Anticholinergic (Parasympatholytic) Bronchodilators
advertisement
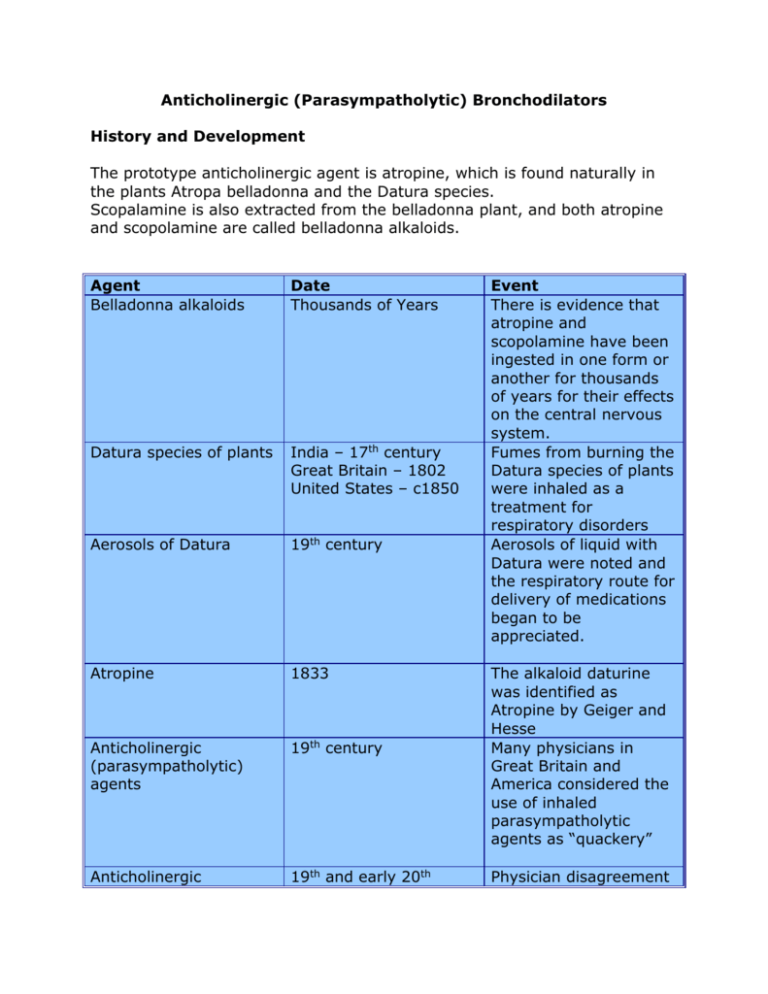
Anticholinergic (Parasympatholytic) Bronchodilators History and Development The prototype anticholinergic agent is atropine, which is found naturally in the plants Atropa belladonna and the Datura species. Scopalamine is also extracted from the belladonna plant, and both atropine and scopolamine are called belladonna alkaloids. Agent Belladonna alkaloids Date Thousands of Years Datura species of plants India – 17th century Great Britain – 1802 United States – c1850 Aerosols of Datura 19th century Atropine 1833 Anticholinergic (parasympatholytic) agents 19th century Anticholinergic 19th and early 20th Event There is evidence that atropine and scopolamine have been ingested in one form or another for thousands of years for their effects on the central nervous system. Fumes from burning the Datura species of plants were inhaled as a treatment for respiratory disorders Aerosols of liquid with Datura were noted and the respiratory route for delivery of medications began to be appreciated. The alkaloid daturine was identified as Atropine by Geiger and Hesse Many physicians in Great Britain and America considered the use of inhaled parasympatholytic agents as “quackery” Physician disagreement (parasympatholytic) agents century on the use of Datura probably rested on several issues: (1) Difficulty in accurate dosage with smoking or aerosol therapy (2) The irritant effects of smoke (3) Confusion over diagnosing and clinically differentiating obstructive and occupational lung diseases led to inappropriate use of Datura alkaloids Adrenaline and ephedrine 1930s By the 1930s, adrenaline and ephedrine had largely replaced stramonium and belladonna extracts for treatment of asthma. Anticholinergic (parasympatholytic) agents 1980s Interest in the anticholinergic agents was renewed, based on two factors: (1) A new understanding of the role of the parasympathetic system in airway obstruction (2) The introduction of atropine derivatives with fewer side effects Ipratropium bromide 1987 Ipratropium bromide was released in the US as the aerosol Atrovent. Clinical Indication for Use I. Indication for Anticholinergic Bronchodilator a. Ipratropium or other anticholinergic agents are indicated as a bronchodilator for maintenance treatment in COPD, including chronic bronchitis and emphysema II. Indications for Combined Anticholinergic and β-Agonist Bronchodilators a. A combination anticholinergic and β-agonist, such as ipratropium and albuterol (Combivent), is indicated for use in patients with COPD on regular treatment who require additional bronchodilation for relief of airflow obstruction b. Ipratropium is also commonly used in severe asthma in addition to β-agonists, especially in acute bronchoconstriction that does not respond well to β-agonist therapy III. Anticholinergic Nasal Spray a. A nasal spray formulation is indicated for symptomatic relief of allergic and non-allergic perennial rhinitis and the common cold Specific Anticholinergic (Parasympatholytic) Agents Drug Ipratropium bromide Brand Name Atrovent Ipratropium bromide and albuterol Combivent Ipratropium bromide and albuterol Oxitropium bromide* DuoNeb Tiotropium bromide Spiriva Oxivent