Intubation injury
advertisement

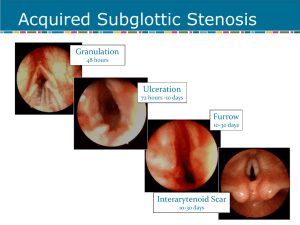
Intubation injury 2004-3-24 R3 杜權恩 Introduction ◇ Laryngeal mucosa, underlying soft tissue, perichondrium or cartilage ◇ Most are superficial or minor ulceration and heal quickly when the tube is removed ◇ 1880, Macewan: clinical observations on the introduction of tracheal tubes by the mouth instead of performing tracheostomy or laryngotomy ◇ 1887, O`Dwyer: short metal tubes introduced into the larynx to overcome the airway obstruction in croup or diphtheria ◇ 1900: Endotracheal tube become routinely in anesthesia ◇ 1950: prolonged intubation was applied ◇ Lin CD, Chen YK, Chang JS: “ Intubation laryngotracheitis” instead of “ intubation injury” ◇ Most resolve without sequel ◇ Intubation injuries are more severe in infants and children than adults - children are more likely to have congenital anatomic abnormalities - variation in body size improper tube selection and intubation ◇ Flexibale bronchoscopy enables the detection of anomalies above and below the glottis and even to the segmental bronchus, also the dynamic status of airway ◇ Injury ◇ The most important consideration: mucosal capillary perfusion ◇ Ischemia irritation congestion, edema ulceration perichondritis, chondritis necrosis of the CA joints and the cricoid cartilage ◇ Laryngeal bedsore ◇ 2 major hypothesis: movement of the tube with mucosa abrasion and the pressure necrosis ◇ The endotracheal tube exert pressure on the posterior larynx, 3 major sites: (1) Medial surface of the arytenoids cartilages, CA joints, and vocal processes (2) Posterior glottis ( vocal process and posterior commissure ) and interarytenoid region (3) Subglottis involving the inner surface of the cricoid cartilage (children) ◇ Subglottis: more vulnerable in infants and small children (the cricoid ring is relatively small compared to the glottis in children) ◇ Factors in intubation trauma 1 (1) Abnormal larynx (2) Trauma sustained during intubation: unskilled, repeat intubation, ventilator movement, suction (3) Impairment of the mucociliary clearing mechanism (4) Gastroesophageal reflux: NG tube (5) Pre-intubation laryngeal appearance: tobacco high risk for granulation and mucociliary dysfunction (6) Bacterial infection (7) Acute or chronic diseased status: altered consciousness, poor tissue perfusion, hypoxia, heart failure, renal failure, DM (8) Duration of intubation: - Adult: 5~7 days Children: 7~14 days Infants: almost no limit time of intubation ( 50 days) (9) Physical characteristics of the tubes: size and shape - Upper limit of ID: male 8.0mm, female 7.0mm - Infants and children < 8 y/o uncuffed tube with a diameter that allow an air leak in the subglottic space with 20 cm-H2O - Plastic tubes of siliconized rubber: smooth-walled and less irritating, softness lead to compressible - High volume, low-pressure cuff Endoscopic assessment (Benjamin) ◇ Laryngeal damage begins during the first few hours and continues with each further day of intubation ◇ During intubation - Indication: adults 5~7 days, children 1~2 weeks, infants only when attempted extubation has been unsuccessful - Resolve without treatment: edema in the vocal fold, edematous protrusion of the ventricles, surface mucosal ulceration, generalized erythema, minor granulation, absence of deep ulceration indicating - - perichondritis Severe and consider tracheostomy: deep ulceration through the perichondrium into the cartilage, widespread concentric ulceration in the subglottis area Attempt extubation, continue intubation VS tracheostomy ◇ After extubation - Most symptoms appear within 24 hr after extubation 2 - Large “tongues” of granulation tissue (immediately) - Reactive