PREOPERATIVE DIAGNOSIS: Williams syndrome
advertisement
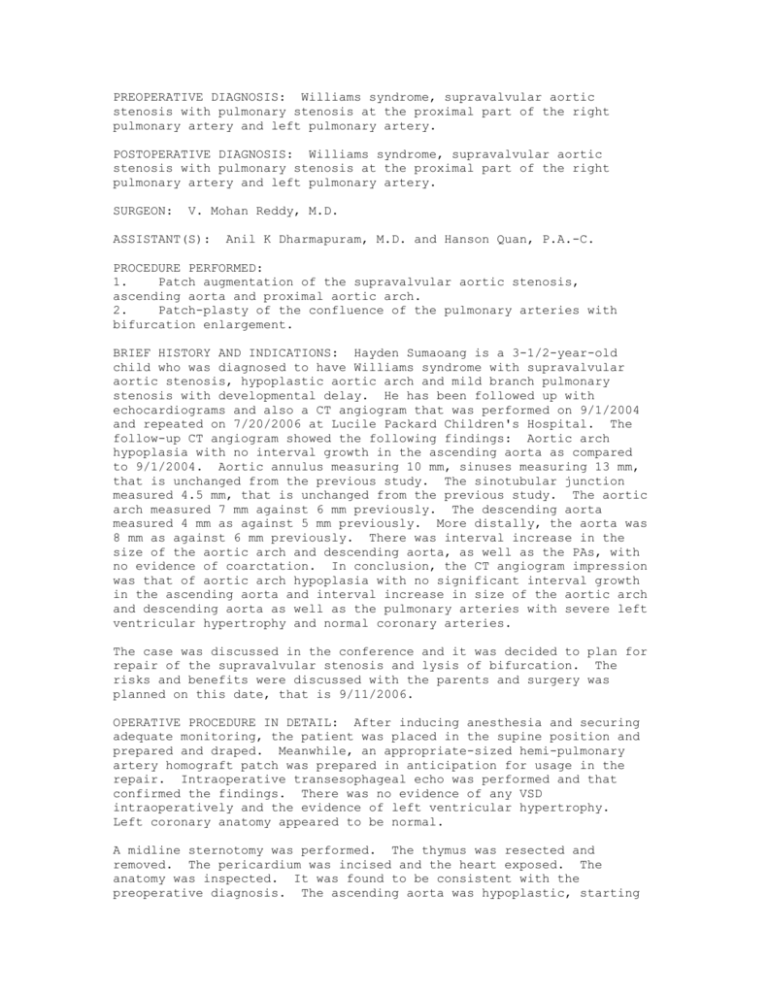
PREOPERATIVE DIAGNOSIS: Williams syndrome, supravalvular aortic stenosis with pulmonary stenosis at the proximal part of the right pulmonary artery and left pulmonary artery. POSTOPERATIVE DIAGNOSIS: Williams syndrome, supravalvular aortic stenosis with pulmonary stenosis at the proximal part of the right pulmonary artery and left pulmonary artery. SURGEON: V. Mohan Reddy, M.D. ASSISTANT(S): Anil K Dharmapuram, M.D. and Hanson Quan, P.A.-C. PROCEDURE PERFORMED: 1. Patch augmentation of the supravalvular aortic stenosis, ascending aorta and proximal aortic arch. 2. Patch-plasty of the confluence of the pulmonary arteries with bifurcation enlargement. BRIEF HISTORY AND INDICATIONS: Hayden Sumaoang is a 3-1/2-year-old child who was diagnosed to have Williams syndrome with supravalvular aortic stenosis, hypoplastic aortic arch and mild branch pulmonary stenosis with developmental delay. He has been followed up with echocardiograms and also a CT angiogram that was performed on 9/1/2004 and repeated on 7/20/2006 at Lucile Packard Children's Hospital. The follow-up CT angiogram showed the following findings: Aortic arch hypoplasia with no interval growth in the ascending aorta as compared to 9/1/2004. Aortic annulus measuring 10 mm, sinuses measuring 13 mm, that is unchanged from the previous study. The sinotubular junction measured 4.5 mm, that is unchanged from the previous study. The aortic arch measured 7 mm against 6 mm previously. The descending aorta measured 4 mm as against 5 mm previously. More distally, the aorta was 8 mm as against 6 mm previously. There was interval increase in the size of the aortic arch and descending aorta, as well as the PAs, with no evidence of coarctation. In conclusion, the CT angiogram impression was that of aortic arch hypoplasia with no significant interval growth in the ascending aorta and interval increase in size of the aortic arch and descending aorta as well as the pulmonary arteries with severe left ventricular hypertrophy and normal coronary arteries. The case was discussed in the conference and it was decided to plan for repair of the supravalvular stenosis and lysis of bifurcation. The risks and benefits were discussed with the parents and surgery was planned on this date, that is 9/11/2006. OPERATIVE PROCEDURE IN DETAIL: After inducing anesthesia and securing adequate monitoring, the patient was placed in the supine position and prepared and draped. Meanwhile, an appropriate-sized hemi-pulmonary artery homograft patch was prepared in anticipation for usage in the repair. Intraoperative transesophageal echo was performed and that confirmed the findings. There was no evidence of any VSD intraoperatively and the evidence of left ventricular hypertrophy. Left coronary anatomy appeared to be normal. A midline sternotomy was performed. The thymus was resected and removed. The pericardium was incised and the heart exposed. The anatomy was inspected. It was found to be consistent with the preoperative diagnosis. The ascending aorta was hypoplastic, starting from just above the annulus at the sinotubular junction and involving the entire ascending aorta and entire arch and extending onto the peripheral part of the descending aorta. The ascending appeared thickened. The bifurcation of the pulmonary arteries appeared narrow. The pulmonary arteries, on inspection, appeared to be normal from outside. In the beginning, a dissection was performed to separate the ascending aorta and the pulmonary arteries. The PDA appeared to be ligamentous. It was isolated, it was looped with 5-0 Prolene transfixation suture and tied and clipped at