Adult Dosage MDI: 18 mcg/puff 2 puffs qid SVN: 0.02% sol. 500 mcg tid, qid MDI: ipratropium 18 mcg/puff and albuterol 90 mcg/puff 2 puffs qid SVN: ipratropium 0.5 mg and albuterol 3.0 mg Unit dose qid MDI: 100 mcg/puff 2 puffs bid, tid DPI: 18 mcg/inhalation 1 inhalation daily *Available outside the United States Clinical Pharmacology I. Tertiary Ammonium Compounds a. Agents i. Atropine sulfate Time Course Onset: 15 min. Peak: 1-2 hr Duration: 4-6 hr Onset: 15 min. Peak: 1-2 hr Duration: 4-6 hr Onset: 15 min. Peak: 1-2 hr Duration: 4-6 hr Onset: 15 min. Peak: 1-2 hr Duration: 8 hr Onset: 30 min. Peak: 3 hr Duration: 24 hr II. ii. Scopolamine b. Clinical Pharmacodynamics i. Easily absorbed into the bloodstream 1. cause systemic effects ii. Cross the blood-brain barrier 1. cause CNS effects Quaternary Ammonium Compounds a. Agents i. Ipratropium bromide ii. Oxitropium bromide iii. Tiotropium bromide b. Clinical Pharmacodynamics i. Poorly absorbed into the bloodstream 1. no/minimal systemic effects ii. Does not cross the blood-brain barrier 1. no CNS effects Pharmacologic Effects of Anticholinergic (Antimuscarinic) Agents Table 7-2 Comparison of cholinergic antagonism to cholinergic effects Cholinergic Effect Decreased heart rate Miosis (contraction of iris, eye) Salivation Lacrimation Urination Defecation Secretion of mucus Bronchoconstriction Anticholinergic Effect Increased heart rate Mitosis (pupil dilatation) Drying of the upper airway Inhibition of tear formation Urinary retention Antidiarrheal or constipation Mucociliary slowing Inhibition of constriction Table 7-3 Pharmacologic Effects of Tertiary versus Quaternary Anticholinergic Agents Given by Inhalation Organ System Respiratory Tract Tertiary Bronchodilation Decreased mucociliary clearance Blocks hypersecretion Central Nervous System Altered CNS function Quaternary Bronchodilation Little or no change in mucociliary clearance Blocks nasal hypersecretion No effect Eye Cardiac Gastrointestinal Genitourinary Mydriasis Cycloplegia Increased intraocular pressure Minor slowing of heart rate (smaller doses) Increased heart rate (larger doses) Dry mouth, dysphagia, dysphonia Urinary retention Usually no effect* No effect Dry mouth Usually no effect** *Assumes aerosol is not sprayed into eye; use with caution in glaucoma **Use with caution in prostatic enlargement or urinary retention Mode of Action I. II. Anticholinergic Agents a. Cholinergic stimulation of muscarinic receptors on airway smooth muscle and submucosal glands cause bronchoconstriction and increased mucus production b. Anticholinergic agents block the action of acetylcholine at parasympathetic postganglionic effector cell receptors c. Anticholinergic agents act as antagonists at parasympathetic receptor sites and block cholinergic-induced bronchoconstriction d. The effect seen will depend on the degree of tone present that can be blocked i. Individuals with normal lungs will have minimal airway dilation – only a resting level of tone to be blocked ii. Individuals with COPD may have significant airway dilation due to a higher degree of parasympathetic activity (beyond normal resting level) due to vagally-mediated reflex bronchoconstriction Vagally Mediated Reflex Bronchoconstriction a. A portion of the bronchoconstriction