glottic or subglottic edema: obstruction in the first minutes or hours Persistent edema and granulation tissue: husky voice in the first few days An intubation granuloma: husky voice many weeks later Posterior glottic stenosis or subglottic stenosis: obstruction weeks or months later Decreased mobility or fixation of the CA joints - Post-extubation stridor ◇ Specific obstructive diseases vocal paralysis, ….. ◇ Untoward sequel of intubation laryngotracheitis subglottic stenosis, ….. ◇ Other “non-organic” obstructive disease neuromuscular disorders General description of intubation changes ◇ Early nonspecific changes - Hyperemia and edema with inflammatory swelling ◇ Edema - Resolve after extubation V.S. chronic Reinke`s edema - Protrusion of edematous mucosa of the ventricle ◇ Ulceration Figure 1 - Superficial (mucosa) heals after tube removal Deep delayed healing and possible scar formation Ulcerated trough: weeks or months after extubation chronic dysfunction or fixation of the CA joints 3 ◇ Granulation tissue Figure 2 - Attempted healing and form at the site of irritation and ulceration Tongues of granulation tissue begin to arise within 48 hrs from the vocal processes, …. Severe obstruction V.S. complete resolution after tube removal (most) Rounded intubation granuloma, healed fibrous nodule, interarytenoid adhesion Commonly occur in the posterior glottis and the subglottic area posterior glottic stenosis ◇ Miscellaneous injuries - Dislocation of an arytenoid - Laceration or bleeding of a vocal cord - Damage to intrinsic muscles - Perforation of the airway - Infection of the soft tissue Grading of laryngeal stenosis ( Zalzal and Cotton ) ◇ Grade I: less than 70% ◇ Grade II: 70~90% ◇ Grade III: more than 90%, identifiable lumen is present ◇ Grade IV: complete obstruction, no lumen present 4 Specific intubation injuries ◇ Ulcerated trough - obvious wide, deep areas of acute ulceration eroding into the cartilage near the CA joint ◇ Healed furrow - develop from incompletely healed ulcerated troughs, and are usually bilateral - seen in the chronic phase as a scarred linear furrow on the medial aspect of the arytenoid and CA joint ◇ Healed fibrous nodule - a small, round, persistent areas of scar tissue on the edge of the vocal cord near the vocal process ◇ Intubation granuloma - a yellow-red pedunculated mass arising from the vocal process and - nearby medial surface of the arytenoid dysphonia, lumping throat ◇ Interarytenoid adhesion - Granulation tissue or ulcerated surfaces fall together and heal across the midline ◇ Posterior glottic stenosis ◇ Subglottic stenosis - the subglottic diameter become sufficient narrow to cause symptoms of airway obstruction - adult: most are due to prolonged intubation - Pediatric: hard caused by a congenital abnormality, soft caused by granulation tissue, submucosal fibrosis, ….. ◇ Ductal retention cyst - Submucosal, large or small, develop in the subglottic region, usually posterior, in infants undergo prolonged intubation - Due to irritation and obstruction of the duct of a mucus-producing gland - 1896 Mitchell et al.: 25% of pediatric laryngeal cysts in the subglottis, exclusively with a history of prolonged intubation mostly multiple, posterolateral subglottis, sometimes accompanied by similar cysts in the upper trachea Ulceration, squamous metaplasia, and subepithelial fibrosis appear after as few as 6 days of intubation ◇ Vocal cord paralysis - spontaneous recovery can be expected within 6 months 5 ◇ Dislocation of arytenoids - Follow blind intubation or use of and introducer - Most commonly on the left side - Persistent hoarseness and pain on swallowing - Manipulation is unlikely to be successful Principles of