Pharmacology of commonly used drugs
advertisement

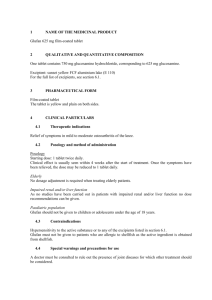
Pharmacology of commonly used drugs in musculoskeletal disorders Mr. Harish Kurup Consultant in Orthopaedics Pilgrim Hospital, Boston Paracetamol / Acetaminophen Paracetamol (called acetaminophen in the USA) is a derivative of p-aminophenol, which corresponds to the active principal metabolite phenacetin. Paracetamol inhibits prostaglandin biosynthesis in the central nervous system but hardly in the peripheral tissues. Paracetamol only has minimal anti-inflammatory action compared to nonsteroidal anti-inflammatory agents. Indications Paracetamol has good analgesic and antipyretic properties. It is suitable for the treatment of pain from any orthopaedic pathology and is usually the first line drug. In general, Paracetamol is less efficacious than salicylates and other antirheumatic agents for problems that require anti-inflammatory treatment. Paracetamol is well suited for use in children. Paracetamol appears to have little potential for dependence. Paracetamol is safe in pregnancy and lactation. Adverse reactions Paracetamol only rarely causes gastrointestinal problems or allergic skin reactions. Blood dyscrasia (e.g. thrombocytopenia), and haemolytic anaemia are very rare. A minority of the responds to Paracetamol with bronchospasms. It is not safely established if Paracetamol can cause a nephropathy, like drug combinations containing phenacetin. When metabolized in the liver, small amounts of an intensely active metabolite, which is normally immediately inactivated by glutathione, are produced. An overdose causes a glutathione deficiency; the reactive metabolite may then cause hepatocellular damage and necrosis leading to acute liver failure. Toxic effects have been observed in adults treated with doses of more than 10 g (20 tablets). However, if there is a preexisting liver insufficiency, Paracetamol can be hepatotoxic even in small amounts. The antidote N- acetyl cysteine must be administered within 8 to 10 hours when there is intoxication. Contraindications Hypersensitivity to Paracetamol. NSAID Non-steroidal anti-inflammatory drugs Ibuprofen and Diclofenac are the most commonly used NSAIDs. Ibuprofen Ibuprofen, a non-steroidal anti-inflammatory agent belonging to the group of propionic acid derivatives, inhibits the enzyme cyclo-oxygenase (prostaglandin synthesis) which catalyzes the transformation of unsaturated fatty acids to prostaglandins. The inhibition of the prostaglandin synthesis is the mechanism for the analgesic, antipyretic, and anti-inflammatory action of the drug. Indications Ibuprofen is suited for the treatment of pain, in particular of pain related to the musculoskeletal system. Pain accompanying arthritis can be reduced and the mobility of the joints can be increased. Non-steroidal anti-inflammatory agents only have a symptomatic effect on joint diseases; the development of the disease is not significantly influenced. In average, ibuprofen has proven equally as efficient as other anti-inflammatory drugs in all areas of application (e.g. diclofenac, indomethacin, and naproxen). Adverse reactions Ibuprofen predominantly causes gastrointestinal problems (dyspepsia, nausea, vomiting, epigastric pain, rarely diarrhoea or constipation). According to different studies, ibuprofen seems to cause fewer such side-effects than many other antiinflammatory agents. Dangerous complications (bleeding ulcers, perforations) are not common. Anti-inflammatory drugs have other side-effects like vertigo, headaches, skin rashes, increase of liver enzymes, etc. Dangerous renal complications (water and salt retention, acute renal failure), hepatitis, and general hypersensitive reactions (fever, hypertension, and aseptic meningitis) are rare. Contraindications Hypersensitivity to aspirin (acetylsalicylic acid) or other non-steroidal antiinflammatory agents. Active peptic ulcer. Safe in pregnancy (avoid in the last 3 months – can cause premature closure of ductus arteriosus) Diclofenac Like other non-steroidal anti-inflammatory agents, diclofenac, a phenylacetic acid derivative, inhibits the prostaglandin biosynthesis. Indications The efficacy of Diclofenac as an anti-inflammatory agent and analgesic is well documented: in comparison with many other