practitioner-reported delay moderate, and decreased as delay increased. In conclusion, the association between diagnostic delay and stage of rectal cancer at time of surgery has important policy implications for improving survival. Effective strategies must 55 be found to reduce diagnostic delay caused by patients with symptoms, general practitioners making referrals, and specialists at hospitals who perform diagnostic procedures and treatment. 56 6. Perspectives Stage of colorectal cancer at time of treatment is the most important prognostic factor (5;6). We showed a strong association between diagnostic delay and stage of rectal cancer, which makes us expect an association between diagnostic delay and mortality. Thus, association between diagnostic delay and mortality is an important research direction. Education of patients about CRC symptoms and dedicating more hospital resources to timely diagnostic procedures are important for reducing diagnostic delay. G.P. delay may be reduced if recommendations on the referral are better followed. A targeted analysis of the G.P. delay could include analysis of specific information in the referral letter, as well as how closely recommendations for follow-up are fulfilled. In general, a more effective diagnostic strategy must be developed insuring co-operation between the general practitioners and the hospitals. Danish patients with colorectal cancer have poorer prognosis than their Norwegian and Finnish counterparts. A targeted comparison of diagnostic delay in Danish, Finnish, and Norwegian patients would help elicit reasons for the worse prognosis among Danes. 57 7. Summary Background: Denmark has a high incidence of colorectal (CRC) cancer with CRC mortality higher than in other Scandinavian countries. The association between diagnostic delay, symptoms of CRC, and stage of cancer at time of operation is controversial. In 1998, the Danish Government issued ‘fast-track’ recommendation that patients suspected of having CRC should be diagnosed within 14 days from referral, and treated within another 14 days. We aimed to examine the association between diagnostic delay, onset symptoms, and stage of CRC. We examined how patients, the general practitioners (G.P.), and the hospitals contribute to the diagnostic delay. We also examined if the fast track recommendations were met. Finally, we examined the correlation between patients’ self-reported diagnostic delay and their general practitioners’ recorded diagnostic delay data. Material and method: We did a prospective population-based observational study of colorectal cancer patients from three counties (13 hospitals) in Denmark. Information on symptoms and their onset dates were obtained through in-hospital patient interviews; the data on Dukes’s stage were obtained through pathology reports and medical records. The inclusion criteria (histologically verified adenocarcinoma of the colon or rectum, and patient resided in our inclusion counties) were fulfilled by 951 primary CRC patients. Sixty-one patients refused to participate, and 147 patients were excluded due to death, inability to cooperate, or ineligibility. To examine the association between diagnostic delay (defined as the interval from onset of symptoms and start of treatment) and stage, we calculated the frequencies of patients with short diagnostic delay ( 60 days), median delay (61-150 days), and long diagnostic delay (> 150 58 days) according to non-advanced stage (Dukes’s stage A or B) and advanced stage (Dukes’s stage C or D). We estimated the relative risk of having an advanced cancer for patients with median and long diagnostic delay, with short diagnostic delay as our reference group. We stratified according to age, gender, and elective or emergency surgery. Total delay was divided into three groups: “patient delay”, “G.P. delay”, and “hospital delay”. The latter was divided into “doctors’ delay of diagnosis” and “delay of treatment”. We analyzed the data first by constructing contingency tables for the main study variables; age, gender, elective, or emergency surgery, and delay- periods. We calculated the percentiles of delay for all included patients and stratified according to age and gender. We calculated the frequency of patients for whom the recommendations of the Danish Government were met. We defined eight groups according to onset symptom. The groups represented the most frequent onset monosymptomatic symptoms and symptom-complexes; (i) monosymptomatic rectal