treatment ◇ Endoscopic evaluation of intubation trauma is necessary for final assessment of the site, nature, and degree of the injury ◇ Acute injuries during intubation - Edema, surface mucosal ulceration, generalized inflammation, early - granulation tissue at the vocal process or the in the posterior larynx observation Deep ulceration into the arytenoids cartilage, cricoid cartilage, CA joint, - all of the posterior glottic space extubation or tracheostomy, antibiotics Dislocation of the arytenoids cartilage attempt to reposition it Removal of granulation tissue ? bleeding, traumatic surface adherence ◇ Chronic injuries after extubation - Interarytenoid adhesion gently break down or divide, further examination in 7~10 days - - Posterior glottic stenosis (scar) divided in the midnight from the subglottic region to the interarytenoid region with laser or scalpel blade, repeated division every 6 months sometimes Subglottic stenosis ◎ anterior cricoid split with/out immediate cartilage graft [1st and 2nd tracheal arch, lower 3rd of the thyroid cartilage] in infants ◎ Laser treatment for scar tissue < 1cm in vertical dimension in adults ◎ involve the glottis reconstructive laryngoplasty (50%) or permanent tracheostomy - ◎ Dilation or unwarranted repeated laser surgery more fibrosis Ductal retention cysts: - ◎ no treatment if small and insignificant ◎ laser for multiple larger cysts cause airway obstruction Fixed or dislocated arytenoids arytenoidectomy ◇ Reintubation: for edema, superficial lesions, or ulceration in preterm 6 Prevention ◇ ◇ ◇ ◇ ◇ Avoid risk factors Choose endotracheal tube : size and material Treat GE reflux Reduce static secretion around the tube Control infection Reference 1.Benjamin B. Prolonged intubation injuries of the larynx: endoscopic diagnosis, classification, and treatment. Ann Otol Rhinol Laryngol 1993;102:1-15 2. Gould S, Young M. Subglottic ulceration and healing following endotracheal intubation in the neonate: a morphometric study. Ann Otol Rhinol Laryngol 1992;101:815-20 3. Bauman N, Benjamin B. Subglottic ductal cysts in the pre-term infant: association with laryngeal intubation trauma. Ann Otol Rhinol Laryngol 1995;104:963-8 4. Weymuller E. Laryngeal injury from prolonged endotracheal intubation. Laryngoscope 1988;98:1-15 (supp 45) 5. Zalzal G, Cotton R. Glottic and subglottic stenosis. In: Cummings C, Fredrickson J, Harker L, Krouse C, Schuller D, eds, Otolaryngology-Head and neck surgery, vol 3, 2nd edn: 1981-2000 6. Contencin P, Narcy P. Size of endotracheal tube and neonatal acquired subglottic stenosis. Arch Otolaryngol Head Neck Surg 1993;119:815-9 7. Montgomery W. Posterior and complete laryngeal stenosis. Arch Otolaryngol 1973;98:170-5 8. Lin CD, Cheng YK, Chang JS, Lin HJ, et al. Endoscopic survey of post-extubation stridor in children. Acta Paediatr Tw 2002;43:91-5 9. Yu HR, Niu CK, Su YT, Huang CB. Flexible bronchoscopic diagnosis of airway injurues after intubation in children. J Formos Med Assoc 2000;99:618-22 10. Bishop MJ. Mechanism of laryngotracheal injury following prolonged tracheal intubation. Chest 1989;96:185-6 11. Wigger HJ, Tang P. Fatal laryngeal obstruction by iatrogenic subglottic cyst. J Pediatr 1968;72: 815-20 12. Ellis SF, Pollak AC, Hanson DG, Jiang JJ. Videolaryngoscopic evaluation of laryngeal intubation injury: incidence and predictive factors. Otolaryngol Head Neck Surg 2001;124:625-33 13. Volpi D, lin PT, Kuriloff DB, Kimmelman CP. Risk factors for intubation of the larynx. Ann Otol Rhinol Laryngol 1987;96:684-86 14. Hoeve LJ, eskici O, Verwoerd CDA. Therapeutic reintubation for post-intubation 7 laryngotracheal injury in preterm infants. Int J Pediatr Otorhinolaryngol 1995;31:7-13 8