Improving Neonatal Skin Care - Emory University Department of
advertisement

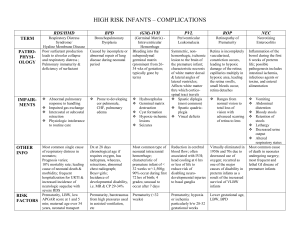
Improving Neonatal Skin Care Gayla Eppinger, NNP-BC Emory University Atlanta GA 2 Improving Neonatal Skin Care Learning Objectives Describe the structure and function of neonatal skin Explain and apply the Neonatal Skin Condition Scale Identify clinical practice goals related to neonatal skin care Describe recommended skin care practices Understand new evidence-based research and recommendations Function of the Skin 1) 2) 3) 4) Serves as barrier against infection and protects internal organs Plays major role in thermoregulation and storage of fat Regulates insensible water loss, also secretes electrolytes & water Provides tactile sensory input and sensations of touch, pressure, temperature, pain & itch a) Difference in Neonatal Skin i) Skin of the premature neonate accounts for 13% of their body weight as compared to 3% of the body weight of an adult ii) Premature neonate has body surface/weight ratio ~ five times greater than that of an adult iii) The skin of a premature neonate is 40-60% thinner than adult skin 1) Epidermis: functions as a barrier, preventing penetration and absorption of potential toxins and microorganisms, as well as retaining heat and water. a) Stratum Corneum: outermost layer of cells forming the epidermis. Non-living layer made up of dead cells constructed like a wall of bricks and mortar b) Forms part of the vernix caseosa, controls transepidermal water loss (TEWL), prevents absorption of toxic substances c) Difference in Neonatal Skin i) 10-20 layers of stratum corneum in full-term infants and adults ii) Neonate <30 weeks gestation has only 2-3 layers and at 23-24 weeks virtually no stratum corneum iii) Maturation rate of stratum corneum varies based on the gestation age: At <27 weeks the process is slowed; At 23-25 weeks it takes 8-10 weeks to develop the function of full term skin; At >27 weeks approaches full-term skin function by ~10 days postnatal age d) Risks of underdeveloped Stratum Corneum i) Infections and skin irritation ii) Increase in insensible water loss iii) Increased evaporative water loss iv) Toxicity from topically applied substances v) Epidermal stripping Anatomy of the Skin Note: Percutaneous absorption of Neomycin (topical antibiotic) has been reported to cause neural deafness. Bacitracin has been noted as one of the 12 most frequent allergens causing a positive patch test reaction in patients ages 892 years. Marks, et al (1995). North American Contact Dermatitis Group standard patch test results. American Journal of Contact Dermatitis, 6, 160-165. 2) The Basal Layer: near the junction of the epidermis and dermis, is the bottom layer of the epidermis. A source of renewal for the epidermis. Living cells which replace cells of the stratum corneum. a) Difference in Neonatal Skin i) Dermal-epidermal junction is connected by fibrils which are fewer and more widely-spaced in premature infants than in full-term infants 3 ii) b) As gestational and postnatal age advances, fibrils become stronger Risks of fewer fibrils i) Diminished cohesion between dermis and epidermis places premature at higher risk for injury ii) Bond between adhesives and epidermis may be stronger than the cohesion between dermis and epidermis, resulting in epidermal stripping when adhesives are removed iii) Premature infant at greater risk of blistering from friction or thermal insults 3) Dermis: under the epidermis. Composed of collagen and elastin fibers. Contains nerves, blood and lymph vessels, mast cells and inflammatory cells. The carrier of heat, pressure and pain. a) Difference in Neonatal Skin i) Premature infants prone to edema due to less collagen and fewer elastin fibers in the dermis ii) Edema places the neonate at increased risk of ischemic injury and pressure necrosis due