Quick Solutions for Iliotibial
Band Syndrome
Michael Fredericson, MD; Marc Guillet, PT, ATC; Len DeBenedictis, MS, CMT
THE PHYSICIAN AND SPORTSMEDICINE - VOL 28 - NO. 2 - FEBRUARY 2000
In Brief: Though recognizing the sharp, burning lateral knee pain of iliotibial band syndrome
isn't difficult, treating the condition can be a challenge because underlying myofascial
restrictions can significantly contribute to the patient's pain and disability. The physical exam
should include a thorough evaluation to identify tender trigger points as well as tenderness and
possible swelling at the distal iliotibial band. After acute symptoms are alleviated with activity
restriction and modalities, problematic trigger points can be managed with massage therapy or
other treatments. A stepwise stretching and strengthening program can expedite patients'
return to running.
Iliotibial band syndrome (ITBS) is the most common cause of lateral knee pain in runners,
with an incidence as high as 12% of all running-related overuse injuries (1-4). ITBS is believed
to result from recurrent friction of the iliotibial band (ITB) sliding over the lateral femoral
epicondyle.
Low mileage, recreational runners usually improve with a simple regimen of anti-inflammatory
medication and appropriate stretches; however, higher mileage, competitive runners typically
require a more comprehensive treatment approach. In our experience caring for the Stanford
University track and cross-country teams, we have had good success with an aggressive
treatment algorithm (table 1) that expedites recovery and return to high-level training.
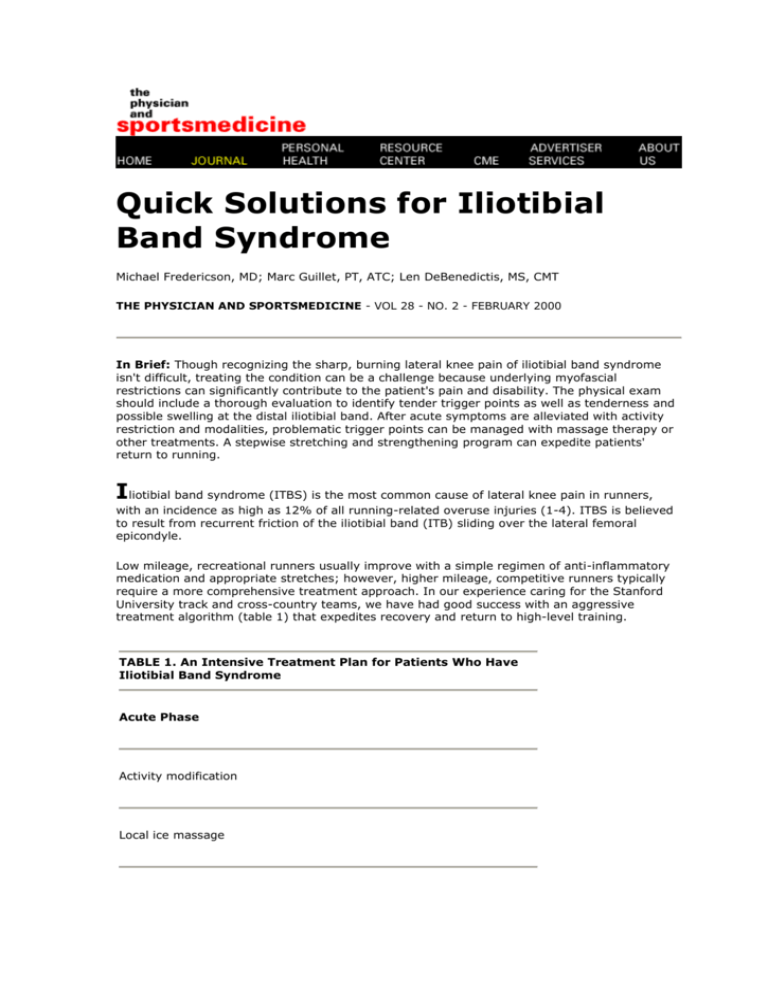
TABLE 1. An Intensive Treatment Plan for Patients Who Have
Iliotibial Band Syndrome
Acute Phase
Activity modification
Local ice massage
Nonsteroidal anti-inflammatory medication
Phonophoresis
Corticosteroid injection if swelling lasts more than 3 days
Subacute Phase
Stretching exercises
Myofascial therapy
Recovery Phase
Progressive strengthening exercises: side-lying leg lifts, step-down
exercises, pelvic drops
Return to Running
Easy sprints
Gradual increase in distance and frequency
The Role of the Iliotibial Band
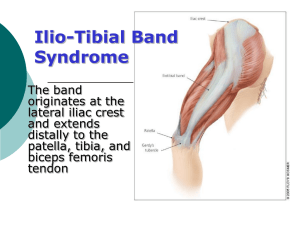
Anatomy. The ITB is considered a continuation of the tendinous portion of the tensor fascia
lata muscle and is indirectly attached to parts of the gluteus medius, gluteus maximus, and the
vastus lateralis muscles. The intermuscular septum connects the ITB to the linea aspera femoris
until just proximal to the lateral epicondyle of the femur (5,6). Distally, the ITB spans out and
inserts on the lateral border of the patella, the lateral patellar retinaculum, and Gerdy's tubercle
of the tibia. The ITB is only free from bony attachment between the superior aspect of the
lateral femoral epicondyle and Gerdy's tubercle (6).
