Dementia and Pharmacy Intervention
advertisement
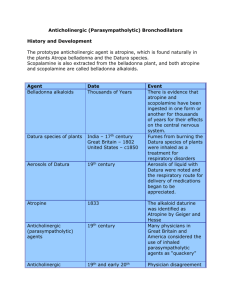
Dementia and Pharmacy Intervention Melissa R. Lewis, Pharm.D. September 17, 2010 Objectives • Define dementia and understand the requirements for diagnosis • Recognize the neuropathology and neurotransmitters involved in dementia • Discuss the pharmacokinetics and pharmacodynamics in the geriatric population • Be able to assess a patient with or suspected to have dementia and make recommendations to optimize therapy A Brief History • First coined by a French physician in 1801 Dr. Philippe Pinel • Alzheimer’s disease first described in 1906 Dr. Alois Alzheimer Types of Dementia • • • • • • Mild Cognitive Impairment (MCI) Alzheimer’s Disease (AD) Vascular Dementia Lewy Body Dementia Frontal Lobe dementia Mixed Dementia Definition • According to the Diagnostic and Statistical Manual of Mental Disorders-IV-TR Multiple cognitive deficits • Memory impairment plus one or more: Aphasia Apraxia Agnosia Dysfunction is executive functioning Deficits must be severe enough to cause impairment in occupational and/or social functioning Epidemiology • Dementia Prevalence • Higher in women than men • Static's vary depending on the source 3.0% with MCI in adult population 1.4-1.6% for ages 65-69 to 16-25% over age 85 Alzheimer’s Disease • • • • 5.3 million people have AD 7th leading cause of death $172 billion dollars in annual costs 10.9 million unpaid caregivers DSM-IV; Alzheimer’s Association 2010 facts and figures Risk Factors for Dementia • Alzheimer’s Disease (AD) Age Family History ApoE E4 genetic allele History of psychiatric illness • Vascular Dementia (VaD) Age Conditions altering vasculature Smoking Neuropathology in Brief • AD B-amyloid plaques • Leads to neuronal death Neurofibrillary tangles • Abnormal neurons die and form tangles Inflammation processes lead to neuronal death and plaque formations • VaD Disruptions of blood flow to different structures in the brain responsible for cognition, executive functioning and behavior Neurochemical Disruptions • Cholinergic Systems Plaque formations damage cholinergic neurons and result in decrease in cognition and memory • Glutamatergic System Plaque aggregation disrupts transmission of glutamate which results in stimulation of NMDA • This can lead to excitotoxicity and neuronal death Morbidity and Mortality • Cognitive and behavioral symptoms are seen in earlier stages • High rates of depression in patients and caregivers • Late stages require extensive care with ADL • Death occurs due to complications Aspiration Infection Falls and other injuries Differential Diagnosis • Delirium Sudden alterations in cognition Fluctuations throughout the day Impaired attention span Disturbances in sleep-wake cycle and psychomotor activity Maybe due to medical condition or medications • Other psychiatric disorder Mood disorder • Substance abuse and or withdrawal Pharmacology in Geriatrics • Medication use in geriatrics 35% of all prescriptions dispensed 50% of all OTC medications • Polypharmacy 4-5 medications At least 2 OTC medications regularly • In 2000, estimates 106,000 deaths from medication errors Annual cost of $85 billion Fick et al. Arch Intern Med 2003; 163: 2716-2724 Geriatric Pharmacokinetics • Absorption Generally unaffected • Distribution Decreased total body water Increased body fat Decreased serum albumin • Metabolism Decreased hepatic blood flow and metabolizing enzymes • Excretion Decreased renal function Geriatric Pharmacodynamics • Dopaminergic Decreased D2 receptors in striatum • Serotonergic Decreased nerve terminals and transporters • Cholinergic system Decreased choline acetyltransferase and cholinergic cells Zubenko et al. Harvard Rev Psychiatry 2000 • Gaba-ergic system Potential increase in response to potentiation at GABA receptors • Adrenergic system Impaired baroreceptor function may result in orthostasis Prescribing in Geriatrics • Complete and thorough medication reconciliation • Reduce polypharmacy • Appropriate dosing and drug