to reduced blood flow to the epidermis iii) Full-term infant’s dermis is thick and well-organized, but, thinner and higher water content than adult’s 4) Subcutaneous: fatty connective tissue. Heat insulator, shock absorber, and caloric reservoir. Fat deposition occurs primarily in last trimester Characteristics of Neonatal Skin 1) Skin appearance: soft, wrinkled, velvety, covered with vernix caseosa a) Difference in Premature Skin i) More transparent, gelatinous and wrinkle-free ii) Lanugo present in varying degrees iii) Subcutaneous edema may be present 2) Skin pH: alkaline skin surface with mean pH of 6.34. During next four days, skin pH falls to mean of 4.95 creating “acid mantle”. Provides protection against microorganisms, particularly pathogenic bacteria and fungus. a) Difference in Premature Skin i) Skin pH greater than 6.0 at birth ii) Declines to 5.5 over the first weeks, and gradually declines to 5.0 over the first month 3) Nutritional stores: fat and trace mineral zinc accumulates during the third trimester. Necessary to prevent nutritional deficiencies that cause skin disruptions. a) Breast milk or infant formulas contain adequate levels of nutrients b) Premature and sick neonates at risk for fatty acid deficiency c) Infants requiring TPN need adequate replacement of fat and zinc in IV solutions 4) Difference in Neonatal Skin: premature and sick newborns are vulnerable to infection due to a) Immature immune system b) Invasive tubes and catheters c) Frequent use of antibiotics d) Immature skin structure and function e) Excoriations and other sites of skin trauma f) Changes in skin pH 5) What Families Need to Know: Skin of the premature newborn is different than that of the full-term newborn. All neonates admitted to the NICU are at risk for developing skin conditions which may require special skin care. Goals of Neonatal Skin Care 1) 2) 3) 4) Reduce traumatic injury Prevent dryness Avoid exposure to toxins Minimize exposure to unnecessary substances 4 5) Promote normal skin development 1) First Bath: should be given once the newborn’s condition, vital signs and temperature have been stable >2 – 4 hours. a) Recommended Practices i) Wear gloves and implement universal precautions before and during first bath ii) Removing all vernix is not necessary for hygienic reasons iii) Do not use antiseptic soaps or cleanser iv) Use warm water v) Use cotton balls or soft cloth vi) Avoid rubbing skin surfaces to prevent chafing and irritation 2) Routine Bathing: main purpose is to remove debris. A time for contact between newborn and caregiver, which, if not handled properly, can result in physiological and behavioral problems for the newborn. a) Recommended Practices i) Use cleansers with a neutral pH with minimal dyes and perfumes to lessen the impact on the acid mantle, and reduce the risk of future skin sensitization ii) Avoid rubbing skin surface as it can cause chafing and irritation iii) Rinse with water b) Recommended Practices for Infants < 32 Weeks Gestation i) Bathe with warm water and cotton balls or soft cloth during first few weeks of life ii) Use warm sterile water on areas of breakdown 3) Immersion Bathing: placing the infant’s entire body, with the exception of head and face, into a tub of water. a) Recommended Practices i) Use water at a temperature of 100.4 degrees (38 degrees C) to ensure an even temperature and decrease evaporative heat loss ii) After the bath: dry, diaper, and double-wrap (with cap) iii) After 10 minutes: dress, change the cap, and wrap in dry warm blankets 4) What Families Need to Know: gather all supplies and clothing prior to starting the bath; perform bath in draft-free First Bath and Routine Bathing location; avoid using soaps and lotions with perfumes and dyes to prevent sensitizations later in life. Cord Care 1) 2) 3) Studies have shown that disinfectants do not affect