doc1101
advertisement
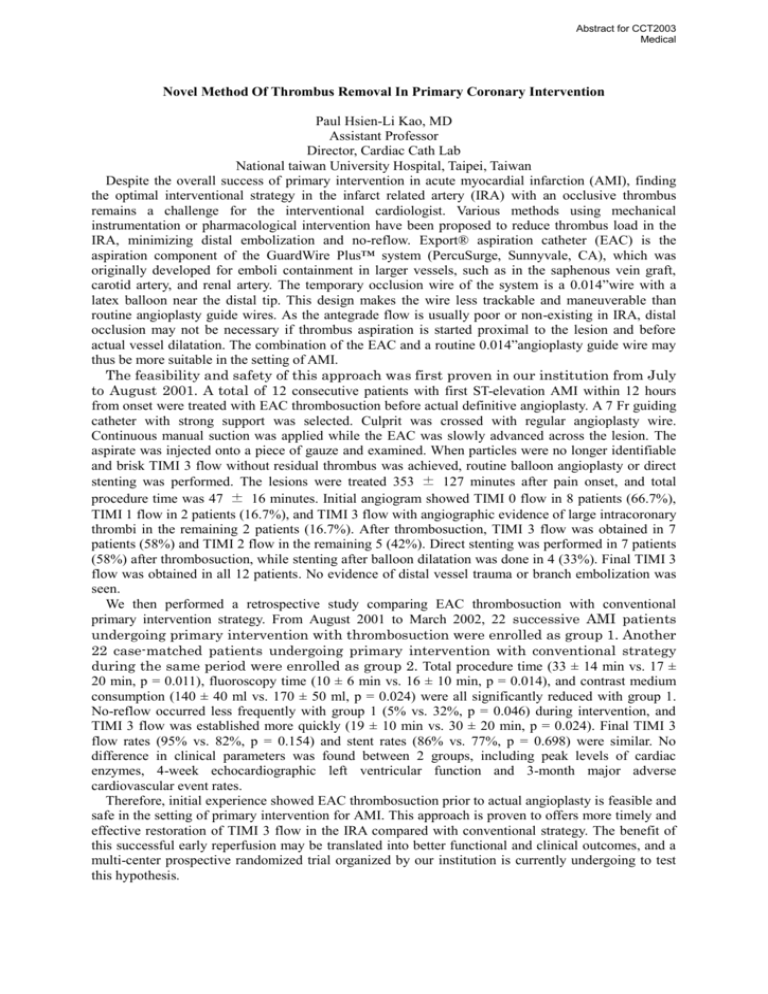
Abstract for CCT2003 Medical Novel Method Of Thrombus Removal In Primary Coronary Intervention Paul Hsien-Li Kao, MD Assistant Professor Director, Cardiac Cath Lab National taiwan University Hospital, Taipei, Taiwan Despite the overall success of primary intervention in acute myocardial infarction (AMI), finding the optimal interventional strategy in the infarct related artery (IRA) with an occlusive thrombus remains a challenge for the interventional cardiologist. Various methods using mechanical instrumentation or pharmacological intervention have been proposed to reduce thrombus load in the IRA, minimizing distal embolization and no-reflow. Export® aspiration catheter (EAC) is the aspiration component of the GuardWire Plus™ system (PercuSurge, Sunnyvale, CA), which was originally developed for emboli containment in larger vessels, such as in the saphenous vein graft, carotid artery, and renal artery. The temporary occlusion wire of the system is a 0.014”wire with a latex balloon near the distal tip. This design makes the wire less trackable and maneuverable than routine angioplasty guide wires. As the antegrade flow is usually poor or non-existing in IRA, distal occlusion may not be necessary if thrombus aspiration is started proximal to the lesion and before actual vessel dilatation. The combination of the EAC and a routine 0.014”angioplasty guide wire may thus be more suitable in the setting of AMI. The feasibility and safety of this approach was first proven in our institution from July to August 2001. A total of 12 consecutive patients with first ST-elevation AMI within 12 hours from onset were treated with EAC thrombosuction before actual definitive angioplasty. A 7 Fr guiding catheter with strong support was selected. Culprit was crossed with regular angioplasty wire. Continuous manual suction was applied while the EAC was slowly advanced across the lesion. The aspirate was injected onto a piece of gauze and examined. When particles were no longer identifiable and brisk TIMI 3 flow without residual thrombus was achieved, routine balloon angioplasty or direct stenting was performed. The lesions were treated 353 ± 127 minutes after pain onset, and total procedure time was 47 ± 16 minutes. Initial angiogram showed TIMI 0 flow in 8 patients (66.7%), TIMI 1 flow in 2 patients (16.7%), and TIMI 3 flow with angiographic evidence of large intracoronary thrombi in the remaining 2 patients (16.7%). After thrombosuction, TIMI 3 flow was obtained in 7 patients (58%) and TIMI 2 flow in the remaining 5 (42%). Direct stenting was performed in 7 patients (58%) after thrombosuction, while stenting after balloon dilatation was done in 4 (33%). Final TIMI 3 flow was obtained in all 12 patients. No evidence of distal vessel trauma or branch embolization was seen. We then performed a retrospective study comparing EAC thrombosuction with conventional primary intervention strategy. From August 2001 to March 2002, 22 successive AMI patients undergoing primary intervention with thrombosuction were enrolled as group 1. Another 22 case-matched patients undergoing primary intervention with conventional strategy during the same period were enrolled as group 2. Total procedure time (33 ± 14 min vs. 17 ± 20 min, p = 0.011), fluoroscopy time (10 ± 6 min vs. 16 ± 10 min, p = 0.014), and contrast medium consumption (140 ± 40 ml vs. 170 ± 50 ml, p = 0.024) were all significantly reduced with group 1. No-reflow occurred less frequently with group 1 (5% vs. 32%, p = 0.046) during intervention, and TIMI 3 flow was established more quickly (19 ± 10 min vs. 30 ± 20 min, p = 0.024). Final TIMI 3 flow rates (95% vs. 82%, p = 0.154) and stent rates (86% vs. 77%, p = 0.698) were similar. No difference in clinical parameters was found between 2 groups, including peak levels of cardiac enzymes, 4-week echocardiographic left ventricular function and 3-month major adverse cardiovascular event rates. Therefore, initial experience showed EAC thrombosuction prior to actual angioplasty is feasible and safe in the setting of primary intervention for AMI. This approach is proven to offers more timely and effective restoration of TIMI 3 flow in the IRA compared with conventional strategy. The benefit of this successful early reperfusion may be translated into better functional and clinical outcomes, and a multi-center prospective randomized trial organized by our institution is currently undergoing to test this hypothesis.