ROLE OF MAGNETIC RESONANCE IMAGING
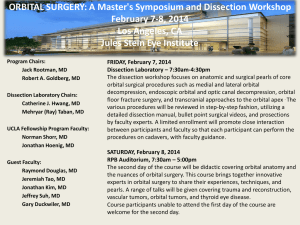
advertisement

EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ ROLE OF MAGNETIC RESONANCE IMAGING IN DIAGNOSIS OF OCULAR AND ORBITAL DISEASES By Hosam A.I. Elzembely, M.D.*, Alaa A.Fathy, M.D.*, Shaaban A. Mehanny, M.D. *, Hosny S. Abdel-Ghany, M.D.** and Rabie M. Hassanain, M.D.* Department of *Ophthalmology, **Radiology; Minia Faculty of Medicine ABSTRACT: Purpose The aim of this study is to evaluate the role of MRI with its advanced techniques in diagnosis of orbital and ocular masses and ocular masses. Methods 28 patients (32 eyes), age range from 6-62 years (mean 34 ± 1.6), 11 males and 17 females. Each patient was submitted to full ophthalmological examination. Some patients were subjected to Ultrasonography, Fluorescein angiography and CAT scan. MRI was done using Philips gyroscan 1 tesla machine with standard head coil in every case. Results The direct sagittal images gave detailed anatomic information. The characterization of hemorrhage is more sensitive than in CAT scan. The vascularity and intravascular flow are easier to appreciate. The combination of T1- and T2- weighted images some diseases as ocular melanoma give some diagnostic specificity. Conclusion MRI is a superb diagnostic technique in the study of ocular and orbital diseases. It adds important anatomical and pathological information to the current available ophthalmic diagnostic tools. KEYWORDS: MRI Radio Magnetic Imaging INTRODUCTION: The diagnosis of the intraocular lesions is mainly made by ophthalmoscopy. Imaging studies as ultrasonography, computed tomography and magnetic resonance imaging are used to confirm the diagnosis as well as assisting in evaluation of cases with opaque media. The non-ionizing magnetic resonance image studies in contrast to ionizing CT provides a superior soft tissue Orbital diseases Resonance. resolution. Early reports of MRI of the eye ball described the technical limitations and hinted at future improvement.1 The development of fat suppression techniques, surface coil receivers and the use of contrast material had greatly improved the quality of MRI.2 200 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ Aim of the study The aim of this study is to evaluate the role of MRI with its advanced techniques in diagnosis of orbital and ocular masses. PATIENTS AND METHODS: 28 patients (32 eyes), age range from 6-62 years (mean 34 ± 1.6), 11 males and 17 females. MRI protocols • T1W1 in axial, coronal and sagittal planes. • T2W1 axial. • SPIR (fat suppression) axial. • Post Gadolinium T1W1 coronal and sagittal. • Post Gadolinium SPIR T1W1 on axial plane. (Contrast media used was Gadolinium DTPA, 1mm/Kg) • Setting: Al-Minya university mology department, department), Al-Minya Center Some patients were subjected to Ultrasonography, Fluorescein angiography and CAT scan. MRI was done using Philips gyroscan 1 tesla machine with standard head coil in every case. (OphthalRadiology Oncology Each patient was submitted to full ophthalmological examination. 201 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ RESULTS: Lesion Number of cases Malignant melanoma 2 Optic Neuritis (Fig. 1) 10 Orbital Pseudotumour (Fig. 2) 4 Orbital cellulitis 2 Orbital lymphoma (Fig. 3) 2 Optic nerve meningioma (Fig. 4) 2 Orbital dermoid (Fig. 7) 4 Orbital cavernous haemangioma (Fig. 5) 4 Rhabdomyosarcoma 1 Lymphangioma (Fig. 6) 1 Figure 1 Figure 2 Figure 3 Figure 4 Figure 5 Figure 6 Figure 7 Optic neuritis MRI demonstrating optic nerve white matter hyperintensity Pseudotumor: (a, b)Coronal & Sagittal T1W1 Post contrast “diffuse enlargement of all groups of Rt EOMs” (c, d) SPIR postcontrast axial images “more evident hyperintense involved muscles” Lymphangioma: (a, b) Axial & Sagittal T1W1 “extraconal swelling at the medial aspect of the Rt orbit with fluid levels” (c) Coronal T2W1 “well demarcated”,(d) SPIR non-contrast “hyperintense lesion” Optic N. Sheath meningioma: (a, b) Axial T1W1 “Mass encircling the optic nerve” (c) Sagittal T2W1 “hypointense lesion” (d) Axial SPIR “marked enhancement” “compare