bacterial colonization or cord and skin infections Certain antiseptic ointments and isopropyl alcohol have been shown to delay cord separation Recommended Practices a) Clean cord and surrounding skin with skin cleanser used for first or routine bath and rinse thoroughly b) Alternatively, clean cord with sterile water c) Keep cord clean and dry d) Fold diaper below umbilicus e) Clean cord with water if soiled with urine or stool 4) What Families Need to Know: normal cords may seem moist and “mucky” in appearance. Educate them about the normal process of cord healing. Circumcision Care 1) 2) Before the procedure a) Disinfect penis and surrounding skin After the procedure a) Remove disinfectant with water, focus on leg creases, buttocks, and lower back b) Cover penis with petrolatum-impregnated gauze strips or sterile gauze pads over petrolatum for the first 24 hours c) Do not use petrolatum or other lubricants if the circumcision was performed using the PlastiBell technique 5 d) e) 3) Cleanse with water only for 3-4 days to prevent irritation from cleansers No proven benefit to using antimicrobial ointments as compared with petrolatum What Families Need to Know: use petrolatum product and gauze first 24 hours. For the next 3-4 days, clean penis with warm water only. Diaper Dermatitis 1) 2) 3) 4) Causes a) Exposure to stool and fecal enzymes. Prolonged contact with urine-soaked diaper leads to skin becoming moist and macerated and more susceptible to injury b) Skin pH rises – as the skin becomes more alkaline, fecal enzymes and bile salts that cause skin breakdown become activated Identify and treat underlying conditions (malabsorption, diarrhea, intestinal resection, opiate withdrawal) Recommended Practices a) Preventative Strategies: keep skin surface dry i) Change diapers frequently ii) Use super absorbent gel disposable diapers iii) Apply petrolatum to slightly reddened, intact skin b) Treatment After Skin Breakdown: protect skin from more injury i) Generously apply skin barriers containing zinc oxide ii) Apply pectin paste without alcohol followed by a greasy coating with petrolatum or zinc oxide to prevent diaper from sticking to the barrier iii) Remove as much waste material as possible when changing diaper, and re-apply barrier in a thick layer iv) Exposure to air and light is not as effective, re-injury occurs when stool contacts injured skin v) Use anti-fungal ointment or creams to treat candida diaper dermatitis What Families Need to Know: how diaper dermatitis develops and proper preventative and treatment strategies. Avoid products with perfumes and dyes. Emollients 1) Purpose: to protect and restore skin integrity a) When applied twice daily to neonates with birth weights 500-1000 grams, emollient use resulted in reduced visible dermatitis and improved skin integrity b) Have been shown to reduce transepidermal water loss in neonates <32 weeks gestation, but the effect diminishes after 6 hours c) May be safely used on neonates under radiant warmers and phototherapy d) Caution: with twice daily use, higher risk of coagulase-negative Staphylococcus epidermidis sepsis in infants <750grams 2) Recommended Practices a) Use emollients that are petrolatum-based, water miscible, and free of preservatives, dyes and perfumes b) Use on skin that is dry, with scaling, fissures or visible cracking c) Use to protect skin that is prone to breakdown (in groin or thigh) d) Use single patient tubes to prevent cross-contamination 6 Product A&D ointment Aloe Vesta Protective ointment Aquaphor Aquaphor Natural Healing ointment Baby Magic Baby Lotion Balmex Diaper Rash ointment Cholysteramine in Aquaphor Critic-aid Desitin Diaper Rash ointment Dr. Danis Buttocks Cream Dyprotex Elase ointment Eucerin cream Happy Hiney Diaper Rash Products and Emollients: Composition and Cost Manufacturer Ingredients Schering-Plough