anti-inflammatory agents (e.g. ibuprofen, indomethacin, naproxen, piroxicam) Diclofenac has proven to be about equal. Like other non-steroidal anti-inflammatory agents, Diclofenac only produces a symptomatic effect. Diclofenac is available in both oral and paraenteral forms. Diclofenac is also available in ointments and gels. Adverse reactions Diclofenac causes gastrointestinal problems (upper abdominal and gastric pain, nausea, vomiting, diarrhoea or constipation) in more than 5% of the treated subjects. Headaches, vertigo and sleep disturbances are also observed occasionally. Haematological problems (e.g. granulocytopenia), increased liver enzymes, exanthemas and renal function disorders are less frequent. Dangerous reactions such as bleeding gastric ulcers, perforations, hepatitis and renal failure are rare. Patients with pre-existing heart failure, hypertension or renal failure are more prone to the development of renal function disorders and should be observed closely after the beginning of the treatment. Contraindications Active gastric or duodenal ulcers. Aspirin intolerance. All NSAIDs are better avoided in third trimester of pregnancy. Codeine Codeine is an opioid (methylmorphine) with a relatively limited analgesic effect; it does not cause significant respiratory depressions. In most humans 10% of a codeine dose is transformed to morphine through demethylation in the liver. Indications Codeine is suitable for the treatment of mild and moderate pain. A minority of the population does not respond to the analgesic effect. Codeine can be combined advantageously with non-opioid analgesics. Aspirin (500 mg), Paracetamol (500 mg), or other more recent non-steroidal anti-inflammatory agents can be suitably combined with codeine (30 mg). Adverse reactions In many cases the imperative constipating effect of codeine is undesired and it is often a reason against long-term use of the drug. Vomiting and nausea also occur regularly. All the other opioid side-effects are also present with codeine but they are comparatively mild. Retention of urine, itching, vertigo, palpitations or bradycardia, sweating, and mild central nervous effects (sedation, mood changes, and some hallucinations) have been observed. A respiratory depression under therapeutic doses is very rare. There is a danger of addiction for subjects with a former or present dependence of the opioid type. Contraindications Advanced respiratory insufficiency, bronchial asthma, raised intracranial pressure. Better avoided in late stages of pregnancy and young children. Morphine Morphine is the principal medical alkaloid of opium. Its effect at the µ-receptors in the central nervous system is said to be responsible for analgesia, euphoria, dependence potential and respiratory depressions. Morphine also binds with kreceptors which mediate spinal analgesia, miosis and sedation. Indications Morphine still is the drug of choice for the treatment of severe acute or chronic pain. It is mostly used parenterally for acute pain (multiple injuries, post-operative). Morphine is also frequently injected to prepare for surgery and it can also be given during the operation for the suppression of nociceptive stimuli. Adverse reactions Morphine causes a wide range of side-effects. However, severe reactions such as respiratory depressions and pronounced hypotension are uncommon when the drug is used therapeutically. Drop in blood pressure due to a cardiac infarction or hypovolemia can have dangerous results. Constipation is the most important problem in long-term treatment. Even therapeutic doses can reduce respiratory frequency and can cause oliguria or urinary retention. Further potential side-effects are euphoria and dysphoria, anxiety, pruritis, urticaria, bronchospasms, spasms of the sphincter oddi, oedemas, headaches and miosis. Development of tolerance entails ever-increasing doses. Naloxone is used for reversing the respiratory depression caused by Opiods. Contraindications Advanced respiratory insufficiency, raised intracranial pressure. Steroids for injection (Also read chapter on injection techniques) Corticosteroids are hormones that are produced naturally by the adrenal glands. They have many important functions in the body, including control of inflammatory responses. Corticosteroid