bleeding, (ii) rectal bleeding and others, (iii) change in bowel habits, (iv) monosymptomatic abdominal pain, (v) very vague symptoms (abdominal pain included), (vi) monosymptomatic anemia, (vii) anemia and others, and (viii) others. We calculated frequencies of patients with these first symptoms and first symptomcomplexes for colon cancer patients and rectal cancer patients separately. We analyzed the association between onset symptoms/symptom complexes and diagnostic delay by obtaining contingency tables of the numbers and frequencies of patients with the different onset symptoms/symptom-complexes for patients with short delay, median delay, and long delay. We calculated the association between the most frequent onset symptoms/symptom-complexes and having an advanced stage of cancer at time of treatment by obtaining relative risk and 95% confidence intervals (CI). To examine the correlation between the patients’ and the general practitioners’ information about diagnostic delay, we randomly selected 150 patients (20%), who primary 59 contacted their family G.P., and sent a questionnaire with the same questions about diagnostic delay to the general practitioner (149 of the questionnaires were returned; 116 (77.3%) were completed). The patients’ information and the general practitioner’s information were compared by Spearman’s Rank Correlation Test and Altman’s plot. All analyses were performed separately for colon and rectal cancer patients. Results: We found no association between diagnostic delay and stage for colon cancer. For rectal cancer, we found an almost two-fold increased in risk of advanced caner for diagnostic delay lasting longer than 60 days compared with delays up to 60 days. Patient delay was the longest delay component for both colon and rectal cancer patients, though the delay for rectal cancer was longer (18 days vs. 44 days). Median G.P. delay was short but had a wide range. Twenty-five percent of the colon cancer patients had a G.P. delay of 59 days or more, and 25% of the rectal cancer patients had a G.P. delay of 53 days or more. The fast track recommendations were poorly met. Median total delay was long for both colon cancer and rectal cancer (116 days vs. 135 days). All delay periods were longer for rectal cancer than for colon cancer with the exception of delay of diagnosis. The vague and unspecific symptoms were more frequently onset symptoms of colon cancer, and they were associated with advanced cancer stage. For rectal cancer, the most frequent onset symptom was the well defined rectal bleeding, either monosymptomatic or combined with other symptoms. For rectal cancer patients, monosymptomatic rectal bleeding as the onset symptom/symptom-complex was associated with short diagnostic delay and with non-advanced stage of cancer for colon cancer and for rectal cancer. The correlation between G.P.-recorded and patient-reported data on the timing of symptoms onset was moderate (Spearman’s correlation coefficient: 0.27-0.60). Correlation was better for shorter delays than for longer delays. Altman’s plot showed a tendency towards patients 60 reporting longer delay than did the general practitioners. Spearman’s correlation coefficient for the correlation illustrated by Altman’s plot was 0.42, p<0.0001 Conclusions: We found a strong association between diagnostic delay and stage for rectal cancer, but not for colon cancer. All aspects of the diagnostic delay need to be shortened. Avenues of improvement include patient education and dedicating more hospital resources to timely diagnosis and treatment of colorectal cancer. Onset symptoms of rectal cancer are better defined than onset symptoms of colon cancer. Rectal bleeding – the most frequent symptom of rectal cancer – was associated with earlier cancer stage, indicating that rectal bleeding is an early CRC symptom. The correlation between the information of diagnostic delay from the patients and the patients’ general practitioners was moderate and was inversely related to the length of patientreported diagnostic delay. 