Cholecalciferol, fish liver oil, petroleum, Memphis, Tenn fragrance, lanolin, mineral oil, paraffin ConvaTec Propylparaben, aloe vera gel, quaternium-15, Princeton, NJ water, hydroxylated lanolin, ozokerite, glycerin, fragrance Beiersdorf, Inc Petrolatum, mineral oil, mineral wax, wool wax Norwalk, Conn alcohol Beiersdorf, Inc Petrolatum, mineral oil, mineral wax, wool wax, Norwalk, Conn alcohol, panthenol, bisabolol, glycerin Mennen Morristown, NJ Block Drug Company Jersey City, NJ Bristol-Myers Squibb Princeton, NJ; Beiersdorf Norwalk, Conn; locally compounded Sween Products N. Mankato, Minn Pfizer New York, NY Compounded at St. John’s Mercy Medical Center, St. Louis, Mo Blistex Oakbrook, Ill Fujisawa Deerfield, Ill Beiersdorf Norwalk, Conn Bristol-Myers, Squibb Princeton, NJ; Beiersdorf Norwalk, Conn compounded at Cost/Oz. 2.12 1.02 .68 .68 Water, glycerin, glyceryl stearate, cetyl alcohol, mineral oil, Peg-100 stearate, lanolin alcohol, fragrance, lanolin, methylparaben, lapyrium chloride, propylparaben, benzalkonium chloride, diazolidinyl urea 11.3% zinc oxide, balsam of Peru, beeswax, benzoic acid, bismuth subnimitrate, mineral oil, purified water, silicone, synthetic white wax 15% cholestyramine liquid (aspartame, citric acid, A&C yellow #10, FD&C red #40, flavor, propylene glycol alginate, colloidal silicon dioxide, sucrose, xanthan gum) in Aquaphor .28 Benzethonium chloride in a soothing, occlusive moisture-resistant paste of proprietary ingredients 40% zinc oxide; BHA, cod liver oil, fragrance, lanolin, methyl paraben, petrolatum, talc, water 32g zinc oxide, 32g starch, 32g talc, 60 ml glycerin, 112 g Aquaphor 2.91 40% micronized zinc oxide, 37.6% petrolatum, 2.5% dimethicone, cod liver oil, aloe 1U fibrinolysin and 666.6 U of deoxyribonuclease in a base of petrolatum and polyethylene Water, mineral oil, isopropyl myristate, Peg-40 sorbitan peroleate, glyceryl lanolate, sorbitol, propylene glycol, cetyl palmitate, magnesium sulfate, aluminum stearate, lanolin alcohol, BHT, methylchloroisothiazolinone, methylisothiazolinone 12 x 4.1 g packets of Questran powder (cholestyramine resin, acacia, citric acid, D&C yellow #10, FD&C yellow #6, flavor, polysorbate 80, propylene glycol, alginate, sucrose) 2.85 1.47 8.40 1.72 13.50 52.72 .84 2.50 7 Carbondale Memorial Hospital compounded in 1 pound of Aquaphor Ilex Paste Calgon-Vestal St. Louis, Mo 5.75 Neosporin Plus Maximum Strength ointment Nystatin cream Burroughs-Wellcome Triangle Park, NC Petrolatum, calcium/sodium PVM/MA copolymer, DMDM hydantoin, iodopropynyl-butycarbamate, mineral oil, peppermint oil, sodium carboxymethyl cellulose Polymyxin B sulfate 10,000U, bacitracin zinc 500U, neomycin 3.5mg, lidocaine 40mg, in a special white petrolatum base 11.78 Nystatin ointment Proshield E. Fougera Melville, NJ Health Pointe Medical Forthworth, Tx 100,000U Nystatin, polysorbate 60, aluminum hydroxide compressed gel, titanium dioxide, glyceryl monostearate, polyethylene glycol monostearate 400, simethicone, sorbic acid, propylene glycol, ethylenediamine, polyoxyethylene fatty alcohol ether, sorbitol solution, methyl paraben, propyl paraben, hydrochloric acid, white petrolatum, purified water 100,000U Nystatin per gram, in a polyethylene and mineral oil base Cleansing foam: purified water, glycerine, cocoamphodiacetate, polaxymer 188, cocamidopropylpeg-dimmiumchloride phosphate, DMSM hydantoin, laureth-23, citric acid, fragrance Lanolin, petrolatum Super Dooper Diaper Doo E. Fougera Melville, NJ 22.50 11.78 6.09 Peacock 5.75 Pharmaceuticals Springfield, Mo Vaseline Cheseborough-Ponds White petrolatum USP .29 Greenwich, Conn Zinc oxide E. Fogera 20% zinc oxide, mineral oil, white wax, white .56 ointment Melville, NY petroleum base Eichenfield, LF, Frieden, IJ, Esterly, NB. 2001. Textbook of Neonatal Dermatology. Philadelphia: WB Saunders. White petroleum is currently