medicines are man-made derivatives of the natural hormones. Triamcinolone Triamcinolone is a synthetic steroid that has an anti-inflammatory effect. It is the most common choice for joint injection. Local complications: - may cause fat necrosis and loss of skin pigmentation - In some cases may accelerate joint degeneration - systemic absorption may occur from intra-articular injection - absorption is increased by usage of water soluble preparations, dose injected, and injection into multiple joints - may cause transient hyperglycemia in diabetic patients (and therefore is advised in type I or brittle diabetics) - avascular necrosis of the femoral head is a rare complication - iatrogenic septic arthritis is uncommon problem but it does occur, so all joint injections should be performed using sterile technique, with a formal betadine prep and use of sterile gloves Triamcinolone Preparations for Intra-articular Injection Triamcinolone hexacetonide (Aristospan) - Used for large joints - has a tendency to cause skin atrophy and hypopigmentation - has a long lasting effect Triamcinolone acetonide (Kenalog) - Used for small and medium sized joints - small joint might receive 10 mg of Kenalog, and larger joints 40 mg Glucosamine Glucosamine is an amino sugar and a prominent precursor in the biochemical synthesis of glycosylated proteins and lipids. Glucosamine is one of the most abundant monosaccharides. It is produced commercially by the hydrolysis of crustacean exoskeletons or, less commonly by fermentation of a grain such as corn or wheat. In body glucosamine forms the precursor of glycosaminoglycans, proteoglycans, and glycolipids. Oral glucosamine is commonly used for the treatment of osteoarthritis. Since glucosamine is a precursor for glycosaminoglycans, and glycosaminoglycans are a major component of joint cartilage, supplemental glucosamine may help to rebuild cartilage and treat arthritis. Its use as a therapy for osteoarthritis appears safe, but there is conflicting evidence as to its effectiveness. A Cochrane review in 2005 has found no advantage of glucosamine over placebo in treatment of arthritis. The possible effects of glucosamine sulfate in patients with osteoarthritis may be the result of its anti-inflammatory activity, the stimulation of the synthesis of proteoglycans and the decrease in catabolic activity of chondrocytes inhibiting the synthesis of proteolytic enzymes and other substances that contribute to damage cartilage matrix and cause death of articular chondrocytes. Clinical use Commonly sold forms of glucosamine are glucosamine sulfate and glucosamine hydrochloride. A typical dosage of glucosamine salt is 1,500 mg per day. Glucosamine is often sold in combination with other supplements such as chondroitin sulfate and methylsulfonylmethane. Safety Clinical studies have consistently reported that glucosamine appears safe. Since glucosamine is usually derived from shellfish, those allergic to shellfish may wish to avoid it. It does not interfere with control of diabetes. Chondroitin sulphate Chondroitin sulfate is a sulfated glycosaminoglycan (GAG) composed of a chain of alternating sugars (N-acetylgalactosamine and glucuronic acid). It is usually found attached to proteins as part of a proteoglycan. Chondroitin sulfate is an important structural component of cartilage and provides much of its resistance to compression. The benefit of chondroitin sulfate in patients with osteoarthritis is likely the result of a number of effects including its anti-inflammatory activity, the stimulation of the synthesis of proteoglycans and hyaluronic acid, and the decrease in catabolic activity of chondrocytes inhibiting the synthesis of proteolytic enzymes, nitric oxide and other substances that contribute to damage cartilage matrix and cause death of articular chondrocytes Clinical use Chondroitin is an ingredient found commonly in dietary supplements used as an alternative medicine to treat osteoarthritis. Chondroitin appears to be made from extracts of cartilaginous cow and pig tissues (cow trachea and pig ear and nose), but other sources such as shark, fish and bird cartilage are also used. Safety Clinical studies have not identified any significant side effects or overdoses of chondroitin sulfate, which supports its long-term safety.