61 8. Danish summary Baggrund: Danmark har en høj incidens af colorectal cancer (CRC), og dødeligheden er højere end i de øvrige skandinaviske lande. Det er uafklaret, om der er en sammenhæng mellem diagnostisk delay og stadie af cancer på operationstidspunktet. Symptomerne for CRC er ofte uspecifikke og vage. I 1998 udgav den danske regering anbefalinger om, at patienter med symptomer, der giver mistanke om CRC, skal undersøges med henblik på diagnose inden for 14 dage og derefter behandles senest 14 dage efter at diagnosen er stillet – 14-dages garantien. Formålet med studiet var at undersøge sammenhængen mellem diagnostisk delay (defineret som perioden fra symptom-start til behandlings-start) og stadie af CRC, at undersøge hele perioden fra symptom-start til behandlings-start opdelt i patient-delay, egen læge-delay og sygehus-delay, herunder at undersøge, om 14-dages reglen blev overholdt. Desuden ønskede vi at undersøge sammenhængen mellem symptomer og diagnostisk delay og mellem symptomer og stadie af CRC. Slutteligt ønskede vi at undersøge korrelationen mellem patienternes information om diagnostisk delay og deres egen læges information om diagnostisk delay. Materiale og metode: En prospektiv interviewbaseret spørgeskemaundersøgelse af en kohorte på 951 CRC patienter fra 3 amter (13 sygehuse) i Vestdanmark. Disse er repræsentative for befolkningssammensætningen i Danmark. I alt 951 primære CRC patienter opfyldte inklusionskriterierne (histologisk verificeret adenocarcinom i colon eller rectum og patienten bosiddende i vores inklusionsområde), og 743 patienter (78,1 %) medvirkede ved spørgeskema-interviewet. Kun 61 patienter (6,4 %) ønskede ikke at deltage, og 147 patienter (15,5 %) blev ekskluderet pga. mors, demens eller manglende kooperationsevne, eller fordi de ikke var dansk talende. Derudover ekskluderede vi de patienter, der 62 gik til coloskopi-kontrol pga. øget risiko for CRC; patienter med HNPCC, FAP, AFAP og kronisk inflammatorisk tarmsygdom. Spørgeskema-interviewene omhandlede symptomer, oplysninger om diagnostisk delay og en række alment sundhedsmæssige og sociale karakteristika. Stadie af tumor ved operation blev klassificeret ud fra det nationale patologiskema for CRC og suppleret med journaloplysninger især mhp rigtig klassifikation af patienter med Dukes´ stadie D. Patienterne blev inddelt i 3 grupper: patienter med kort diagnostisk delay ( 60 dage), middel diagnostisk delay (61-150 dage) og langt diagnostisk delay (> 150 dage). Mht stadie inddelte vi patienterne i 2 grupper: patienter med ikke-avanceret stadie (Dukes’s stadie A og B) og patienter med avanceret stadie (Dukes’s stadie C og D). Frekvensen af patienter med ikke-avanceret cancer og avanceret cancer er beregnet for alle 3 diagnostisk delay grupper. Vi beregnede den relative risiko for avanceret cancer ved middel diagnostisk delay og langt diagnostisk delay med gruppen af patienter med kort diagnostisk delay som reference-gruppe. Diagnostisk delay blev opdelt i ”patient delay”, ”egen læge delay” og ”hospitals delay”, som yderligere blev opdelt i ”diagnose delay” og ”behandlings delay”. Vi udregnede 25% percentilen, medianen, 75% percentilen og 95% percentilen for alle delay perioder og stratificerede på køn og alder. Derudover udregnede vi andelen af patienter, der havde ”patient delay” på 7 dage og på 30 dage, og andelen af patienter, der havde ”egen læge delay” på ingen eller 1 dag, hvilket vi satte lig med at, de var henvist ved første besøg. Vi valgte intervaller, som vi skønnede var af en varighed, som gjorde det realistisk af holde diagnostisk delay på maximalt 60 dage under forudsætning af, at 14-dags garantien blev overholdt. Vi belyste ”egen læge delay” ved at se på egen læges reaktion på de symptomer, patienterne præsenterede, og så på egen læges undersøgelser før henvisning til videre udredning. Frekvensen af patienter, for hvem 14dags reglen blev overholdt, blev opgjort. Alle analyser er lavet med colon cancer patienter og rectum cancer patienter hver for sig. 63 Vi definerede 8 symptom-grupper med de hyppigste debut-symptomer, enten monosymptomatiske eller symptom-kompleker. Grupperne bestod af: (i) monosymptomatisk rectal blødning, (ii) rectal blødning kombineret med andre symptomer, (iii) ændringer i afføringsvaner, (iv) monosymptomatiske mavesmerter, (v) meget vage symptomer (incl. mavesmerter), (vi) monosymptomatisk anæmi, (vii) anæmi kombineret med andre symptomer, og en gruppe med (viii) resten - kaldet andre symptomer. Vi udregnede antallet af patienter og frekvensen af patienter, der havde de forskellige debut-symptomer eller debut symptom-komplekser for henholdsvis colon cancer patienter og rectum cancer patienter. Vi kortlagde antallet og andelen af colon cancer patienter og rectum cancer patienter med de forskellige debut-symptomer/debut symptom-komplekser i de 3 delay grupper: kort delay, middel delay og langt delay. Sammenhængen mellem debut-symptomer/debut-symptom-komplekser