with b” Cavernous Hemangioma: (a) Coronal T1W1 “Extraconal Hypointense” (b) Sagittal T1W1 postcontrast “mottled contrast enhancement” (c, d) Dynamic Contrast “evident opacification with pooling of contrast” Lymphoma: (a) Coronal T2W1 “diffuse enlargement of Lt IR muscle, hypointense” (b) Sagittal T1W1 “enhanced compared to adjacent brain” (c) SPIR non-contrast “Hyperintense” (d) SPIR contrast “Hyperintense” Orbital Dermoid: (a) Coronal T2W1 “Heterogenous soft tissue lesion” (b) Sagittal T1W1 (c) Axial SPIR T1W1 non-contrast “Hypointense” (d) Axial SPIR T1W1 post-contrast “NO contrast enhancement” 202 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ 203 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ superior soft tissue resolution and allow the identification of tissue compounds as melanin, met-hemoglobin and proteinaceous fluid. As regards safety, the non-ionizing MRI is safer than the ionizing CAT scan especially on repeated exposures 1 DISCUSSION: In 2005 a study at Jules Stein Eye Institute on 131 cases with biopsy proven orbital tumours – with prospective evaluation of the CT and MRI imaging – put the guide lines for reviewing orbital imaging. They applied 83 features base don 5 major characteristics (anatomic location \ bone and para nasal sinuses involvement \ content \ shape \ and associated features. This study is considered a mile stone in the interpretation of MRI and CT imaging.4 Significant diagnostic information is available with MRI: • First, the direct sagittal images gave detailed anatomic information. • Second, the characterization of hemorrhage is more sensitive than in CAT scan. • Third, the vascularity and intravascular flow are easier to appreciate. • Fourth, with the combination of T1- and T2- weighted images some diseases as ocular melanoma give some diagnostic specificity. Ocular US is a useful office imaging tool in many ocular and orbital diseases, but it can easily miss intraocular calcifications and it has a poor diagnostic value for orbital disease.5 Newer MRI techniques such as diffusion weighted MRI 4 and magnetic resonance spectroscopy proved to be helpful in the diagnosis and follow up of renal brain and soft tissue tumors.6-10 Magnetic resonance spectroscopy also proved to be effective in differentiating metastatic brain tumors, radiation necrosis and brain abscess.3,11 CONCLUSION: MRI is a superb diagnostic technique in the study of ocular and orbital diseases. It adds an important anatomical and pathological information to the current available ophthalmic diagnostic tools. REFERENCES: 1. McCrohan JL, Patterson JF, Gange RM, Goldstein HA. Average radiation doses in standard head examination for 250CT systems. Radiology 1987 Apr. 163 (1): 55-62. 2. Lee AG, Brazis PW, Garrity JA, White M. Imaging for neuro-ophthalmic and orbital disease. Am J Ophthalmol 2004; 138: 852-862. 3. Hakyemez B, Ergin N, Uysal S, Isik I, Kilic E. Diffusion-weighted MRI in the differentiation of brain abscesses and necrotic tumors. Tani Girisim Radyol 2004; 10(2): 110-8. 4. Ben Simon GJ, Annunziata CC, Fink J, Villablanca P, McCann JD, Goldberg RA. Rethinking orbital As regards the cases of orbital pseudo tumors MRI proved to be very helpful in diagnosis, evaluation and assessment of its intracranial 12-19 extension. Another important condition in which MRI is extremely helpful is Tolosa-hunt syndrome. MRI studies with contrast enhancement showed abnormality in the cavernous sinus and proved definitely to be superior than CT scanning in such conditions.20,21,22 CAT scan can detect those calcifications which were missed by US examination MRI provides a 204 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ imaging establishing guidelines for interpreting orbital imaging studies and evaluating their predictive value in patients with orbital tumors. Ophthalmology. 2005 Dec; 112(12): 2196-207 5. Romano A, Bozzao A, Bonamini M, Fasoli F, Ferrante, Floris R, Colonnes C, Fantozzi LM. Diffusion-weighted MR imaging: clinical applications in neuroradiology. Radiol Med 2003; 106 (5-6): 521-48. 