Controlled adduction. The ITB assists the tensor fascia lata as it abducts the thigh or, more
precisely, controls and decelerates adduction of the thigh. The ITB may also act as an
anterolateral stabilizer of the knee (6). The ITB moves anterior to the epicondyle as the knee
extends and slides posteriorly as the knee flexes, remaining tense in both positions (5).
Symptomatic impingement. A biomechanical study (7) of runners who had ITBS found that
the posterior edge of the band impinges against the lateral epicondyle just after foot strike in
the gait cycle. The friction occurs at or at slightly less than 30° of knee flexion. Recurrent
rubbing can produce irritation and subsequent inflammation, especially beneath the posterior
fibers of the ITB, which are thought to be tighter against the lateral femoral condyle than the
anterior fibers (8).
Histopathologic studies (9) in patients who have chronic ITBS show that the tissue under the
ITB consists of synovium that is a lateral extension and invagination of the knee joint capsule,
rather than a separate bursa as previously described in the literature. One magnetic resonance
imaging study (10) also found that patients who have ITBS have significantly thicker bands than
those without symptoms.
What Causes ITBS?
A number of etiologic factors have been related to ITBS (1,3,8).
Mileage and knee flexion/extension weakness. In a retrospective study, Messier et al (11)
found that runners with ITBS were less experienced and were doing greater weekly mileage and
a greater percentage of their training on the track compared with noninjured runners. Also,
injured runners had weaker knee flexion and knee extension bilaterally, and they exhibited
lower maximal normalized braking forces.
Excessive pronation? The literature is contradictory regarding excessive pronation as a factor
in ITBS. James (12) observed that runners with ITBS often have genu varum and/or tibia vara,
heel varus, forefoot supination, and compensatory pronation. High-speed videography,
however, has shown that rear-foot motion in runners with ITBS differs little from that of a
control group; in fact, the control group had a slightly greater tendency to pronate than those
with ITBS. Others postulate that leg-length discrepancies contribute to ITBS. This can be
secondary to a true anatomic discrepancy or environmentally induced by training on crowned
roads (1,3,13).
Hip abductor weakness. Researchers at our institution (14) recently compared 24 distance
runners (14 women, 10 men) who had ITBS with noninjured controls and found that runners
with ITBS had significant weakness in the hip abductors of their affected limb. After 6 weeks of
rehabilitation directed at strengthening the gluteus medius, 92% of the runners were pain free.
Electromyographic studies of joggers (15) have shown that to control coronal plane motion
during the stance phase, the gluteus medius--and to a lesser extent the tensor fascia lata--must
exert a continuous hip abductor moment. The pattern of muscle action stays constant as gait
speed increases. At foot contact, the femur adducts relative to the pelvis. The involved muscles
contract eccentrically, then concentrically through the support phase and into the propulsive
phase as the hip abducts. Though the gluteus medius and tensor fascia lata are both hip
abductors, the gluteus medius (especially the posterior aspect) externally rotates the hip,
whereas the tensor fascia lata internally rotates the hip (16). Consequently, fatigued runners or
those who have a weak gluteus medius are prone to increased thigh adduction and internal
rotation at midstance, leading to an increased valgus vector at the knee. We postulate (14) that
this increases tension on the ITB, making it more prone to impingement on the lateral
epicondyle of the femur, especially during the early stance phase of gait (foot contact), when
maximal deceleration absorbs ground reaction forces.
