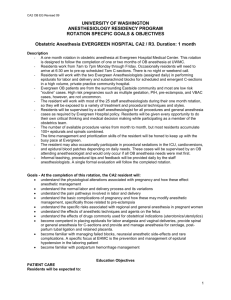
Obstetric Anesthesia (CA 2)
advertisement

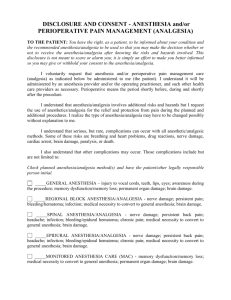
OBSTETRIC ANESTHESIA GOALS AND OBJECTIVES CA 2 Level DEFINITION Obstetrical Anesthesia is a 4 week required rotation for CA-2 anesthesia residents, which includes all types of anesthesia for Obstetrics. CURRICULUM All residents rotating through the service are expected to gain an understanding of basic principles of both clinical and cognitive management of peripartum anesthetic needs. Development of competence in pre-anesthetic assessment and planning, intra-partum management, rational responses to and prevention of complications and post-anesthetic care appropriate to the parturient in a community or tertiary care hospital are expected. MEDICAL KNOWLEDGE At the conclusion of this rotation, the resident should be able to: 1. Describe the physiologic changes of normal pregnancy. 2. List advantages and disadvantages of analgesic methods for labor including epidural, combined spinal-epidural, inhalational, pudendal and parenteral opioids. 3. Discuss anesthesia and post-operative analgesia for cesarean delivery including epidural, spinal, general, and combined spinal-epidural. 4. Discuss the pharmacokinetics and pharmacodynamics of neuraxial opioids. 5. Discuss the pharmacodynamics of common non-anesthesia medications used in obstetrics and their interactions with anesthetics, including oxytocin preparations, methylergonovine, prostaglandins, magnesium, terbutaline, nitroglycerine, indomethacin, and steroids. 6. Discuss pharmacokinetics and pharmacodynamics of local anesthetics including toxicity issues and rationale for use for a wide range of clinical conditions. 7. Describe basic fetal monitoring, including fetal heart rate monitoring. 8. Develop a differential diagnosis and describe risk factors and management for obstetric hemorrhage in the peripartum period. 9. Recognize and describe the pathophysiology of hypertensive disorders of pregnancy including management of preeclampsia/HELLP/eclampsia. 10. Identify and discuss analgesia/anesthesia for patients with thrombophilias (e.g., Factor V Leiden mutation, anti-cardiolipin antibody syndrome). 11. Discuss analgesic/anesthetic options for patients receiving anticoagulants. 12. Discuss obesity in pregnancy, including its pathophysiology, and the management of the parturient. 13. Recognize and describe the evaluation and management of patients with thrombocytopenia. 14. Describe the management of patients who plan vaginal birth after cesarean (VBAC) delivery. 15. Identify possible causes of postpartum headache including the diagnosis and the management of post-dural puncture headache. 16. Identify and discuss the management of neurologic complications associated with labor and delivery. 17. Identify and discuss the management of failed regional anesthetic for cesarean delivery. PATIENT CARE At the conclusion of this rotation, the resident should be able to: 1. Identify parturients who will benefit from anesthesia evaluation during labor. 2. Correctly identify analgesia options for labor. 3. Place a lumbar epidural catheter for analgesia with minimal assistance in 70-80% of cases. 4. Correctly connect an epidural catheter to an infusion pump and provide continuous analgesia. 5. Prepare an obstetric operating room for emergency cesarean delivery. 6. Place a subarachnoid block with minimal assistance for elective or repeat cesarean delivery in 70-80% of cases. 7. Perform rapid sequence induction with faculty assistance for maternal/fetal emergency. 8. Provide analgesia/anesthesia for removal of retained placental fragments with faculty assistance. 9. Correctly recognize and respond to unplanned dural puncture during epidural placement. 10. Diagnose post-dural puncture headache (PDPH). 11. Prescribe conservative management for PDPH. 12. Perform (or describe how to perform) an epidural blood patch with faculty assistance for PDPH. 13. Provide anesthesia for cervical cerclage. 14. Provide anesthesia for an assisted second stage vaginal delivery. 15. Provide anesthesia for post-partum tubal ligation. 16. Recognize and respond to obstetric hemorrhage. 17. Provide analgesia / anesthesia for an external cephalic version, based on the patient’s need for delivery following the procedure. INTERPERSONAL AND COMMUNICATION SKILLS At the conclusion of the rotation the resident will: 1. Be able to form a rational plan for analgesia in a patient with painful labor, communicate that plan to the patient and obtain informed consent. 2. Inform the obstetric staff of any changes in maternal/fetal condition (e.g. hypotension) that occur during anesthesia care. 3. Cooperate with the obstetric nursing team and obstetric providers (obstetricians, family practitioners, nurse midwives) to assure patient satisfaction. 4. Obtain informed consent for cesarean delivery. 2 PROFESSIONALISM At the conclusion of this rotation, the resident must: 1. Adhere to procedures designed for maternal privacy and security of the newborn. 2. Demonstrate the ability to achieve pain relief in a parturient with severe pain. 3. Communicate with all levels of professionals working to provide obstetric care, including physicians, midwives, and RNs. 4. Confirm effective analgesia after cesarean delivery SYSTEMS-BASED PRACTICE At the conclusion of this rotation, the resident must: 1. Be able to participate in daily morning report and weekly Team Meeting where systems issues on L&D are discussed with nursing and obstetric care providers (MD and CNM). 2. Participate in care conferences on high risk patients in preparation for their delivery. 3. Participate in at least one postpartum hemorrhage simulation with the nursing and OB services for team training. 4. Attend High Risk OB clinic once a week to interact on patients who may need specialized anesthesia services at delivery. Rev. 7/2009 3