Dr. Godfrey Biemba - Zambia UK Health Workforce Alliance
advertisement
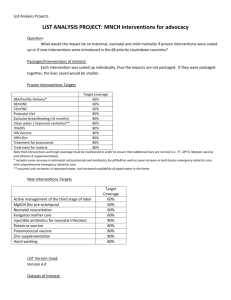
Maternal and Newborn Health Conference for Zambia’s Mothers and Babies Two Neonatal Survival Intervention Studies: Zambia Chlorhexidine Application Trial (ZamCAT) and Lufwanyama Neonatal Survival Project (LUNESP) Dr. Godfrey Biemba, MBChB, M.Sc Research Assistant Professor, Boston University Country Director, ZCAHRD What is ZCAHRD? • A registered non-governmental Applied and Implementation Research Organization • Comprise • Faculty and staff of the Center for Global Health and Development (CGHD) at Boston University (USA) • Zambian public health professionals and specialists • Project offices in Lusaka, Mazabuka, Choma, Kalomo, Livingstone. • Central Office in Lusaka Zambia Chlorhexidine Application Trial (ZamCAT) • Cluster-randomized controlled effectiveness trial comparing: • Daily cord cleansing with 4% chlorhexidine to • Dry cord care (MoH guided standard practice) • Primary outcome = neonatal mortality • Target sample size = 42,500 mother/baby pairs • Recruit pregnant women from 24 weeks gestation during ANC at facility or during outreach • Total of 9 visits are made per participant post enrollment/consenting (4=prenatal & 5=postnatal). • Six Districts of Southern Province (Choma, Monze, Mazabuka, Kalomo, Livingstone & Siavonga) with a total of 90 clusters 3 Zambia Chlorhexidine Application Trial (ZamCAT) • Part of an Alliance for Maternal and Newborn Health Improvement (AMANHI) • Multi-country study that aims to generate unique information to guide improvements on interventions to reduce maternal and newborn mortality and morbidity, and to prevent stillbirths • Progress: • >35,000 pregnant women enrolled; 28,000 deliveries; >25,000 completed study • Under AMANHI, 270 female data collectors have been trained to (as part of maternal morbidity screening): • Determine EDD using pregnancy wheels • Measure urine protein using urine dipsticks • Measure BP using portable microlife BP machines. 4 Lufwanyama Neonatal Survival Project In communities with limited access to health care, is it possible to reduce neonatal mortality by training TBAs in skills that address some of the most important causes of neonatal mortality, notably birth asphyxia, neonatal hypothermia, and neonatal sepsis? Cluster randomized, controlled effectiveness trial Cluster= ‘All infants delivered by a given TBA’ Intervention: TBAs trained in NRP and antibiotics/facilitated referral (AFR) at baseline with refresher training every 3-4months Control: TBAs providing existing standard of care Primary endpoint: Mortality at 28 days of life among live-born infants Additional endpoints: Stillbirth rates, mortality rates at different times during 28 days Cause of death analysis based on verbal autopsies • Reviewed by 3 neonatologists, blinded to allocation group 5 COMPONENTS OF THE INTERVENTION Neonatal resuscitation Program (NRP) Antibiotics with facilitated referral (AFR) Skills Skills Prevention of hypothermia Identification of trigger conditions Clear airway Single dose oral amoxicillin Position airway Accompany mother/infant pair to nearest health facility Proper stimulation when needed Rescue breathing when needed Equipment Two flannel blankets/delivery Rubber bulb syringe/delivery Laerdal mask Laminated reference card (front) Equipment, drugs and supplies Two 250 mg amoxicillin capsules Mixing cup/spoon Oral syringe Bottle with chlorinated water Laminated reference card (back) 6 RESULTS: Primary Endpoint Cumulative All-Cause Mortality By Day 28 7 LUNESP RESULTS : Timing of Deaths During First Month Death Rate on Day of Delivery: 19.9/1000 births (control) vs. 7.8/1000 births (intervention) RR = 0.4, 95% CI 0.19-0.83 8 LUNESP CONCLUSIONS Intervention was highly effective at reducing neonatal mortality • 45% reduction in all-cause mortality by day 28 (Primary Endpoint) • Decreased neonatal mortality rate by 18 per 1000 live births • Note: Zambia national average: 34 deaths per 1000 live births • 1 death averted per 56 deliveries attended by an intervention TBA Largest impact in earliest days of life • Day of birth: 60% reduction • Week one: 44% reduction • Weeks 2-4: non-significant trend NRP appeared to be the most effective component of interventions • Birth asphyxia deaths reduced by 70-80% • No difference in sepsis deaths • No difference in other causes of death 9 Acknowledgements • Arthur Mazimba, David Hamer, Katherine Semrau and the rest of ZamCAT team • Chris Gill, David Hamer, Kojo Yeboah-Anwti and the rest of LUNESP team • Donors: BMGF, USAID ZIKOMO! TWALUMBA! LUITUMEZI! TWATASHA! 10