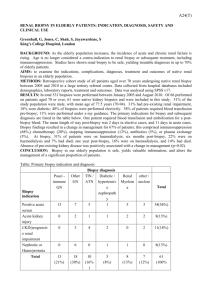
Renal biopsy complications 2004-2005: A regional retrospective

Renal biopsy complications 2005-2006: A regional retrospective review and proposals for future trainee records
Chris Mulgrew,C, 1 Mukherjee,E, 2, Elias,R, 3, Armstrong,K, 1, Chitalia,N, 4, Quan,G, 5
1 Guy’s Hospital, 2 King’s College Hospital, 3 St George’s Hospital, 4 Mayday Hospital
5 St Helier Hospital,
Percutaneous renal biopsies of both native and transplanted kidneys are generally performed by specialist registrars training in renal medicine. Complication rates quoted to patients prior to procedures have tended to be based on either published single operator figures or data from single centres. Records of complications often differ markedly between trainees and between centres in both criteria and accuracy. A standardised method of record keeping across the region would aid prospective data collection, in addition to allowing accurate local complication rates to be given to patients.
A retrospective review of all renal biopsies performed by renal trainees in all South
London renal units between 1 st
April 2005 and 31 st
March 2006 was undertaken. Renal biopsies performed at five centres - St Helier, Guy’s, St George’s, King’s College and
Mayday hospitals - were identified by examining histopathology records. Biopsies performed by radiologists or at other referring hospitals were excluded. To identify patients suffering major complications, haematology records of all patients were examined and notes of those having blood cross-matched between 1 week before and 2 weeks after the biopsy date were studied. Those requiring transfusion following bleeding due to the biopsy, those requiring radiological/surgical intervention and any patients who died as a direct result of the biopsy were then identified. Radiology records were crossreferenced to identify those undergoing interventional procedures after renal biopsy.
With data from one centre pending and to be added shortly, 468 native and 204 transplant renal biopsies were performed during the period studied. Bleeding from the kidney requiring a blood transfusion alone occurred in 20/468 (4.3%) of native and 4/204 (2.0%) of transplant biopsies. The number of patients requiring transfusion and radiological intervention was 7/468 (1.5%) and 0/204 (0%) respectively, while 1/468 (0.2%) native and 1/204 (0.5%) transplant biopsy cases needed surgical intervention and transfusion.
1/468 (0.2%) patient died following a native biopsy during the study period, thought to be as a direct result of the procedure. No deaths were reported following transplant biopsies.
This review is the first to report complication rates of renal biopsies performed across a training region by a cohort of rotating trainees. Clearly there are limitations to this data – for example, the retrospective nature cannot account for variations in indications for transfusion, while co-morbidities will affect the relative risk of procedures – but it gives a snapshot of activity and complications that should be communicated to patients.
Interventional procedures such as renal biopsy carry risks to the patient that are similar to many operations carried out by surgical trainees. Unlike surgical trainees however there is no formal requirement for renal trainees to maintain logbooks of all their procedures and complications. We believe that the collection of biopsy complication data should be prospective and ideally unified in all centres across the region. A trial of prospective data collection and entry on to a Proton database commenced at St Helier Hospital in late
2006. It is proposed that this is extended across the region. Unified criteria for data collection will assist in both accurate quotation of complication risks to the patient and enable trainees to keep accurate personal training records.