The Patient Workup
History. The main symptom of ITBS is sharp pain or burning on the lateral aspect of the knee.
Runners often note that they start out running pain free but develop symptoms after a
reproducible time or distance. Early on, symptoms subside shortly after a run, but return with
the next run. If ITBS progresses, pain can persist even during walking, particularly when the
patient ascends or descends stairs.
Physical exam. The knee examination is typically negative except for local tenderness and,
occasionally, swelling over the distal ITB where the band moves over the lateral femoral
condyle. No tenderness is noted at the lateral joint line, popliteal tendon, lateral collateral
ligament, or anterior lateral fat pad. Occasionally, pain or paresthesia extends along the length
of the band. Crepitation, snapping, or mild pitting edema can occur over the affected area. Pain
may be elicited by having the patient lie on his or her side with the affected knee up and flexed
90°, and applying pressure to the ITB over the lateral femoral condyle while straightening the
knee. The test is positive if pain occurs as the knee approaches 30° of flexion, the position in
which the tensed ITB rubs directly over the lateral femoral condyle (8).
Locating myofascial restrictions. Severe lateral knee pain associated with ITBS may be
intensified by myofascial restrictions that are not directly associated with the friction of the ITB
sliding over the lateral femoral epicondyle. Myofascial restrictions include central and
attachment trigger points (17), muscle contractures, and fascial adhesions. These restrictions
may also contribute to excessive tension on the ITB, which underlies the friction syndrome, and
may precede and accompany the condition or linger after the primary friction syndrome has
subsided. We have found that myofascial restrictions vary from a minor complication to the
primary cause of the lateral knee pain.
Evaluation often reveals tender areas in the vastus lateralis, gluteus minimus, and distal biceps
femoris muscles. Within these tender areas, discrete trigger points are often found that can
refer pain to the lateral thigh, to the knee, or even to the lateral lower leg. Examination consists
of thorough and very firm palpation of the trigger points (figure 1). This is best performed with
the patient in a relaxed side-lying position with the hip on the symptomatic side flexed to about
45° and the knee slightly flexed. A pillow or bolster is placed under the leg to be palpated.
Central trigger points in the gluteus minimus and vastus lateralis muscles can refer intense pain
to the lateral knee that is indistinguishable from the pain caused by ITBS.
Attachment trigger points occur at the distal musculotendinous junctions of the vastus
lateralis and biceps femoris muscles and can refer sharp pain to the epicondyle. They
are caused by chronic muscle tension.
Contracture of the vastus lateralis muscle causes a deep-to-superficial displacement
that increases longitudinal tension on the ITB.
Fascial adhesions in the posterior fibers of the ITB, particularly distally, are common in
patients who have ITBS. These adhesions are often associated with burning pain and
may be the result of past injury or inflammation.
If the trigger points are sensitive and the patient reports sensations in the referral zones,
myofascial treatment is strongly indicated. If the tissues are very tight and sensitive but
produce no referral sensations, myofascial treatments are still likely to be effective. If no
contracture, sensitivity, or referral patterns are evident, myofascial treatments are not
indicated.
Tests. We perform the modified Thomas test (figure 2) (18,19) on all patients who have
suspected ITBS to evaluate for flexibility deficits in the iliopsoas, rectus femoris, and tensor
fascia lata/ITB.
We also evaluate gastrocnemius and soleus muscle flexiblity (figure 3) and gluteus medius
muscle strength (figure 4: not shown) (18,19). Tightness of the gastrocnemius-soleus complex
will limit ankle dorsiflexion, increase subtalar pronation, and increase knee flexion.
A thorough evaluation should also include gait and treadmill running analyses to screen for
dynamic muscle imbalance or weakness contributing to the injury.