the aortic end. The pulmonary artery end of the ductus was also sutured with a transfixation suture and the PDA divided in between the two sutures. The entire ascending aorta was dissected including the neck vessels and the arch and the peripheral part of the descending aorta. The pulmonary arteries were also dissected to expose the bifurcation. Meanwhile, preparations were made for installation to the cardiopulmonary bypass. It was decided to perform double aortic cannulation, that is to cannulate both the innominate and proximal part of the descending aorta with two separate aortic cannulae. So pursestrings were placed, one in the base of the innominate artery and another in the proximal part of the descending aorta. #10 arterial cannula was used to cannulate the proximal part of the descending aorta and the innominate separately. Both of these cannulae were connected to a Y-connector and then connected to the arterial end of the CPB. The SVC and IVC were cannulated with two angled venous cannulae. Cardiopulmonary bypass was established and slow cooling was started to achieve cooling of temperature to 32 degrees centigrade. A vent was placed in the right pulmonary vein into the LV. A pursestring suture was placed in the descending aorta just proximal to the innominate artery for placement of cardioplegia and that was connected to the cardioplegia system. At the desired temperature, the aorta was cross clamped just distal to the cardioplegia cannula and proximal to the innominate cannula to include the aorta and arch. The aortic root was cooled and cardioplegia infused. Surface cooling was done with ice cold saline. After establishment of cardiac asystole, the aortic root cardioplegic cannula was removed and the cardioplegia cannula incision was enlarged with a fine scissor. The aorta was incised both proximally and distally starting from the incision of the cardioplegia cannula. Proximally, it was incised towards the aortic valve, passing across the sinotubular junction. At this level, the incision was carried down both ways into the sinuses of the right coronary artery and beyond the coronary artery to completely open the aorta that was narrow at this level of the sinotubular junction. Following this, the coronary arteries were inspected and found to be normal at the level of the ostia; however, there was a ridge of tissue above the level of the left coronary artery ostium that was removed completely. Following this, both ostia of the coronary artery were inspected and found to be adequate with no evidence of any obstruction as evaluated by passing of fine probes of appropriate size. Distally, the incision of the aorta was continued onto the undersurface of the aortic arch and extended almost towards the undersurface of the aortic arch. Meanwhile, the already prepared pulmonary homograft patch was appropriately incised and shaped into a longitudinal piece with two separate ends at the proximal ends that would separately fit into both enlarged sinuses of the NCC and the RCC. The patch was appropriately trimmed to match the shape of the undersurface of the aortic arch after being sutured. Augmentation of the entire ascending aorta and arch was performed with the patch using 5-0 Prolene continuous suture. The suturing was first started at the bases of the sinuses separately and then continued distally. After 25 minutes, the cardioplegia was repeated by infusing cold crystalloid cardioplegia into both the coronary arteries separately. Following this the distal augmentation was continued towards the undersurface of the arch. At this level distally, the incision was posited towards the arch on the under surface of the aorta to extend to the proximal part