selection • Utilizing pharmacists for consultation and effective communication/education • Medication education focused on compliance and adherence Geriatric Medicine: An Evidence Based Approach - 4th Ed. (2003) Pharmacist Intervention • Screen for medication interactions • Screen for medications that impair cognition or have anticholinergic side effects • Prepared with alternate medication recommendations Approach to Dementia Consult Always look at the overall picture of your patient • Environment Busy or loud unit New people with each shift change • Medical conditions HPI and PMH Order/Assess pertinent labs • Life-style changes Recent move to care facility Recent loss of loved one(s) • Address differential diagnosis Delirium Medical condition Psychiatric disorder Substance induced • Address medications known to alter cognition Beers Criteria Medications with anticholinergic properties Drug Interactions • Occur when the effectiveness or toxicity of a drug is altered by the concomitant administration of another drug • 3 classifications of drug interactions Pharmaceutic • Physical or chemical incompatibility Pharmacodynamic • Addition, synergism or antagonism of each drug’s effect Pharmacokinetic • Changes in blood levels of the object drug Medications in Delirium • Many drugs are suspect in delirium or cognitive impairment cases Psychoactive meds suspect in 15-75% of cases Identified as definite cause in only 2-14% • There are not many well designed studies examining drug-induced delirium The studies have conflicting results, vary in design and analysis Benzodiazepines and antipsychotics noted significant results in few studies Anticholinergics, anticonvulsants, antidepressants, antiemetics, antiparkinsonians, corticosteroids, H-2 antagonists, and NSAIDs were not significantly associated with delirium • Critical review conclusions: the current evidence of an association of specific medications and delirium is rather weak. Gaudreau JD, et al. Psychosomatics 2005; 46(6): 302-316 Medications in Delirium Medication Class Benzodiazepines Medication Medication Class Antidepressants Opioids Dopaminergic Agents Corticosteroids Amantadine Levodpa Bromocriptine Prednisone NSAIDs Diclofenac Ibuprofen Sulindac Indomethacin Salicylic acid Ketoprofen Antihypertensives Enalapril Captopril Lisinopril Reserpine Clonidine Methyldopa Nifedipine Verapamil Atenolol Metoprolol Propranolol Antipsychotics Clozapine * Fluphenazine Haloperidol Loxapine Olanzapine Perphenazine Quetiapine Risperidone Thioridazine Ziprasidone Antiarrhythmics Amiodarone Lidocaine Quinidine Tocainide Anticholinergics Atropine Benztropine Scopolamine Tolterodine Antimicrobials Tobramycin Bactrim Linezolid Other Agents Antiasthmatics Theophylline Anticonvulsants Phenytoin Acetazolamide Lamotrigine Pregabalin Valproic Acid* Digoxin Alcohol withdrawl Lithium * * Documented incidence from clinical trials Medications that have anticholinergic effects which can be associated with cognitive impairment Borovick and Fuller. Drug-Induced Diseases: Prevention, Detection, and Management: 2nd ed. ASHP 2010; Chapter 15: Delirium. Amitriptyline Desipramine Doxepin Imipramine Protriptyline Mirtazapine Fluoxetine Paroxetine Sertraline Lorazepam Diazepam Clonazepam Alprazolam Triazolam Clorazepate Fentanyl * Meperidine * Morphine * Medication Beers Criteria • Based on expert consensus Extensive literature reviews • Utilization of the medications on the list Increase provider/facility cost Increase inpatient, outpatient and emergency visits • Centers for Medicare and Medicaid (CMS) utilized in nursing home regulation • Last updated in 2002 Fick DM, et al. Arch Intern Med 2003; 163: 2716-2724 Abbreviated Beers Criteria Drug Propoxyphene and combinations Indomethacin Pentazocine Trimethobenzamide Muscles relaxants and antispasmodics Flurazepam Amitriptyline Doxepine Meprobamate Specific dosing of benzodiazepines Lorazepam > 3 mg Oxazepam > 60 mg Alprazolam > 2 mg Temazepam > 15 mg Triazolam > 0.25 mg Long-acting benzodiazepines Chlordiazepoxide