regarded as the gold standard. It acts primarily by trapping water in the epidermis. Oils, oil-and-water-based creams and lotion emollients have greater tactile acceptance than greasy ointments. Compared with ointments- oils, creams, and lotions provide a much less-effective moisture barrier. In addition, formulation of a cream or lotion emulsion requires the addition of several potentially irritating, sensitizing, or toxic ingredients. Eucerin Crème contains methylchloroisothiazolinone/methylisothiazolinone (CMI/MI, also known as Kathon CG). CMI/MI has been associated with allergic contact sensitization in up to 10% of exposed adults and is the third most common sensitizer in children with chronic dermatitis. Wood alcohols, along with Kathon CG, thimerosal, nickel, fragrances, and neomycin rank among the most common causes of allergic contact dermatitis in children. 8 Skin Disinfectants 1) Recommended Practices a) Disinfect skin surfaces before invasive procedures b) All disinfectants have the potential to damage tissue; use judiciously c) Use with caution on underdeveloped or damaged skin 2) Disinfectant Products a) Chlorhexidine gluconate (CHG) i) Most effective agent to reduce catheter-related infections in adults ii) Has been shown to reduce colonization with bacteria in NICU patients b) Povidone-iodine 10% aqueous solution (PI) i) More efficacious than alcohol for skin disinfection ii) Can be absorbed through the skin of premature neonates and result in thyroid suppression c) Isopropyl alcohol (70%) i) Use cautiously, it is irritating and drying to skin and may cause chemical burns ii) Do not use for removing CHG or PI Note: After use, always remove disinfectant with sterile water or saline to minimize absorption and prevent tissue damage. Adhesives Adhesive removal is the primary cause of skin breakdown. 1) Recommended Practices a) Applying Adhesive i) Minimize amount of adhesive in contact with skin ii) Use smaller pieces of tape iii) Use “double-backed” tape iv) Deactivate adhesive with cotton balls when full adhesion not required v) Do not use bonding agents (benzoin) to enhance adhesion vi) Avoid bandages after heel sticks. Use pressure with a cotton ball or gauze b) 2) Removing Adhesive i) Loosen adhesive with mineral oil or petrolatum-based emollients ii) Slowly fold adhesive back onto itself while moistening the adhesive-skin surface with water-soaked cotton balls iii) Avoid solvents due to potential and proven toxicity Adhesive Products a) Hydrogel Electrodes and Adhesive Strips i) Cause little or no trauma ii) Recommended for premature and full-term infants iii) Cannot be used to secure catheters, endotracheal tubes or other life support equipment b) Pectin Barriers i) Mold to skin surfaces and adhere well ii) Can be used under tape to prevent epidermal stripping caused by tape removal 9 iii) Absorb moisture iv) Removal can cause skin trauma, so use care when removing v) Hydrocolloid adhesives are similar to pectin barriers c) Stretchy Gauze and Other Wraps i) Use to anchor electrodes, probes, and secure limbs to IV boards ii) Use with caution to prevent constriction of blood flow and decrease tissue perfusion d) Transparent Dressings i) Use to anchor silicone catheters, central venous lines, peripheral IVs, nasal cannulas and nasogastric tubes ii) Semi-permeable film allows the skin to breathe and catheter sites to be visible iii) Can cause epidermal stripping when removed e) Alcohol-Free Skin Protectants i) Coat skin with plastic polymers to create a barrier between skin and adhesives ii) Recommended for infants over 30 days of age iii) Safety in premature and full-term infants has not been evaluated Importance of Skin Assessment: facilitates early identification and treatment of skin problems. Head-to-toe inspection of skin surfaces should be done every 12 hours. a) Use an objective scale