og stadie blev analyseret ved at udregne den relative risiko (med confidens-intervaller) for at have avanceret stadie på operationstidspunktet for de forskellige debut-symptomer/debut-symptom-komplekser. Igen blev analyserne lavet for colon cancer patienter og rectum cancer patienter hver for sig. Korrelationen mellem patienternes information om diagnostisk delay og egen læges information om diagnostisk delay er undersøgt: Der udvalgtes tilfældigt 150 patienter (20%), der primært havde søgt egen læge (ca. 90 % af patienterne), og egen læge fik tilsendt et spørgeskema om diagnostisk delay (149 skemaer returneret; > 99 %, 116 komplette 77,3 %). Overensstemmelsen mellem patienternes oplysninger om diagnostisk delay og egen læges oplysninger om diagnostisk delay er beregnet ved Spearman’s Rank Korrelations Test og Altman’s plot er tegnet. Spearman’s rho for korrelationen illustreret ved Altman’s plot er beregnet. Resultater: 64 Studie I: Der fandtes ingen sammenhæng mellem diagnostisk delay og stadie for colon cancer. For rectum cancer fandtes en væsentlig sammenhæng mellem diagnostisk delay og stadie, således at risikoen for avanceret cancer (Dukes´ stadie C eller D) ca. er fordoblet ved et diagnostisk delay over 60 dage Studie II: Median “patient delay“ var den længste delay periode for både colon cancer patienter og rectum cancer patienter, dog noget længere for rectum cancer patienter (18 vs. 44 dage). Median ”egen læge delay” var kort, men med en enormt stor range. 25% af colon cancer patienterne havde en ”egen læge delay” på 59 dage eller mere, og 25% af rectum cancer patienterne havde en ”egen læge delay” på 53 dage eller mere. 14-dages garantien blev dårligt overholdt. Median ”total delay” var lang for både colon cancer patienter og rectum cancer patienter (116 vs. 135 dage). Alle delay perioder bortset fra ”diagnose delay” var længere for rectum cancer end for colon cancer. Studie III: De mest vage symptomer var hyppigere debut-symptom ved colon cancer end ved rectum cancer, og de var associeret med avanceret stadie, mens de mere konkrete symptomer var hyppigste debut-symptom ved rectum cancer. Blødning pr. rectum, enten monosymptomatisk eller kombineret med andre symptomer, var det mest hyppige debut-symptom for rectum cancer. Monosymptomatisk rectal blødning var for rectum cancer patienter associeret med kort delay. For såvel colon cancer som rectum cancer patienter var både monosymptomatisk rectal blødning og rectal blødning kombineret med andre symptomer associeret med ikke-avanceret cancer. Studie IV: Spearman’s rho korrelations koefficient varierede fra 0,27 til 0,60, og var således ikke helt perfekt. Både Spearman’s Rank Korrelations Test og Altman’s plot viste, at patienternes og lægernes information om diagnostisk delay korrelerede bedst for kort delay. Altman’s plot viste yderligere en tendens til, at patienterne rapporterer længere diagnostisk delay end lægerne. Spearman’s rho for korrelationen illustreret ved Altman’s plot var 0,42, p<0.0001. 65 Konklusion: Studie I: Der fandtes en væsentlig sammenhæng mellem diagnostisk delay og stadie for rectum cancer, hvorimod dette ikke var tilfældet for colon cancer. Fremtidige undersøgelser må vise, om dette, som forventet, også afspejler sig i en forskel i dødelighed ved rectum cancer. Studie II: Alle aspekter af diagnostisk delay må forbedres. Patienterne skal informeres bedre om symptomer på CRC og vide, at de skal søge læge for dem. Egen læge skal undersøge hver patient med symptomer på CRC efter anbefalingerne, og dette skal føre til en hurtig tid til videre udredning, hvis der er indikation for det. Hospitalerne skal have ressourcer til at kunne imødekomme 14-dages garantien bedre. Studie III: De vage symptomer var hyppigere for colon cancer patienter end for rectum cancer patienter, og de var associeret med avanceret cancer. Hyppigste debut-symptomer på rectum cancer var mere konkrete, og det hyppigste debut-symptom på rectum cancer var rectal blødning især som symptom kombineret med andre symptomer. For rectum cancer patienter var rectal blødning associeret med kort delay. Rectal blødning var associeret med ikke-avanceret cancer for både colon cancer og rectum cancer. Studie IV: Korrelationen mellem patienternes og lægernes oplysninger om diagnostisk delay var ikke helt perfekt og viser vanskeligheden af at indsamle prospektive data vedr. symptom-debut. Korrelationen var bedst for kort delay. Undersøgelsen er en del af større pågående prospektive undersøgelser, der for CRC sammenligner diagnostisk delay, stadium og dødelighed i Danmark, Norge og Finland. 