Differential diagnosis. The differential diagnosis for lateral knee pain includes primary
myofascial pain, patellofemoral stress syndrome, early degenerative joint disease, lateral
meniscal pathology, superior tibiofibular joint sprain, popliteal or biceps femoris tendinitis,
common peroneal nerve injury, and referred pain from the lumbar spine. In most patients,
these conditions can easily be ruled out with a careful history and physical examination. A local
anesthetic injection may help differentiate soft-tissue pain from intra-articular or referred pain.
Treatment and Rehabilitation
Acute phase. Ice and phonophoresis are applied locally to reduce inflammation. Activity
modification is critical. Running and any other potentially exacerbating activity such as cycling
should be avoided to reduce the repetitive mechanical stress at the lateral femoral condyle.
Swimming (using only the arms) with a pool buoy between the legs is usually the only activity
permitted during the acute phase. Oral nonsteroidal anti-inflammatory medications may also
help reduce pain and inflammation. If grossly visible swelling in the area does not subside after
3 days of treatment, a local corticosteroid injection is indicated. Ice and phonophoresis are
continued after injection.
Subacute phase. Stretching exercises are started after acute inflammation subsides. Contractrelax exercises to lengthen shortened muscle groups are performed in three bouts of a 7-second
submaximal contraction followed by a 15-second stretch. Particular attention is given to
increasing the length of the ITB (figures 5 through 8). Stretching is indicated for the iliopsoas,
rectus femoris, and gastrocnemius-soleus muscles when restrictions are noted on physical
exam. Patients perform the stretches three times daily, focusing on the muscles that are
excessively tight.
Myofascial restrictions are also addressed once acute inflammation has subsided. Identifying
and eliminating these myofascial components complements physical therapy and should
precede strengthening and muscle re-education. Soft-tissue treatment usually eliminates a
significant part of the pain pattern and allows definitive and more successful treatment of ITBS.
Central trigger points of the gluteus minimus and vastus lateralis muscle: Compression,
deep stripping massage, specific stretches, and heat can release central trigger points
and associated contracture.
Attachment trigger points in the musculotendinous junction of the distal vastus lateralis
and biceps femoris muscles: Compression and deep massage is indicated, followed by
icing at the trigger points.
Contracture of the vastus lateralis muscle: Deep-tissue massage, self massage using a
foam roll, and deep stretching of the vastus lateralis reduce tension and are valuable for
prevention and therapy.
Fascial adhesions in the posterior ITB: In some cases, longitudinal stripping of an
adhesion can eliminate the pain pattern in 1 week (three treatments).
Patients can be referred to a physical therapist or deep-tissue massage therapist. Not all
therapists have the necessary manual skills and experience; successful soft-tissue treatment for
ITBS requires an understanding of the pain referral patterns involved and exceptional manual
control as high palpation pressure is applied. Recommendations from other physicians or from
coaches and athletes who have effectively used such treatments offer the best chance for
locating a skilled therapist.
Strengthening phase. Strength exercises begin once range-of-motion and myofascial
restrictions are resolved. The initial exercise is side-lying leg lifts to help the patient learn to
isolate the gluteus medius muscle (figure 9). For all strength exercises, patients start with one
set of 20 repetitions and build up to three sets of 20 repetitions daily.
Because training is specific to limb position, it is essential that patients progress to weightbearing exercise. Initially, patients are asked to stand in front of a full-length mirror and
perform a step-down exercise (figure 10). Once this is mastered, patients are taught to perform
the pelvic drop exercise (figure 11).
Return-to-running phase. Return to running depends on the severity and chronicity of the
condition and the patient's premorbid function. Most patients fully recover by 6 weeks. As a
general rule, patients can return to running once they can perform all strength exercises
without pain. We recommend running every other day for the first week, starting with easy
sprints on level ground. Biomechanical studies (7) have shown that faster-paced running is less
likely to aggravate ITBS because at foot strike the knee is flexed beyond the angles that cause
friction. Over the next 3 to 4 weeks, gradual increases in distance and frequency are permitted.
Surgical management. Various surgical techniques are performed to decrease impingement of
the ITB on the lateral femoral condyle. The most common procedure is releasing the posterior 2
cm of the ITB at the lateral condyle where it appears to create the most tension over the
femoral condyle (1,20). We have never had to refer one of our patients for surgery, and
attribute this to the success of our aggressive rehabilitation program.