b) Evaluate risk factors that may impede skin integrity i) Monitoring probes and electrodes ii) Adhesives to secure tubes and catheters iii) Paralyzing agents and vasopressors iv) Surgical wounds and ostomies v) Technology that limits position and mobility Neonatal Skin Condition Scale Dryness: 1 = normal, no sign of dryness 2 = dry skin, visible scaling 3 = very dry skin, cracking/fissures Erythema: 1 = no evidence of erythema 2 = visible erythema < 50% body surface 3 = visible erythema > 50% body surface Breakdown: 1 = none 2 = small localized areas 3 = extensive Prevention of Skin Breakdown 1) Risk factors for pressure sores a) Treatments or technologies that make turning or moving difficult b) Severe edema, hypotension, peripheral tissue hypoperfusion 10 c) Common sites include occiput of head, ears due to relatively large size and weight of newborn’s head 2) Friction injuries are another source of skin breakdown 3) Recommended Practices for preventing pressure ulcers a) Use cotton surfaces or sheepskin b) Reduce the impact of pressure on a small surface area with the use of water or air mattresses, gel mattresses, and pads c) Protect areas that have skin-on-skin contact with petrolatum ointment d) Use transparent dressings to protect knees and elbows 1) Recommended Practices for Skin Breakdown a) Flush affected areas with warm solution of half saline/half sterile water using 18- or 20- gauge IV catheter and 30cc syringe every 4-6 hours b) Cover superficial wounds and scrapes with petrolatum-based ointment c) Use antibiotic ointment if extensive bacterial colonization with gram positive organisms d) Triple antibiotic ointment is not recommended e) Use transparent dressings, hydrogel and hydrocolloid wound care products on deeper wounds f) Hydrogel dressings can be used in conjunction with antimicrobial or antifungal ointments g) Transparent dressings and hydrocolloids should not be used on infected wound h) No disinfectant solutions directly on wounds 2) Recommended Practices for Fungal Infections a) Asses for early symptoms (erythematous skin surfaces, crusting or erosive lesions) b) Obtain skin culture, gram stain or potassium hydroxide (KOH) prep c) Apply antifungal ointment to skin breakdown & discontinue petrolatum-based ointments d) Observe closely for systemic fungal infection Treatment of Skin Breakdown Transepidermal Water Loss Underdeveloped stratum corneum leads to excessive TEWL and evaporative heat loss. 1) Recommended Practices a) At birth, use occlusive polyethylene bag to cover body torso and extremities b) Place infant in high humidity environment (relative humidity >70%) first seven days c) Cover body surfaces with transparent dressings d) Apply petrolatum-based ointment every 6 hours to body surface e) Maintain relative humidity >40% f) Use double-walled incubators g) Provide supplemental conductive heat using heated mattress to reduce radiant warmer output h) Use polyethylene tents or blankets, that do not touch the skin, to trap moisture Nutrition Zinc is required for wound healing and maintenance of skin integrity; essential fatty acid deficiency (EFAD) can result in scaly dermatitis. 1) Recommended Practices a) Add zinc to parenteral nutrition b) Additional amounts of zinc may be required for infants with high ostomy output, chronic diarrhea, short bowel syndrome or large wounds c) Prevent EFAD with daily intravenous intralipid infusion 11 New Skin Care Research Carolyn Lund, MS, RN, FAAN, Children's Hospital, Oakland, California, a member of the Evidence-Based Clinical Practice Development team, presented a poster on the clinical outcomes of the AWHONN/NANN clinical practice guideline.