of the aortic arch. To the most distal ends of the anastomosis, the aortic cross-clamp was replaced with a side-biting Cclamp that was placed to include the base of the neck vessels onto the undersurface of the aortic arch and well above the aortic cannula that was placed in the descending aorta. After placing the C-clamp, adequate exposure was obtained to extend the anastomosis of the augmentation well onto the undersurface of the aortic arch and the proximal part of the descending aorta. After completion of the augmentation of the aorta with this patch, a stab suture incision was made with a pursestring on the top of the aorta and de-airing was performed by stopping the vent. Meanwhile, rewarming was started. After adequate de-airing of the aorta, the aortic cross-clamp, that is the side-biting clamp, was slowly released and the aortic root adequately de-aired. After releasing the aortic cross-clamp, the vent was restored. The heart started beating with normal contraction of the ventricle. Rewarming was continued to normothermia. The aortic root vent was snugged. On the beating heart, the augmentation of the pulmonary artery bifurcation was planned. It was done as follows. Two stay sutures were placed, one proximal and one distal at the level of the bifurcation and the MPA was incised longitudinally. It was extended proximally towards the pulmonary valve and distally towards the bifurcation. At the level of the bifurcation, it was noticed that both RPA and LPA origins were narrow due to another bifurcation. A plasty was performed by cutting onto the bifurcation to include both the ostia of the RPA and LPA. After initially opening the bifurcation, suturing was performed into the slightly opened bifurcation using 7-0 Prolene. The suturing was started at the apex of the incision, that is towards the opening of both ostia, and posited upwards, that is toward the bifurcation. By doing so, the entire bifurcation was adequately enlarged and both origins of the RPA and LPA appeared adequate and opened up adequately. After enlarging the bifurcation posteriorly, the anterior part of the MPA was augmented with separate piece of homograft patch that was appropriately prepared and then sutured using 6-0 Prolene continuous suture. The entire augmentation was performed on a beating heart. At this junction, rewarming was completed. Preparations were made to wean the patient off cardiopulmonary bypass. At first, the anastomotic areas were evaluated for bleeding and hemostasis was obtained by appropriate suturing. The LV vent was stopped and the vent removed. The heart was gradually weaned off bypass with moderate inotropic support of 3 mcg of dopamine and 1 mcg of milrinone. To control hypertension, Nipride was used. The hemodynamics appeared to be stable with satisfactory saturations. The myocardial contractions appeared to be normal. The entire ascending aorta and arch filled normally with good contour. Intraoperative transesophageal echo was performed. It showed evidence of good repair with no evidence of obstruction at the level of the aorta and the pulmonary arteries. The LV function appeared to be normal. After assuring adequate hemostasis, protamine was administered and decannulation performed. Hemostasis was checked carefully. The right pleura was opened and the pleural cavity drained with separate chest tube. The mediastinum was drained with a #20 chest tube separately. Two ventricular pacing wires were placed. With adequate hemostasis, the chest was closed with sternal wires and the subcutaneous layers and skin were closed appropriately. The patient was shifted with stable hemodynamics and saturations and with adequate control of hypertension to the CV ICU.