66 9. References 1. Pisani P, Parkin DM, Ferlay J. Estimates of the worldwide mortality from eighteen major cancers in 1985. Implications for prevention and projections of future burden. Int.J.Cancer 1993;55(6):891-903. 2. Pisani P, Parkin DM, Bray F, Ferlay J. Estimates of the worldwide mortality from 25 cancers in 1990. Int.J.Cancer 1999;83(1):18-29. 3. Edwards BK, Howe HL, Ries LA, Thun MJ, Rosenberg HM, Yancik R et al. Annual report to the nation on the status of cancer, 1973-1999, featuring implications of age and aging on U.S. cancer burden. Cancer 2002;94(10):2766-92. 4. Statens Institut for Medicinsk Teknologivurdering. Kræft i tyktarm og endetarm. Diagnostik og screening. Medicinsk Teknologivurdering. Medicinsk Teknologivurdering 2001. 5. Deans GT, Parks TG, Rowlands BJ, Spence RA. Prognostic factors in colorectal cancer. Br.J.Surg. 1992;79(7):608-13. 6. Clinico-pathological features of prognostic significance in operable rectal cancer in 17 centres in the U.K. (Third report of the M.R.C. Trial, on behalf of the Working Party). Br.J.Cancer 1984;50(4):435-42. 7. Arbman G, Nilsson E, Storgren-Fordell V, Sjodahl R. A short diagnostic delay is more important for rectal cancer than for colonic cancer. Eur.J.Surg. 1996;162(11):899-904. 8. Kyle SM, Isbister WH, Yeong ML. Presentation, duration of symptoms and staging of colorectal carcinoma. Aust.N.Z.J.Surg. 1991;61(2):137-40. 9. Ratcliffe R, Kiff RS, Hoare EM, Kingston RD, Walsh SH, Jeacock J. Early diagnosis in colorectal cancer still no benefit? Ann.Chir 1989;43(7):570-4. 10. Graffner H, Olsson SA. Patient's and doctor's delay in carcinoma of the colon and rectum. J.Surg.Oncol. 1986;31(3):188-90. 11. Pescatori M, Maria G, Beltrani B, Mattana C. Site, emergency, and duration of symptoms in the prognosis of colorectal cancer. Dis.Colon Rectum 1982;25(1):33-40. 12. Holliday HW, Hardcastle JD. Delay in diagnosis and treatment of symptomatic colorectal cancer. Lancet 1979;1(8111):309-11. 13. Devlin HB, Plant JA, Morris D. The significance of the symptoms of carcinoma of the rectum. Surg.Gynecol.Obstet. 1973;137(3):399-402. 14. Goodman D, Irvin TT. Delay in the diagnosis and prognosis of carcinoma of the right colon. Br.J.Surg. 1993;80(10):1327-9. 15. Irvin TT, Greaney MG. Duration of symptoms and prognosis of carcinoma of the colon and rectum. Surg.Gynecol.Obstet. 1977;144(6):883-6. 67 16. Jolly KD, Scott JP, MacKinnon MJ, Clarke AM. Diagnosis and survival in carcinoma of the large bowel. Aust.N.Z.J.Surg. 1982;52(1):12-6. 17. Khubchandani M. Relationship of symptom duration and survival in patients with carcinoma of the colon and rectum. Dis.Colon Rectum 1985;28(8):585-7. 18. McDermott FT, Hughes ES, Pihl E, Milne BJ, Price AB. Prognosis in relation to symptom duration in colon cancer. Br.J.Surg. 1981;68(12):846-9. 19. Pahlman L, Glimelius B, Enblad P. Clinical characteristics and their relation to surgical curability in adenocarcinoma of the rectum and rectosigmoid. A population-based study on 279 consecutive patients. Acta Chir Scand. 1985;151(8):685-93. 20. Robinson E, Mohilever J, Zidan J, Sapir D. Colorectal cancer: incidence, delay in diagnosis and stage of disease. Eur.J.Cancer Clin.Oncol. 1986;22(2):157-61. 21. Rowejones DC, Aylett SO. Delay in treatment in carcinoma of colon and rectum. Lancet 1965;2(7420):973-6. 22. Gonzalez-Hermoso F, Perez-Palma J, Marchena-Gomez J, Lorenzo-Rocha N, Medina-Arana V. Can early diagnosis of symptomatic colorectal cancer improve the prognosis? World J Surg. 2004;28(7):716-20. 23. Langenbach MR, Schmidt J, Neumann J, Zirngibl H. Delay in treatment of colorectal cancer: multifactorial problem. World J.Surg. 2003;27(3):304-8. 24. Bharucha S, Hughes S, Kenyon V, Anderson ID, Carlson GL, Scott NA. Targets and elective colorectal cancer: outcome and symptom delay at surgical resection. Colorectal Dis. 2005;7(2):169-71. 25. Selvachandran SN, Hodder RJ, Ballal MS, Jones P, Cade D. Prediction of colorectal cancer by a patient consultation questionnaire and scoring system: a prospective study. Lancet 2002;360(9329):278-83. 26. Byles JE, Redman S, Hennrikus D, Sanson-Fisher RW, Dickinson J. Delay in consulting a medical practitioner about rectal bleeding. J.Epidemiol.Community Health 1992;46(3):2414. 27. Goulston KJ, Cook I, Dent OF. How important is rectal bleeding in the diagnosis of bowel cancer and polyps? Lancet 1986;2(8501):261-5. 