seen in COPD may be due to a mechanism of vagally mediated reflex innervation of airway smooth muscle b. Sensory C-fiber nerves respond to a variety of stimuli, such as irritant aerosols, cold air, cigarette smoke, noxious fumes, and mediators of inflammation such as histamine c. When C-fiber nerves are activated, they produce an afferent nerve impulse to the CNS, which results in a reflex cholinergic efferent impulse i. Constriction of airway smooth muscle ii. Mucous gland secretion III. iii. Cough Muscarinic Receptor Subtypes a. Anticholinergic agents are nonselective muscarinic receptor antagonists Receptor M1 Location Postganglionic neuron M2 M3 Postganglionic neuron Airway smooth muscle Submucosal glands Effect Facilitate cholinergic nerve transmission causing the release of ACH Inhibits further ACH release Causes contraction of smooth muscle Increased secretion Adverse Effects Side Effects Seen with Anticholinergic Aerosol (Ipratropium) MDI and SVN (common) MDI (occasional) SVN Dry mouth Cough Nervousness Irritation Dizziness Headache Palpitation Rash Pharyngitis Dyspnea Flu-like symptoms Bronchitis Upper respiratory infections Nausea Occasional bronchoconstriction Eye pain Urinary retention (<3%) Side effects were reported in a small percentage (<1% to 5%) Precautions: Use with caution in patients with narrow-angle glaucoma, prostatic hypertrophy, bladder neck obstruction, constipation, bowel obstruction, or tachycardia The eye must be protected from drug exposure: MDI – holding chamber SVN – mouthpiece and reservoir tube to expiratory side Clinical Application Comparison of Effects for Anticholinergic and β adrenergic Bronchodilators Parameter Onset Time to peak effect Duration Tremor Fall in PaO2 Tolerance Site of action I. II. III. IV. Anticholinergic Slightly slower Slower Longer None None None Larger, central airways β Agonist Faster Faster Shorter Yes Yes Yes Central and peripheral airways Use in Chronic Obstructive Pulmonary Disease a. Anticholinergic agents were found to be more potent bronchodilators than β-adrenergic agents in bronchitis-emphysema Use in Asthma a. Anticholinergic agents not proven superior to β-adrenergic agents b. They offer an additional avenue of management c. They are especially useful for i. Nocturnal asthma ii. Psychogenic asthma (vagally mediated) iii. Patients on beta blockers (angina, HTN, glaucoma) iv. Patients with notable side effects from theophylline v. Acute, severe episodes of asthma not responding well to βadrenergic agents Combination Therapy: β-adrenergic and Anticholinergic Agents in COPD a. Theoretically useful i. Complementary sites of action ii. Mechanism of action separate and complimentary iii. Pharmacokinetics somewhat complementary (onset, peak, duration) iv. Possible additive effects – results conflicting v. Combivent Study: 462 patients at 24 centers Agent Mean increase in FEV1 Combivent 31-33% Atrovent 24-25% Albuterol 24-27% Sequence of Administration a. Frequently debated i. Anticholinergic bronchodilator acts in the central, larger airways 1. some argue it should be given before the β-adrenergic ii. β-adrenergic often given first 1. have more rapid onset and beta-2 receptors are distributed in the large and small airways b. Combivent® and DuoNeb® make it a moot point