6. Gujar SK, Maheshwari S, BjorKman-Burtscher I, Sundgren PC. Magnetic resonance spectroscopy. J neuroophthalmol 2005; 25 (3): 217-26. 7. Wang CK, Li Cw, Hsieh TJ, Chien SH, Liu GC, Tasi KB. Characterization of bone and soft tissue tumors with in vivo 1H MR spectroscopy: initial results. Radiology 2004; 232 (2): 599-605. 8. Rock JP, Scarpace L, Hearshen D, Gutierrez J, Fisher JL, Rosenblum M, Mikkelsen T. Association among magnetic resonance spectroscopy, apparent diffusion coefficients, image guided histopathology with special attention to radiation necrosis. Neurosurgery 2004; 54 (5): 1111-7. 9. Sartor K, Hartmann M, Fiebach J, Harting I, Wilhelm T, Heiland S. Normal and abnormal water diffusion in the brain. Rofo. 2003; 175 (10): 1317-29. 10. Squillaci E, Manenti G, Di Stephano F, Miano R, Strigari L, Simonetti G. Diffusion-weighted MR imaging in the evaluation of renal tumours. J Exp Clin Cancer Res 2004; 23 (1): 39-45. 11. Hwang YF, Huang TY, Hwang SL, Kwan AL, Howng SL. Differentiation among metastatic brain tumors, radiation necroses, brain abscesses using proton magnetic resonance spectroscopy. Kaohsiung J Med Sci 2004; 20 (9): 437-42. 12. Bencherif B, Zouaoui A, Chedid G, Kujas M, Van Effenterre R, Marsault C. Intracranial extension of an idiopathic orbital inflammatory pseudotumor. AJNR Am J Neuroradiol 1993;14:181-184. 13. De Jesus O, Inserni JA, Gonzalez A, Colon LE. Idiopathic orbital inflammation with intracranial extension. J Neurosurg 1996;85:510513. 14. Frohman LP, Kupersmith MJ, Lang J, Reede D, Bergeron RT, Aleksic S, et al. Intracranial extension and bone destruction in orbital pseudotumor. Arch Ophthalmol 1986;104:380-384. 15. Weber AL, Romo LV, Sabates NR. Pseudotumor of the orbit. Clinical, pathologic, and radiologic evaluation. Radiol Clin North Am 1999;37:151-68. 16. Noble SC, Chandler WF, Lloyd RV. Intracranial extension of orbital pseudotumor: a case report. Neurosurgery 1986;18:798-801. 17. Kaye AH, Hahn JF, Craciun A, Hanson M, Berlin AJ, Tubbs RR. Intracranial extension of inflammatory pseudotumor of the orbit. J Neurosurg 1984;60:625-629. 18. Clifton AG, Borgstein RL, Moseley IF, Kendall BE, Shaw PJ. Intracranial extension of orbital pseudotumor. Clin Radiol 1992;45:23-26. 19. Ayala AS, Fernandez Sarabia T, Cabeza Martinez B, Moya MJ, Menendez FL, Garcia PZ. Orbital pseudotumor with intracranial extension. Eur Radiol 2000;10:1505. 20. Desai SP, Carter J, Jinkins JR. Contrast-enhanced MR imaging of Tolosa-Hunt syndrome : A case report. AJNR Am J Neuroradiol 1991; 12: 182-183. 21. Goto Y, Hosokawa S, Goto I, Hirakata R, Hasuo K.Abnormality in the cavernous sinus in three patients with Tolosa-Hunt syndrome : MRI and CT findings. J Neurol Neurosurg Psychiatry 1990;53:231-234. 205 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Elzembely et al __________________________________________________________________________________ 22. De Arcaya AA, Cerezal L, Canga A, Polo JM, Berciano J, Pascual J. Neuroimaging diagnosis of Tolosa- Hunt syndrome MRI contribution. Headache 1999;39:321-325. دور أشعة الرنين المغناطيسى فى تشخيص أمراض العين والحجاج حسام عبد الحميد ابراهيم الزمبيلى* -عالء أحمد فتحى* -شعبان عبدالحميد مهنى* حسنى سيد عبدالغنى** -ربيع محمد حسانين* أقسام *طب وجراحة العيون و**االشعة كلية طب المنيا الغرض من الدراسة تقييم دور الرنين المغناطيسى بتقنياته الحديثة فى تشخيص وعالج أمراض العين والحجاج. طرق البحث ثمانىة وعشرون مريضا (اثنان وثالثون عينا) ،يتراوح عمرهم من ستة الى اثنان وستون عاما (متوسط اربعة وثالثون عاما) .تم اخضاع كل مريض لفحص عين شامل ,بعض المرضى احتاجوا للخضوع ألشعة تليفزيونية وتصوير قاع العين بالصبغة وأشعة مقطعية بالكمبيوتر .تم استخدام جهاز فيليبس جيروسكان واحد تسال فى اجراء أشعة الرنين المغناطيسى للمرضى. النتائج تم اظهار النزيف بصورة أوضح فى أشعة الرنين المغناطيسى عنها باالشعة المقطعية بالكمبيوتر .الدموية ومرور الدم فى االوعية الدموية كانت ايضا أكتر وضوحا .استخدام مزيج من صور ت 1و ت 2كان ذاقيمة تشخيصية كبيرة فى حاالت االورام الصبغية الخبيثة الخالصة أشعة الرنين المغناطيسى ذات قيمة تشخيصية كبيرة فى أمراض العين والحجاج ,فهى تضيف قيمة تشريحية و باثولوجية كبيرة الى الوسائل التشخيصية المتاحة حاليا فى تشخيص أمراض العيون الكلمات المفتاحية اشعة الرنين المغناطيسى \ امراض الحجاج 206