28. Kay L, Jorgensen T, Schultz-Larsen K. Abdominal pain in a 70-year-old Danish population. An epidemiological study of the prevalence and importance of abdominal pain. J.Clin.Epidemiol. 1992;45(12):1377-82. 29. MacDonald L, Freeling P. Bowels: beliefs and behaviour. Fam.Pract. 1986;3(2):80-4. 30. Dent OF, Goulston KJ, Zubrzycki J, Chapuis PH. Bowel symptoms in an apparently well population. Dis.Colon Rectum 1986;29(4):243-7. 31. Goulston K, Chapuis P, Dent O, Bokey L. Significance of bowel symptoms. Med.J.Aust. 1987;146(12):631-3. 68 32. Chapuis PH, Goulston KJ, Dent OF, Tait AD. Predictive value of rectal bleeding in screening for rectal and sigmoid polyps. Br.Med.J.(Clin.Res.Ed) 1985;290(6481):1546-8. 33. Curless R, French J, Williams GV, James OF. Comparison of gastrointestinal symptoms in colorectal carcinoma patients and community controls with respect to age. Gut 1994;35(9):1267-70. 34. Metcalf JV, Smith J, Jones R, Record CO. Incidence and causes of rectal bleeding in general practice as detected by colonoscopy. Br.J.Gen.Pract. 1996;46(404):161-4. 35. Kay L, Jorgensen T, Jensen KH. The epidemiology of irritable bowel syndrome in a random population: prevalence, incidence, natural history and risk factors. J.Intern.Med. 1994;236(1):23-30. 36. Farrands PA, Hardcastle JD. Colorectal screening by a self-completion questionnaire. Gut 1984;25(5):445-7. 37. Thompson WG, Heaton KW. Functional bowel disorders in apparently healthy people. Gastroenterology 1980;79(2):283-8. 38. Farrands PA, Hardcastle JD, Chamberlain J, Moss S. Factors affecting compliance with screening for colorectal cancer. Community Med. 1984;6(1):12-9. 39. Silman AJ, Mitchell P, Nicholls RJ, Macrae FA, Leicester RJ, Bartram CI et al. Selfreported dark red bleeding as a marker comparable with occult blood testing in screening for large bowel neoplasms. Br.J.Surg. 1983;70(12):721-4. 40. Cockburn J, Paul C, Tzelepis F, McElduff P, Byles J. Delay in seeking advice for symptoms that potentially indicate bowel cancer. Am.J Health Behav. 2003;27(4):401-7. 41. Hamilton W, Sharp D. Diagnosis of colorectal cancer in primary care: the evidence base for guidelines. Fam.Pract. 2004;21(1):99-106. 42. Majumdar SR, Fletcher RH, Evans AT. How does colorectal cancer present? Symptoms, duration, and clues to location. Am.J.Gastroenterol. 1999;94(10):3039-45. 43. Farrands PA, O'Regan D, Taylor I. An assessment of occult blood testing to determine which patients with large bowel symptoms require urgent investigation. Br.J.Surg. 1985;72(10):835-7. 44. Segal WN, Greenberg PD, Rockey DC, Cello JP, McQuaid KR. The outpatient evaluation of hematochezia. Am.J.Gastroenterol. 1998;93(2):179-82. 45. Mant A, Bokey EL, Chapuis PH, Killingback M, Hughes W, Koorey SG et al. Rectal bleeding. Do other symptoms aid in diagnosis? Dis.Colon Rectum 1989;32(3):191-6. 46. Fijten GH, Starmans R, Muris JW, Schouten HJ, Blijham GH, Knottnerus JA. Predictive value of signs and symptoms for colorectal cancer in patients with rectal bleeding in general practice. Fam.Pract. 1995;12(3):279-86. 47. Guidelines for the Diagnosis and the Management of Colorectal Cancer www.im.dk/publikationer/ventetider2001/ventetider2001.htm (10.December 2004). Web 2002. Ref Type: Internet Communication 69 48. Vella M, O'Dwyer PJ. Prediction of colorectal cancer by consultation questionnaire. Lancet 2002;360(9350):2079-80. 49. Kraeft i tal. 2005. www.sst//fm8-10060.nt.uni2.dk/kraefttal2/p2000S22.htm (22. January 2005) Ref Type: Internet Communication 50. Dukes C. The classification of cancer of the rectum. J Pathol Bacteriol 1932;35:323-32. 51. Kronborg O. Staging and surgery for colorectal cancer. Eur.J.Cancer 1993;29A(4):575-83. 52. Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish Cancer Registry--history, content, quality and use. Dan.Med.Bull. 1997;44(5):535-9. 53. Hermanek P, Hutter R, Sobin L, Wagner G, Witterkind C. TNM Atlas Fourth Edition 1997. Springer-Verlag Berlin Heidelberg New York; 1997. 54. Danish Colorectal Cancer Group. Annual report 2001-2002 for colorectal cancer. 2005.www.kirurgisk-selskab.dk/dccg/indhold.pdf (22. January 2005) Ref Type: Internet Communication 55. Danish Society for Pathological Anatomy and Clinical Cytology. Recommendations of handling specimens with malignant colorectal neoplasm . 1997. Ref Type: Report 56. Compton CC, Greene FL. The staging of colorectal cancer: 2004 and beyond. CA Cancer J.Clin. 2004;54(6):295-308. 57. Bulow S. Familial adenomatous polyposis. Ann.Med. 1989;21(4):299-307. 