[4] The clinical practice guideline provided the studied institutions with a foundation for practice that was integrated into care. Statistically significant changes in practice were described after implementation of the skin care guideline: bathing frequency decreased and emollient use increased yet there was no increase in positive blood cultures. Using a standardized assessment score, the Neonatal Skin Condition Score (NSCS), there was a statistically significant improvement in skin condition noted in both well newborns and premature newborns after implementation of the evidence-based neonatal skin care guideline. Dolores Quinn, RN, NNP,[5] UCSF Medical Center, San Francisco, California, presented the results of a randomized controlled trial that compared the impact of bathing every other day vs every fourth day on skin flora type and colony count in premature infants 25 to 33 weeks of gestation. There was no statistical significance between the groups. Skin flora and colony count did not increase with the increased interval between bathing. The limitations of the study include the small sample size. This research supports the skin care practice recommendation related to bathing, which limits bathing frequency to 2-3 times per week and attempts to define a bathing timetable that is safe, as defined by increase in skin colony counts and infection. Guidelines for Clinical Practice Evaluation and implementation of research-based evidence is the foundation of nursing care. Implementation of the AWHONN-NANN Skin Care Guideline improves overall skin condition of newborns and reduces iatrogenic injury. Nurses need to continue to review and evaluate new research and products for implementation in their practice as well as conduct/support new research that describes skin care practices with clinical outcomes. 12 References Agren J, Sjors G, Sedin G. Transepidermal water loss in infants born at 24 and 25 weeks of gestation. Acta Paediatr. 1998;87:1185-1190 Alexander, M. (Ed.). (2000). Infusion Nursing Standards of Practice. Journal of Intravenous Nursing, 23(S1-S88). Association of Women’s Health Obstetric and Neonatal Nursing and the National Association of Neonatal Nurses. EvidenceBased Clinical Practice Guideline: Neonatal Skin Care. Washington, DC: The Association of Women’s Health, Obstetric and Neonatal Nurses; 2001. Bautista, M.I.B., Wickett, R.R., Visscher, M.O., Pickens, W.L., Hoath, S.B. (2000). Characterization of Vernix Caseosa as a Natural Biofilm: Comparison to Standard Oil-Based Ointments. Pediatric Dermatology, 17 (4):253-260. Benis, M.M. (1999). Newborn Percutaneous Absorption: Hazards and Therapeutic Uses. Neonatal Network. 18(8):63-69. Bonham, P. (2000). Topical Therapy Tips: Wound Care with Hydrocolloid Dressings. Advance for Nurses, October 2:29-31. Choudhuri J, McQueen R, Inoue S, Gordon RC. Efficacy of skin sterilization for a venipuncture with the use of commercially available alcohol or iodine pads. Am J Infect Control. 1990;18:82-85. Cisler-Cahill, L. (2006). A Protocol for the Use of Amorphous Hydrogel to Support Wound Healing in Neonatal Patients: An Adjunct to Nursing Skin Care. Neonatal Network, 25(4):267-273. Darmstadt G, Dinulos J. Neonatal skin care. Pediatr Clin North Am. 2000;47:757-782. Dickison, L. Garland L. Nursing management of NCPAP in preterm neonates: evidence based reduction of skin breakdown. Program and abstracts of the National Association of Neonatal Nurses 19th Annual Conference; October 8-11, 2003; Palm Springs, California. Edwards W, Conner J, Gerdes J, et al. The effect of Aquaphor ointment on nosocomial sepsis rates and skin integrity in infants of birthweights 501-1000g. Program and abstracts of Hot Topics Neonatology Conference; December 3-5, 2000; Washington, DC. Eichenfield, L.F., Frieden, I.J., Esterly, N.B. (2001). Textbook of Neonatal Dermatology, W.B. Saunders. Philadelphia: WB Saunders. Garland JS, Buck RK, Maloney P, et al. Comparison of 10% povidone-iodine and 0.5% chlorhexidine gluconate for the prevention of peripheral intravenous catheter colonization in neonates: a prospective trial. Pediatr Infect Dis J. 1995;14:510-516. Haubrich, K.A. (2003). Role of Vernix Caseosa in the Neonate. Potential Application in the Adult Population. AACN Clinical Issues. 