Roadmap to Success
The algorithm approach for the treatment of ITBS has proven highly successful at our sports
medicine clinic. The keys to success for the more resistant cases are myofascial therapy after
acute inflammation has been addressed and progression to weight-bearing strengthening
exercises, with particular attention to the gluteus medius muscle, before return to running.
References
1. Barber FA, Sutker AN: Iliotibial band syndrome. Sports Med 1992;14(2):144-148
2. Clement DB, Taunton JE, Smart GW, et al: A survey of overuse running injuries. Phys
Sportsmed 1981;9(5):47-58
3. Linderburg G, Pinshaw R, Noakes TD: Iliotibial band syndrome in runners. Phys
Sportsmed 1984;12(5):118-130
4. Noble CA: Iliotibial band friction syndrome in runners. Am J Sports Med 1980;8(4):232234
5. Evans P: The postural function of the iliotibial tract. Ann R Coll Surg Engl
1979;61(4):272-280
6. Terry GC, Hughston JC, Norwood LA: The anatomy of the iliopatellar band and the
iliotibia tract. Am J Sports Med 1986;14(1):39-45
7. Orchard JW, Fricker PA, Abud AT, et al: Biomechanics of iliotibial band friction syndrome
in runners. Am J Sports Med 1996;24(3):375-379
8. Nishimura G, Yamato M, Tamai K, et al: MR findings in iliotibial band syndrome. Skeletal
Radiol 1997;26(9):533-537
9. Nemeth WC, Sanders BL: The lateral synovial recess of the knee: anatomy and role in
chronic iliotibial band friction syndrome. Arthroscopy 1996;12(5):574-580
10. Ekman EF, Pope T, Martin DF, et al: Magnetic resonance imaging of iliotibial band
syndrome. Am J Sports Med 1994;22(6):851-854
11. Messier SP, Edwards DG, Martin DF, et al: Etiology of iliotibial band friction syndrome in
distance runners. Med Sci Sports Exer 1995;27(7):951-960
12. James SL: Running injuries to the knee. J Am Acad Orthop Surg 1995;3(6):309-318
13. Schwellnus MP: Lower limb biomechanics in runners with the iliotibial band friction
syndrome, abstracted. Med Sci Sports Exerc 1993;25(5):S68
14. Fredericson M, Dowdell BC, Oestreicher N, et al: Correlation between decreased
strength in hip abductors and iliotibial band syndrome in runners, abstracted. Arch Phys
Med Rehabil 1997;78(9):1031
15. Mann RA, Moran GT, Dougherty SE: Comparative electromyography of the lower
extremity in jogging, running, and sprinting. Am J Sports Med 1986;14(6):501-510
16. Hollinshead WH, Jenkins DB: Functional Anatomy of the Limbs and Back, ed 5.
Philadelphia, WB Saunders, 1982, p 265
17. Simons DG, Travell JG, Simons LS: Travell & Simons' Myofascial Pain and Dysfunction:
The Trigger Point Manual, ed 2. Baltimore, Williams & Wilkins, 1999
18. Kendall FP, McCreary EK, Provance PG: Muscles: Testing and Function, ed 4. Baltimore,
Williams & Wilkins, 1993
19. Janda V: Muscle Function Testing. London, Butterworths, 1983
20. Martens M, Libbrecht P, Burssens A: Surgical treatment of iliotibial band friction
syndrome. Am J Sports Med 1989;17(5):651-654
Dr Fredericson is team physician for cross-country and track teams and is assistant professor in
the Division of Physical Medicine and Rehabilitation, Department of Functional Restoration, and
Mr Guillet is director of rehabilitation in the sports medicine program, both at Stanford
University in Stanford, California. Mr DeBenedictis is director of the Stanford Myofascial Institute
in Palo Alto, California. Address correspondence to Michael Fredericson, MD, Stanford University
Medical Center, Department of Functional Restoration, Division of Physical Medicine and
Rehabilitation, 300 Pasteur Dr, R-107B, Stanford, CA 94305.
RETURN TO FEBRUARY 2000 TABLE OF CONTENTS
HOME |
JOURNAL | PERSONAL HEALTH | RESOURCE CENTER |
ADVERTISER SERVICES | ABOUT US
Copyright (C) 2000. The McGraw-Hill Companies. All Rights Reserved
Privacy Policy. Privacy Notice.
CME |