58. Katballe N, Christensen M, Wikman FP, Orntoft TF, Laurberg S. Frequency of hereditary non-polyposis colorectal cancer in Danish colorectal cancer patients. Gut 2002;50(1):43-51. 59. Mellemkjaer L, Johansen C, Gridley G, Linet MS, Kjaer SK, Olsen JH. Crohn's disease and cancer risk (Denmark). Cancer Causes Control 2000;11(2):145-50. 60. Mellemkjaer L, Olsen JH, Frisch M, Johansen C, Gridley G, McLaughlin JK. Cancer in patients with ulcerative colitis. Int.J.Cancer 1995;60(3):330-3. 61. Wheeler DW. Delay experienced by patients with symptomatic colorectal cancer. Colorectal Diseases 1999;1:174-6. 62. Robertson R, Campbell NC, Smith S, Donnan PT, Sullivan F, Duffy R et al. Factors influencing time from presentation to treatment of colorectal and breast cancer in urban and rural areas. Br.J Cancer 2004;90(8):1479-85. 63. Synnestvedt M, Meen O, Hofstad B. [Colorectal cancer. Location dependent symptoms?]. Tidsskr.Nor Laegeforen. 1997;117(26):3796-9. 64. Dent OF, Goulston KJ, Tennant CC, Langeluddecke P, Mant A, Chapuis PH et al. Rectal bleeding. Patient delay in presentation. Dis.Colon Rectum 1990;33(10):851-7. 70 65. Cheung PS, Wong SK, Boey J, Lai CK. Frank rectal bleeding: a prospective study of causes in patients over the age of 40. Postgrad.Med.J. 1988;64(751):364-8. 66. Norrelund N, Norrelund H. Colorectal cancer and polyps in patients aged 40 years and over who consult a GP with rectal bleeding. Fam.Pract. 1996;13(2):160-5. 67. Barwick TW, Scott SB, Ambrose NS. The two week referral for colorectal cancer: a retrospective analysis. Colorectal Dis. 2004;6(2):85-91. 68. Carlsson L, Hakansson A, Nordenskjold B. Common cancer-related symptoms among GP patients. Opportunistic screening in primary health care. Scand.J.Prim.Health Care 2001;19(3):199-203. 69. Funch DP. Predictors and consequences of symptom reporting behaviors in colorectal cancer patients. Med.Care 1988;26(10):1000-8. 70. Pullyblank AM, Cawthorn SJ, Dixon AR. Knowledge of cancer symptoms among patients attending one-stop breast and rectal bleeding clinics. Eur.J.Surg.Oncol. 2002;28(5):511-5. 71. Thomas RJ, Clarke VA. Community (mis)understanding of colorectal cancer treatment. Aust.N.Z.J.Surg. 1998;68(5):328-30. 72. Hansen HJ, Morsel-Carlsen L, Bulow S. [Patients' perception of symptoms in colorectal cancer. A cause of delay in diagnosis and treatment]. Ugeskr.Laeger 1997;159(13):1941-4. 73. de Nooijer J, Lechner L, de Vries H. Early detection of cancer: knowledge and behavior among Dutch adults. Cancer Detect.Prev. 2002;26(5):362-9. 74. McCaffery K, Wardle J, Waller J. Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev.Med. 2003;36(5):525-35. 75. Kjeldsen BJ, Kronborg O, Fenger C, Jorgensen OD. A prospective randomized study of follow-up after radical surgery for colorectal cancer. Br.J.Surg. 1997;84(5):666-9. 76. Talley NJ, Zinsmeister AR, Van Dyke C, Melton LJ, III. Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroenterology 1991;101(4):927-34. 77. Drossman DA, Sandler RS, McKee DC, Lovitz AJ. Bowel patterns among subjects not seeking health care. Use of a questionnaire to identify a population with bowel dysfunction. Gastroenterology 1982;83(3):529-34. 78. Kay L, Jorgensen T, Schultz-Larsen K. Colon related symptoms in a 70-year-old Danish population. J.Clin.Epidemiol. 1993;46(12):1445-9. 79. Keddie N, Hargreaves A. Symptoms of carcinoma of the colon and rectum. Lancet 1968;2(7571):749-50. 80. Acher PL, Al Mishlab T, Rahman M, Bates T. Iron-deficiency anaemia and delay in the diagnosis of colorectal cancer. Colorectal Dis. 2003;5(2):145-8. 81. Dixon AR, Thornton-Holmes J, Cheetham NM. General practitioners' awareness of colorectal cancer: a 10 year review. BMJ 1990;301(6744):152-3. 71 82. Wobbes T. Carcinoma of the colon and rectum in geriatric patients. Age Ageing 1985;14(6):321-6. 83. MacArthur C, Smith A. Factors associated with speed of diagnosis, referral, and treatment in colorectal cancer. J.Epidemiol.Community Health 1984;38(2):122-6. 84. Olsson L, Loof L, Ekbom A. A population-based audit for diagnosing colorectal cancer. Scand.J Gastroenterol. 2004;39(2):158-63. 85. Ohman U. Prognosis in patients with obstructing colorectal carcinoma. Am.J.Surg. 1982;143(6):742-7. 86. Umpleby HC, Williamson RC. Survival in acute obstructing colorectal carcinoma. Dis.Colon Rectum 1984;27(5):299-304. 87. Waiting List www.im.dk/publikationer/ventetider2001/ventetider2001.htm (10 December 2004). Web 2001. 88. Read-Jones M. General practitioner's awareness of colorectal cancer: has referral improved? Br.J Gen.Pract. 