14(4):457-464. Hoath S, Narendran V. Adhesives and emollients in the preterm infant. Semin Neonatol. 2000;5:112-119. Jacob, S. E., Steele, T. (2006). Allergic Contact Dermatitis: Early Recognition and Diagnosis of Important Allergens. Dermatology Nursing, 18(5):433-446. Linder N, Davidovitch N, Reichman B, et al. Topical iodine-containing antiseptics and subclinical hypothyroidism in preterm infants. J Pediatr. 1997;131:434-439. Lund, C., Kuller, J., Lane, A., Lott, J.W., Raines, D.A. (1999). Neonatal Skin Care: The Scientific Basis for Practice. JOGNN: Journal of Obstetric, Gynecologic, & Neonatal Nursing. 28(3):241-254. Lund CH. Update on the neonatal skin care guideline: bathing, disinfectants, adhesives, emollients, diaper dermatitis and IV infiltrates. Program and abstracts of the National Association of Neonatal Nurses 19th Annual Conference; October 8-11, 2003; Palm Springs, California. Lund CH, Osborne JW, Kuller J, Lane AT, Lott JW, Raines DA. Neonatal skin care: clinical outcomes of the AWONN/NANN evidence-based clinical practice guideline. Association of Women's Health, Obstetric and Neonatal Nurses and the National Association of Neonatal Nurses. J Obstet Gynecol Neonatal Nurs. 2001;30:41-51. Lund CH, Kuller J, Lane AT, Lott JW, Raines DA, Thomas KK. Neonatal skin care: evaluation of the AWHONN/NANN research based practice project on knowledge and skin care practices. Association of Women's Health, Obstetric and Neonatal Nurses/National Association of Neonatal Nurses. J Obstet Gynecol Neonatal Nurs. 2001;30:30-40. 13 Lund CH, Osborne JW, Kuller J, Lane AT, Lott JW, Raines DA. Neonatal skin care: clinical outcomes of the Association for Women's Health, Obstetric and Neonatal Nurses (AWHONN) and the National Association of Neonatal Nurses (NANN) Clinical Practice Guideline. Program and abstracts of the National Association of Neonatal Nurses 19th Annual Conference; October 8-11, 2003; Palm Springs, California. Poster #103 Lund CH. Special skin care issues for the ELBW infants: TEWL management, emollients and infection, invasive fungal dermatitis and NCPAP. Program and abstracts of the National Association of Neonatal Nurses 19th Annual Conference; October 8-11, 2003; Palm Springs, California. Maki D, Ringer M, Alvarado C. Prospective randomized trial povidone-iodine, alcohol and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet. 1991;338:339-343. Maki, D. G. (1989). Pathogenesis, Prevention, and Management of Infections Due to Intravascular Devices Used for Infusion Therapy. In A. L. Bisno & F. A. Waldvogel (Eds.). Infections Associated with Indwelling Medical Devices (pp. 161177). Washington, DC: American Society for Microbiology. Marks, et al (1995). North American Contact Dermatitis Group standard patch test results. American Journal of Contact Dermatitis, 6, 160-165. Mendenhall, A.K., Eichenfield, L.F. (2000). Back to Basics: Caring for the Newborn’s Skin. Contemporary Pediatrics. 17(8):99114. Quinn, D., Newton, N., Piecuch, R. (2005). Effect of Less Frequent Bathing on Premature Skin. JOGNN Clinical Research, 34(6):741-746. Rowan JL, Atkins JT, Levy ML, Baer SC, Baker C. Invasive fungal dermatitis in the < or = 1000 gram neonate. Pediatrics. 1995;95:682-687. Visscher, M.O., Narendran, V., Pickens, W.L., LaRuffa, A.A., Meinzen-Derr, J., Allen, K., Hoath, S.B. (2005). Vernix Caseosa in Neonatal Adaptation. Journal of Perinatology, 25:440-446. Yoshio, H., Tollin, M., Gudmundsson, G.H., Lagercrantz, H., Jornvall, H., Marchini, G., Agerberth, B. (2003). Antimicrobial Polypeptides of Human Vernix Caseosa and Amniotic Fluid: Implications for Newborn Innate Defense. Pediatric Research, 53(2): 211-216.