Diazepam Quazepam Halazepam Chlorazepate Concern Demonstrates analgesic effects similar to acetaminophen with adverse effects of narcotics Produces most CNS effects of the NSAID class Narcotic with several CNS effects: confusion and hallucinations Poor antiemetic effects; potential for EPS Poorly tolerated in elderly; anticholinergic effects; increase fall risk Severity Rating Low High High High High Extremely long half-life cause prolonged side effects of sedation and falls Potent anticholinergic; sedating Potent anticholinergic; sedating Highly addictive anxiolytic Doses ranging higher than those suggested demonstrate little benefit with increased side effects compared to smaller doses High Long half-life produces prolonged sedation and increased risk for falls High High High High Abbreviated Beers Criteria Disopyramide Digoxin Short-acting dipyridamole Methyldopa Reserpine > 0.25 mg Chlorpropamide GI antispasmodics Dicyclomine Hyoscyamine Belladonna alkaloids Clidiniumchlordiazapoxide Anticholinergics/Antihistamines Chlorpheniarmine Diphenhydramine Hydroxyzine Cyproheptadine Promethazine Diphenhydramine Ferrous Sulfate > 325 mg/day Barbiturates (except Phenobarbital) Particular antiarrhythmic may induce heart failure in elderly; also anticholinergic effects Closely monitor renal clearance and levels to prevent toxicity Potential for orthostatic hypotenstion; long-acting formulation only in those with prosthetic heart valves Bradycardia; may potentiate depression May induce depression, impotence, sedation, orthostatic hypotension Long half-life may prolong hypoglycemia Increased anticholinergic effects; efficacy uncertain High Potent anticholinergic High Confusion and sedation; use lowest possible dose in allergic reactions High doses not dramatically absorbed; constipation greatly increased Highly addictive; harmful side effects High Low Low High Low High High Low High Abbreviated Beers Criteria Meperidine Ticlopide Ketorolac Amphetamines Long-term use of NSAIDs Bisacodyl Amiodarone Fluoxetine (daily dosing) Nitrofurantoin Doxazosin Methyltestosterone Short acting nifedipine Clonidine Mineral oil Cimitidine Ethacrynic acid Estrogens only agents Advantage over other analgesics questionable; increased side effects No more efficacious than aspirin for clots; more side effects Use (especially long-term) associated with GI side effects Addictive; Induce hypertension, angina, and myocardial infarction GI bleeds, renal failure, high blood pressure, heart failure Long-term use may exacerbate bowel dysfunction May prolong QT interval; questionable efficacy in elderly Long half-life may prolong CNS stimulation, sleep disturbances, agitation Renal impairment Hypotention; anticholinergic effects Prostatic hypertrophy; cardiac issues Hypotension; constipation Hypotension; CNS effects Risk for aspiration and other side effects Increased CNS effects (confusion); drug interactions Hypertension; fluid imbalances Evidence of carcinogenic potential and lack of cardio-protective effects in elderly women High High High High High High High High High Low High High Low High Low Low Low Notes: Abbreviations: CNS- central nervous system; NSAIDs- nonsteroidal anti-inflammatory drugs; EPS- extrapyramidal symptoms Anticholinergic effects- may effect several different systems; most notable effects include: ataxia, dry mouth and eyes, blurred vision, constipation, tachycardia, light-headedness urinary retention, confusion, and agitation. Tips for Recommendations • Always include non-medication factors in consults if pertinent Environment Medical condition - Pain control - Daily routine • Approach medication changes, discontinuations and/or additions one at a time Multiple changes that occur rapidly could exacerbate cognitive or behavioral changes • Just because a medication might be found on the Beers Criteria or associated with delirium it might still be necessary Assess the current medical illness and past medical conditions prior to changing a therapy and weight the risk vs. benefit Questions???