2001;51(468):580. 89. Simunovic M, Gagliardi A, McCready D, Coates A, Levine M, DePetrillo D. A snapshot of waiting times for cancer surgery provided by surgeons affiliated with regional cancer centres in Ontario. CMAJ. 2001;165(4):421-5. 90. Flashman K, O'Leary DP, Senapati A, Thompson MR. The Department of Health's "two week standard" for bowel cancer: is it working? Gut 2004;53(3):387-91. 91. Jass JR SL. WHO's Tumorclassification 1989. Springer-Verlag Berlin Heidelberg New York; 1989. 92. Rothman K. Modern Epidemiology. Library of Congress Catalog Card; 1986. 93. Altman DG, Gardner MJ. Presentation of variability. Lancet 1986;2(8507):639. 94. Sobin L, Witterkind C. TNM Atlas Sixth Edition 2002. Wiley-Liss, New York; 2002. 95. O'Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J.Natl.Cancer Inst. 2004;96(19):1420-5. 96. Whittaker MA, Carr NJ, Midwinter MJ, Badham DP, Higgins B. Acinar morphology in colorectal cancer is associated with survival but is not an independent prognostic variable. Histopathology 2000;36(5):439-42. 97. Sternberg A, Amar M, Alfici R, Groisman G. Conclusions from a study of venous invasion in stage IV colorectal adenocarcinoma. J.Clin.Pathol. 2002;55(1):17-21. 98. Deans GT, Heatley M, Anderson N, Patterson CC, Rowlands BJ, Parks TG et al. Jass' classification revisited. J.Am.Coll.Surg. 1994;179(1):11-7. 99. Komuta K, Batts K, Jessurun J, Snover D, Garcia-Aguilar J, Rothenberger D et al. Interobserver variability in the pathological assessment of malignant colorectal polyps. Br.J.Surg. 2004;91(11):1479-84. 72 100. Cross SS. Grading and scoring in histopathology. Histopathology 1998;33(2):99-106. 101. Goldstein NS. Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years: recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am.J.Surg.Pathol. 2002;26(2):179-89. 102. Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann.Surg.Oncol. 2003;10(1):65-71. 103. Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J.Clin.Oncol. 2003;21(15):2912-9. 104. Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch.Pathol.Lab Med. 2000;124(7):979-94. 105. Mukai M, Ito I, Mukoyama S, Tajima T, Saito Y, Nakasaki H et al. Improvement of 10-year survival by Japanese radical lymph node dissection in patients with Dukes’s B and C colorectal cancer: a 17-year retrospective study. Oncol.Rep. 2003;10(4):927-34. 106. Bouhier K, Maurel J, Lefevre H, Bouin M, Arsene D, Launoy G. Changing practices for diagnosis and treatment of colorectal cancer in Calvados: 1990-1999. Gastroenterol.Clin.Biol. 2004;28(4):371-6. 107. Carter S, Winslet M. Delay in the presentation of colorectal carcinoma: a review of causation. Int.J.Colorectal Dis. 1998;13(1):27-31. 108. Crosland A, Jones R. Rectal bleeding: prevalence and consultation behaviour. BMJ 1995;311(7003):486-8. 109. Macadam DB. A study in general practice of the symptoms and delay patterns in the diagnosis of gastrointestinal cancer. J.R.Coll.Gen.Pract. 1979;29(209):723-9. 110. Debnath D, Dielehner N, Gunning KA. Guidelines, compliance, and effectiveness: a 12 months' audit in an acute district general healthcare trust on the two week rule for suspected colorectal cancer. Postgrad.Med.J 2002;78(926):748-51. 111. Kemppainen M, Raiha I, Rajala T, Sourander L. Delay in diagnosis of colorectal cancer in elderly patients. Age Ageing 1993;22(4):260-4. 112. Bassett ML, Bennett SA, Goulston KJ. Colorectal cancer. A study of 230 patients. Med.J.Aust. 1979;1(13):589-92. 113. Rex DK, Bond JH, Feld AD. Medical-legal risks of incident cancers after clearing colonoscopy. Am.J Gastroenterol. 2001;96(4):952-7. 114. Bressler B, Paszat LF, Vinden C, Li C, He J, Rabeneck L. Colonoscopic miss rates for rightsided colon cancer: a population-based analysis. Gastroenterology 2004;127(2):452-6. 115. Kemppainen M, Raiha I, Rajala T, Sourander L. Characteristics of colorectal cancer in elderly patients. Gerontology 1993;39(4):222-7. 73 REFERENCES 1. Pisani P, Parkin DM, Ferlay J. Estimates of the worldwide mortality from eighteen major cancers in 1985. Implications for prevention and projections of future burden. Int J Cancer 1993;55(6):891-903. 2. Pisani P, Parkin DM, Bray F, Ferlay J. Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer 1999;83(1):18-29. 3. Edwards BK, Howe HL, Ries LA, Thun MJ, Rosenberg HM, Yancik R, et al. Annual report to the nation on the status of cancer, 1973-1999, featuring implications of age and aging on U.S. cancer burden. Cancer 2002;94(10):2766-92. 74